The hyaluronan receptor CD44 drives COVID-19 severity through its regulation of neutrophil migration
et al., bioRxiv, doi:10.1101/2025.10.13.682000, Oct 2025
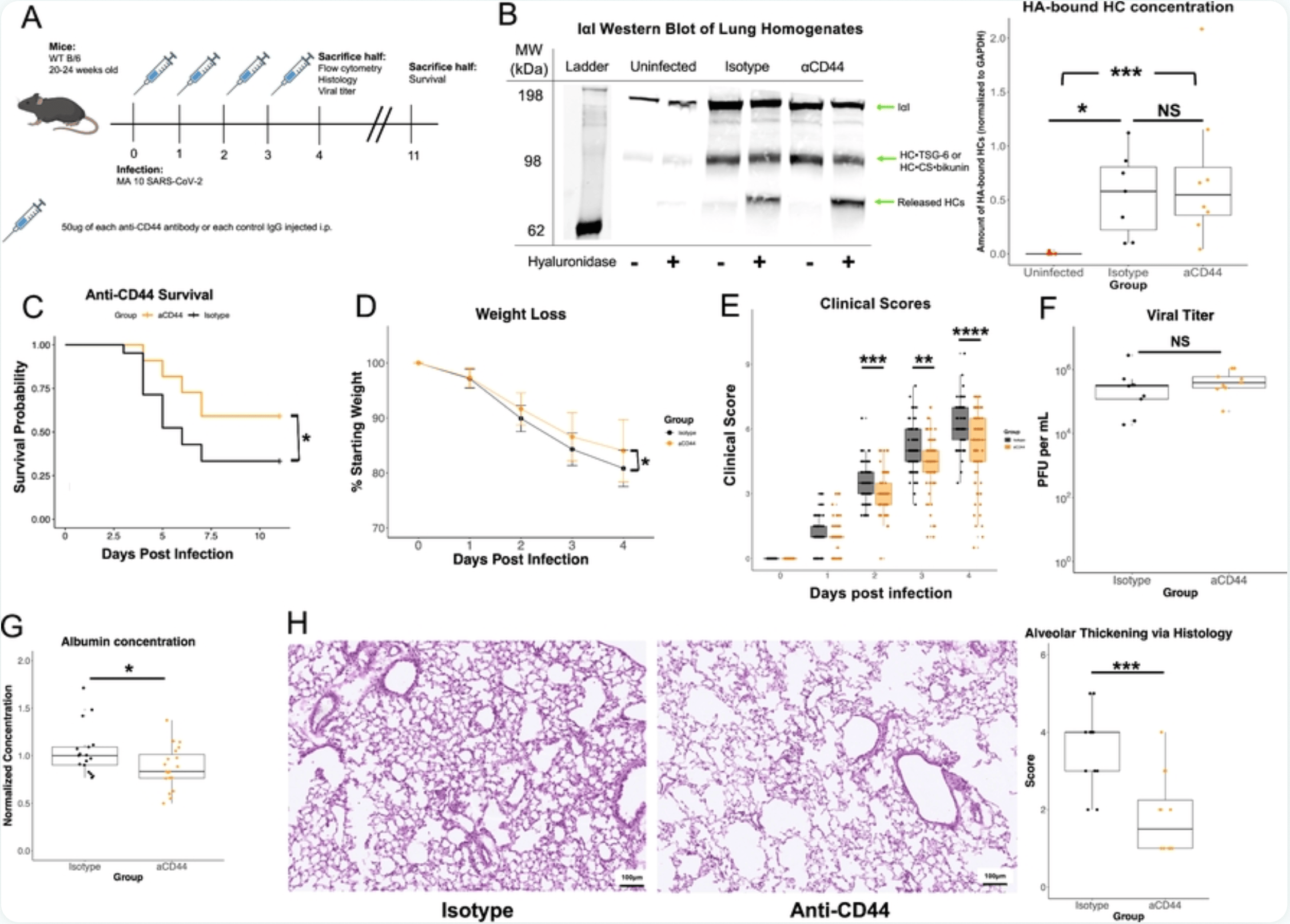
Mouse study showing benefit with anti-CD44 monoclonal antibodies (KM201 and IM7) in reducing COVID-19 severity through disruption of hyaluronan-CD44 interactions.
Hart et al., 14 Oct 2025, USA, preprint, 12 authors.
Contact: wap3g@virginia.edu.
The hyaluronan receptor CD44 drives COVID-19 severity through its regulation of neutrophil migration
doi:10.1101/2025.10.13.682000
The novel respiratory disease COVID-19 caused by the coronavirus SARS-CoV-2 continues to be a public health emergency worldwide, and there is a need for more effective therapy for patients. The relationship between the extracellular matrix and the host immune response to infection is severely understudied. Deposition of the polysaccharide hyaluronan (HA) into the lungs is associated with more severe COVID-19 disease outcomes. HA is a major component of the extracellular matrix in connective tissues and is abundant in many parts of the body, including cartilage, skin, brain, and vitreous body. CD44 is the primary receptor for HA and is found on almost all immune cells in the lung. Known functions of CD44 include mediation of immune cell migration, activation, and differentiation. We hypothesized that increased HA deposition during COVID-19 increases CD44-mediated immune cell infiltration into lungs and results in more severe pathology. Here, we report that in mice infected with a mouse-adapted strain of SARS-CoV-2, treatment with a combination of two anti-CD44 monoclonal antibodies confers a significant survival benefit and reduces weight loss and clinical score of the mice on Day 4 post infection. We show that anti-CD44 treatment decreases many key cytokines and chemokines in the bronchoalveolar lavage fluid on Day 4. With flow cytometry, we show that anti-CD44 reduces the numbers of neutrophils in infected lungs. We also show through immunofluorescence that treatment with anti-CD44 antibodies reduces colocalization of HA and CD45 in lung sections, indicating that HA's interaction with immune cells contributes to pathology. Our findings demonstrate that disruption of HA-receptor interactions is a way to prevent inflammatory pathology in pulmonary infection.
Supplemental Material Supplementary Figure S1 . Anti-CD44 monoclonal antibody treatment does not reduce IV + neutrophil numbers. Changes in whole lung IV + lymphocyte numbers in whole lung homogenates taken from MA10-infected mice on day 4 post infection. Neutrophils (CD45 + CD11b + CD11c -Ly6C hi Ly6G + ), Inflammatory monocytes (CD45 + CD11b + CD11c -Ly6C hi Ly6G - ), B cells (CD45 + CD19 + SSC lo ), CD8 T cells (CD45 + CD3 + CD8 + SSC lo ), and CD4 T cells (CD45 + CD3 + CD4 + SSC lo ) are shown. No significant differences in P values calculated via one way ANOVA followed by Tukey's HSD test.
Supplementary Figure S2. Neutrophils make up the vast majority of Ly-6G + cells. Neutrophils (CD45 + CD11b + CD11c -Ly6C hi Ly6G + ) as percentage of all live Ly-6G + cells in whole lung homogenates taken from MA10-infected mice on day 4.
S1 Table. Immunofluorescence antibodies S2 Table. Flow cytometry antibodies
References
Adrover, Disulfiram inhibits neutrophil extracellular trap formation and protects rodents from acute lung injury and SARS-CoV-2 infection, JCI Insight
Albtoush, 7TSG6 hyaluronan matrix remodeling dampens the inflammatory response during colitis, Matrix Biology, doi:10.1016/j.matbio.2023.06.007
Banