Bias in observational studies on the effectiveness of in hospital use of hydroxychloroquine in COVID-19
et al., Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.5632, Apr 2023
HCQ for COVID-19
1st treatment shown to reduce risk in
March 2020, now with p < 0.00000000001 from 424 studies, used in 59 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
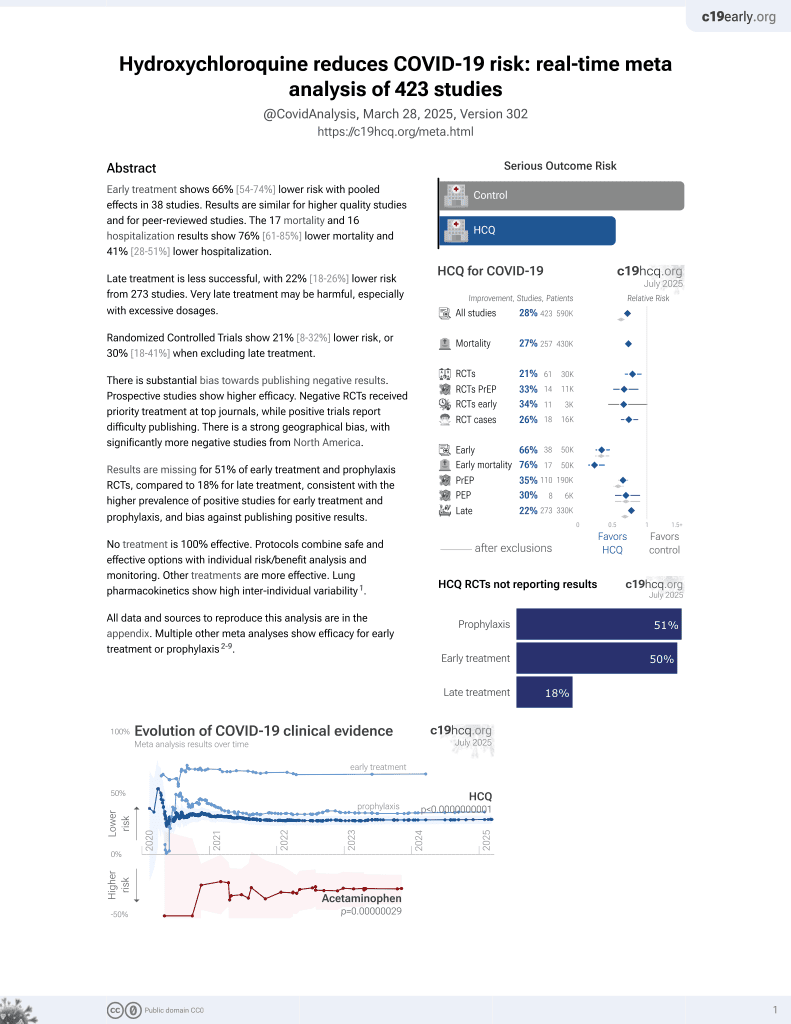
Analysis of 33 observational studies for HCQ, showing wide variation in the risk of bias according to ROBINS-I assessments.
10 meta-analyses show significant improvements with hydroxychloroquine for mortality1-4,
hospitalization1,
recovery5,
combined death/hospitalization/cases6,
cases7-9, and
viral clearance10.
Currently there are 38 HCQ for COVID-19 early treatment studies, showing 76% lower mortality [61‑85%], 67% lower ventilation [-710‑99%], 31% lower ICU admission [1‑53%], and 41% lower hospitalization [28‑51%].
1.
Landsteiner de Sampaio Amêndola et al., COVID-19 Infection in Rheumatic Patients on Chronic Antimalarial Drugs: A Systematic Review and Meta-Analysis, Journal of Clinical Medicine, doi:10.3390/jcm11226865.
2.
Risch, H., Early Outpatient Treatment of Symptomatic, High-Risk Covid-19 Patients that Should be Ramped-Up Immediately as Key to the Pandemic Crisis, American Journal of Epidemiology, kwaa093, 27 May 2020, doi:10.1093/aje/kwaa093.
3.
Risch (B), H., Response to: “Early Outpatient Treatment of Symptomatic, High-Risk Covid-19 Patients” and “Re: Early Outpatient Treatment of Symptomatic, High-Risk Covid-19 Patients that Should be Ramped-Up Immediately as Key to the Pandemic Crisis”, American Journal of Epidemiology, July 20, 2020, doi:10.1093/aje/kwaa152.
4.
Stricker et al., Hydroxychloroquine Pre-Exposure Prophylaxis for COVID-19 in Healthcare Workers from India: A Meta-Analysis, Journal of Infection and Public Health, doi:10.1016/j.jiph.2021.08.001.
5.
Prodromos et al., Hydroxychloroquine is effective, and consistently so used early, for Covid-19: A systematic review, New Microbes and New Infections, doi:10.1016/j.nmni.2020.100776.
6.
Ladapo et al., Randomized Controlled Trials of Early Ambulatory Hydroxychloroquine in the Prevention of COVID-19 Infection, Hospitalization, and Death: Meta-Analysis, medRxiv, doi:10.1101/2020.09.30.20204693.
7.
García-Albéniz et al., Systematic review and meta-analysis of randomized trials of hydroxychloroquine for the prevention of COVID-19, European Journal of Epidemiology, doi:10.1007/s10654-022-00891-4.
8.
Han et al., The efficacy and safety of hydroxychloroquine for COVID-19 prophylaxis and clinical assessment: an updated meta-analysis of randomized trials, Journal of Thoracic Disease, doi:10.21037/jtd-23-1043.
Hempenius et al., 24 Apr 2023, Netherlands, peer-reviewed, 6 authors.
Contact: h.gardarsdottir@uu.nl.
Bias in observational studies on the effectiveness of in hospital use of hydroxychloroquine in COVID‐19
Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.5632
Purpose: During the first waves of the coronavirus pandemic, evidence on potential effective treatments was urgently needed. Results from observational studies on the effectiveness of hydroxychloroquine (HCQ) were conflicting, potentially due to biases. We aimed to assess the quality of observational studies on HCQ and its relation to effect sizes. Methods: PubMed was searched on 15 March 2021 for observational studies on the effectiveness of in-hospital use of HCQ in COVID-19 patients, published between 01/01/2020 and 01/03/2021 on. Study quality was assessed using the ROBINS-I tool. Association between study quality and study characteristics (journal ranking, publication date, and time between submission and publication) and differences between effects sizes found in observational studies compared to those found in RCTs, were assessed using Spearman's correlation. Results: Eighteen of the 33 (55%) included observational studies were scored as critical risk of bias, eleven (33%) as serious risk and only four (12%) as moderate risk of bias. Biases were most often scored as critical in the domains related to selection of participants (n = 13, 39%) and bias due to confounding (n = 8, 24%). There were no significant associations found between the study quality and the characteristics nor between the study quality and the effect estimates. Discussion: Overall, the quality of observational HCQ studies was heterogeneous. Synthesis of evidence of effectiveness of HCQ in COVID-19 should focus on RCTs and carefully consider the added value and quality of observational evidence.
CONFLICT OF INTEREST STATEMENT The authors declare no conflict of interest.
ETHICS STATEMENT The authors state that no ethical approval was needed.
SUPPORTING INFORMATION Additional supporting information can be found online in the Supporting Information section at the end of this article.
References
Albani, Fusina, Giovannini, Impact of azithromycin and/or Hydroxychloroquine on hospital mortality in COVID-19, J Clin Med, doi:info:doi/10.3390/jcm9092800
Arshad, Kilgore, Chaudhry, Treatment with hydroxychloroquine, azithromycin, and combination in patients hospitalized with COVID-19, Int J Infect Dis, doi:info:doi/10.1016/j.ijid.2020.06.099
Awad, Schiller, Fulman, Chak, Impact of hydroxychloroquine on disease progression and ICU admissions in patients with SARS-CoV-2 infection, Am J Heal Pharm, doi:info:doi/10.1093/ajhp/zxab056
Catteau, Dauby, Montourcy, Low-dose hydroxychloroquine therapy and mortality in hospitalised patients with COVID-19: a nationwide observational study of 8075 participants, Int J Antimicrob Agents, doi:info:doi/10.1016/j.ijantimicag.2020.106144
Clarivate, None, InCites Journal Citation Reports
De Lucena Alves, Segundo, Da Costa, How a few poorly designed COVID-19 studies may have contributed to misinformation in Brazil: the case for evidence-based communication of science, BMJ Open Sci, doi:info:doi/10.1136/BMJOS-2021-100202
Fantini, Scala, Chahinian, Yahi, Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection, Int J Antimicrob Agents
Fiolet, Guihur, Rebeaud, Mulot, Peiffer-Smadja et al., Effect of hydroxychloroquine with or without azithromycin on the mortality of coronavirus disease 2019 (COVID-19) patients: a systematic review and meta-analysis, Clin Microbiol Infect, doi:info:doi/10.1016/j.cmi.2020.08.022
Gautret, Lagier, Parola, Clinical and microbiological effect of a combination of hydroxychloroquine and azithromycin in 80 COVID-19 patients with at least a six-day follow up: a pilot observational study, Travel Med Infect Dis, doi:info:doi/10.1016/j.tmaid.2020.101663
Hempenius, Luijken, De Boer, Klungel, Groenwold et al., Quality of reporting of drug exposure in pharmacoepidemiological studies, Pharmacoepidemiol Drug Saf, doi:info:doi/10.1002/pds.5020
Hernán, Sauer, Hernández-Díaz, Platt, Shrier, Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses, J Clin Epidemiol
Hernán, Using big data to emulate a target trial when a randomized trial is not available, Am J Epidemiol, doi:info:doi/10.1093/AJE/KWV254
Hunt, Gardarsdottir, Bazelier, Klungel, Pajouheshnia, A systematic review of how missing data are handled and reported in multi-database pharmacoepidemiologic studies, Pharmacoepidemiol Drug Saf, doi:info:doi/10.1002/pds.5245
Ispe, Guidelines for good pharmacoepidemiology practices (GPP), Pharmacoepidemiol Drug Saf, doi:info:doi/10.1002/pds.1471
Kim, Sparks, Liew, A rush to judgment? Rapid reporting and dissemination of results and its consequences regarding the use of Hydroxychloroquine for COVID-19, Ann Intern Med, doi:info:doi/10.7326/M20-1223
Lagier, Million, Gautret, Outcomes of 3,737 COVID-19 patients treated with hydroxychloroquine/azithromycin and other regimens in Marseille, France: a retrospective analysis, Travel Med Infect Dis, doi:info:doi/10.1016/j.tmaid.2020.101791
Langan, Schmidt, Wing, The reporting of studies conducted using observational routinely collected health data statement for pharmacoepidemiology (RECORD-PE), BMJ, doi:info:doi/10.1136/bmj.k3532
Lauriola, Pani, Ippoliti, Effect of combination therapy of Hydroxychloroquine and azithromycin on mortality in patients with COVID-19, Clin Transl Sci, doi:info:doi/10.1111/cts.12860
Lee, Mackenzie, Mcdonald, Tong, An observational cohort study of hydroxychloroquine and azithromycin for COVID-19: (Can't Get No) satisfaction, Int J Infect Dis, doi:info:doi/10.1016/j.ijid.2020.06.095
Martinuka, Von Cube, Wolkewitz, Methodological evaluation of bias in observational coronavirus disease 2019 studies on drug effectiveness, Clin Microbiol Infect, doi:info:doi/10.1016/j.cmi.2021.03.003
Mcguinness, Higgins, Risk-of-bias VISualization (robvis): an R package and shiny web app for visualizing risk-of-bias assessments, Res Synth Methods, doi:info:doi/10.1002/jrsm.1411
Medicines, The European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP) Guide on Methodological Standards in Pharmacoepidemiology, 9th Revision
Pan, Peto, Karim, Repurposed antiviral drugs for COVID-19interim WHO solidarity trial results, N Engl J Med, doi:info:doi/10.1056/nejmoa2023184
Peters, Collard, Van Assen, Outcomes of persons with coronavirus disease 2019 in hospitals with and without standard treatment with (hydroxy)chloroquine, Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis, doi:info:doi/10.1016/j.cmi.2020.10.004
Pottegård, Kurz, Moore, Christiansen, Klungel, Considerations for pharmacoepidemiological analyses in the SARS-CoV-2 pandemic, Pharmacoepidemiol Drug Saf, doi:info:doi/10.1002/pds.5029
Renoux, Azoulay, Suissa, Biases in evaluating the safety and effectiveness of drugs for COVID-19: designing real-world evidence studies, Am J Epidemiol, doi:info:doi/10.1093/aje/kwab028
Rosenberg, Dufort, Udo, Association of Treatment with Hydroxychloroquine or azithromycin with In-hospital mortality in patients with COVID-19 in New York state, JAMA, doi:info:doi/10.1001/jama.2020.8630
Rubin, Harrington, Hogan, Gatsonis, Baden et al., The urgency of care during the COVID-19 pandemiclearning as we go, N Engl J Med, doi:info:doi/10.1056/nejme2015903
Self, Semler, Leither, Effect of hydroxychloroquine on clinical status at 14 days in hospitalized patients with COVID-19: a randomized clinical trial, JAMA, doi:info:doi/10.1001/jama.2020.22240
Siemieniuk, Bartoszko, Ge, Drug treatments for COVID-19: living systematic review and network meta-analysis, BMJ, doi:info:doi/10.1136/bmj.m2980
Sterne, Hernán, Reeves, ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions, BMJ, doi:info:doi/10.1136/bmj.i4919
Su, Ling, Ma, Efficacy of early hydroxychloroquine treatment in preventing COVID-19 pneumonia aggravation, the experience from Shanghai, China, Biosci Trends, doi:info:doi/10.5582/bst.2020.03340
Suissa, Dell'aniello, Time-related biases in pharmacoepidemiology, Pharmacoepidemiol Drug Saf, doi:10.1002/pds.5083
Velentgas, Dreyer, Nourjah, Smith, Torchia, Developing a Protocol for Observational Comparative Effectiveness Research: A User's Guide
Wang, Schneeweiss, Assessing and interpreting real-world evidence studies: introductory points for new reviewers, Clin Pharmacol Ther, doi:info:doi/10.1002/CPT.2398
Wolkewitz, Schumacher, Survival biases lead to flawed conclusions in observational treatment studies of influenza patients, J Clin Epidemiol, doi:info:doi/10.1016/J.JCLINEPI.2017.01.008
DOI record:
{
"DOI": "10.1002/pds.5632",
"ISSN": [
"1053-8569",
"1099-1557"
],
"URL": "http://dx.doi.org/10.1002/pds.5632",
"abstract": "<jats:title>Abstract</jats:title><jats:sec><jats:title>Purpose</jats:title><jats:p>During the first waves of the coronavirus pandemic, evidence on potential effective treatments was urgently needed. Results from observational studies on the effectiveness of hydroxychloroquine (HCQ) were conflicting, potentially due to biases. We aimed to assess the quality of observational studies on HCQ and its relation to effect sizes.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>PubMed was searched on 15 March 2021 for observational studies on the effectiveness of in‐hospital use of HCQ in COVID‐19 patients, published between 01/01/2020 and 01/03/2021 on. Study quality was assessed using the ROBINS‐I tool. Association between study quality and study characteristics (journal ranking, publication date, and time between submission and publication) and differences between effects sizes found in observational studies compared to those found in RCTs, were assessed using Spearman's correlation.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Eighteen of the 33 (55%) included observational studies were scored as critical risk of bias, eleven (33%) as serious risk and only four (12%) as moderate risk of bias. Biases were most often scored as critical in the domains related to selection of participants (<jats:italic>n</jats:italic> = 13, 39%) and bias due to confounding (<jats:italic>n</jats:italic> = 8, 24%). There were no significant associations found between the study quality and the characteristics nor between the study quality and the effect estimates.</jats:p></jats:sec><jats:sec><jats:title>Discussion</jats:title><jats:p>Overall, the quality of observational HCQ studies was heterogeneous. Synthesis of evidence of effectiveness of HCQ in COVID‐19 should focus on RCTs and carefully consider the added value and quality of observational evidence.</jats:p></jats:sec>",
"alternative-id": [
"10.1002/pds.5632"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2022-06-10"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2023-04-14"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2023-04-24"
}
],
"author": [
{
"ORCID": "https://orcid.org/0000-0003-0223-4815",
"affiliation": [
{
"name": "Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences Utrecht University Utrecht The Netherlands"
}
],
"authenticated-orcid": false,
"family": "Hempenius",
"given": "Mirjam",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences Utrecht University Utrecht The Netherlands"
}
],
"family": "Bots",
"given": "Sophie H.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Clinical Epidemiology Leiden University Medical Center Leiden The Netherlands"
}
],
"family": "Groenwold",
"given": "Rolf H. H.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences Utrecht University Utrecht The Netherlands"
}
],
"family": "de Boer",
"given": "Anthonius",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences Utrecht University Utrecht The Netherlands"
},
{
"name": "Julius Center for Health Sciences and Primary Care University Medical Center Utrecht Utrecht The Netherlands"
}
],
"family": "Klungel",
"given": "Olaf H.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences Utrecht University Utrecht The Netherlands"
},
{
"name": "Department of Clinical Pharmacy, Division Laboratory and Pharmacy University Medical Center Utrecht Utrecht The Netherlands"
},
{
"name": "Faculty of Pharmaceutical Sciences University of Iceland Reykjavik Iceland"
}
],
"family": "Gardarsdottir",
"given": "Helga",
"sequence": "additional"
}
],
"container-title": "Pharmacoepidemiology and Drug Safety",
"container-title-short": "Pharmacoepidemiology and Drug",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2023,
4,
18
]
],
"date-time": "2023-04-18T12:09:42Z",
"timestamp": 1681819782000
},
"deposited": {
"date-parts": [
[
2023,
8,
18
]
],
"date-time": "2023-08-18T06:09:42Z",
"timestamp": 1692338982000
},
"indexed": {
"date-parts": [
[
2025,
6,
4
]
],
"date-time": "2025-06-04T04:23:20Z",
"timestamp": 1749011000430,
"version": "3.40.5"
},
"is-referenced-by-count": 3,
"issue": "9",
"issued": {
"date-parts": [
[
2023,
4,
24
]
]
},
"journal-issue": {
"issue": "9",
"published-print": {
"date-parts": [
[
2023,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
24
]
],
"date-time": "2023-04-24T00:00:00Z",
"timestamp": 1682294400000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/pds.5632",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"page": "1001-1011",
"prefix": "10.1002",
"published": {
"date-parts": [
[
2023,
4,
24
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
24
]
]
},
"published-print": {
"date-parts": [
[
2023,
9
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1056/nejme2015903",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_2_1"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105960",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_3_1"
},
{
"DOI": "10.1016/j.tmaid.2020.101663",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_4_1"
},
{
"DOI": "10.1002/pds.5029",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_5_1"
},
{
"DOI": "10.1093/ajhp/zxab056",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_6_1"
},
{
"DOI": "10.1016/j.tmaid.2020.101791",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_7_1"
},
{
"DOI": "10.1136/BMJOS‐2021‐100202",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_8_1"
},
{
"DOI": "10.1016/j.ijid.2020.06.099",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_9_1"
},
{
"DOI": "10.1111/cts.12860",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_10_1"
},
{
"DOI": "10.1016/j.ijid.2020.06.095",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_11_1"
},
{
"DOI": "10.1056/NEJMoa2022926",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_12_1"
},
{
"DOI": "10.1056/nejmoa2023184",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_13_1"
},
{
"DOI": "10.1136/bmj.m2980",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_14_1"
},
{
"DOI": "10.7326/M20‐1223",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_15_1"
},
{
"DOI": "10.1016/j.cmi.2020.08.022",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_16_1"
},
{
"DOI": "10.1093/aje/kwab028",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_17_1"
},
{
"DOI": "10.1016/j.cmi.2021.03.003",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_18_1"
},
{
"key": "e_1_2_9_19_1",
"unstructured": "Clarivate.InCites Journal Citation Reports.2021Accessed August 4 2021.https://jcr.clarivate.com"
},
{
"DOI": "10.1136/bmj.i4919",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_20_1"
},
{
"key": "e_1_2_9_21_1",
"unstructured": "RECOVERY trial to stop enrolling patients to “ineffective” hydroxychloroquine arm – The Pharmaceutical Journal. Accessed September 28 2021.https://pharmaceutical-journal.com/article/news/recovery-trial-to-stop-enrolling-patients-to-ineffective-hydroxychloroquine-arm"
},
{
"key": "e_1_2_9_22_1",
"unstructured": "Coronavirus (COVID‐19) Update: FDA Revokes Emergency Use Authorization for Chloroquine and Hydroxychloroquine | FDA. Accessed October 6 2021.https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-revokes-emergency-use-authorization-chloroquine-and"
},
{
"DOI": "10.1016/j.cmi.2020.10.004",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_23_1"
},
{
"DOI": "10.5582/bst.2020.03340",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_24_1"
},
{
"DOI": "10.1002/pds.5083",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_25_1"
},
{
"DOI": "10.1016/J.JCLINEPI.2017.01.008",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_26_1"
},
{
"DOI": "10.1001/jama.2020.8630",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_27_1"
},
{
"DOI": "10.1016/j.ijantimicag.2020.106144",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_28_1"
},
{
"DOI": "10.3390/jcm9092800",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_29_1"
},
{
"DOI": "10.1016/j.ejim.2020.08.019",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_30_1"
},
{
"DOI": "10.1002/pds.5020",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_31_1"
},
{
"DOI": "10.1002/pds.5245",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_32_1"
},
{
"DOI": "10.1002/pds.1471",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_33_1"
},
{
"key": "e_1_2_9_34_1",
"unstructured": "European Medicines Agency.The European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP) Guide on Methodological Standards in Pharmacoepidemiology 9th Revision. Accessed August 4 2021.http://www.encepp.eu/standards_and_guidance"
},
{
"article-title": "Administration food and drug, research (CDER) Center for Drug Evaluation and, research (CBER) Center for Biologics Evaluation and Guidance for industry and FDA staff best practices for conducting and reporting pharmacoepidemiologic safety studies using electronic healthcare data",
"author": "U.S. Department of Health and Human Services",
"journal-title": "Drug Saf",
"key": "e_1_2_9_35_1",
"year": "2013"
},
{
"key": "e_1_2_9_36_1",
"unstructured": "VelentgasP DreyerNA NourjahP SmithSR TorchiaMM.Developing a Protocol for Observational Comparative Effectiveness Research: A User's Guide.2013Accessed May 3 2019.https://www.ncbi.nlm.nih.gov/books/NBK126190/"
},
{
"key": "e_1_2_9_37_1",
"unstructured": "European Medicines Agency.Guideline on Good Pharmacovigilance Practices (GVP) – Module VIII – Post‐Authorisation Safety Studies (Rev 3).2017Accessed October 31 2019.www.ema.europa.eu"
},
{
"DOI": "10.1093/AJE/KWV254",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_38_1"
},
{
"DOI": "10.1016/j.jclinepi.2016.04.014",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_39_1"
},
{
"DOI": "10.1136/bmj.k3532",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_40_1"
},
{
"DOI": "10.1002/CPT.2398",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_41_1"
},
{
"DOI": "10.1001/jama.2020.22240",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_42_1"
},
{
"DOI": "10.1002/jrsm.1411",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_43_1"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/pds.5632"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Bias in observational studies on the effectiveness of in hospital use of hydroxychloroquine in <scp>COVID</scp>‐19",
"type": "journal-article",
"update-policy": "https://doi.org/10.1002/crossmark_policy",
"volume": "32"
}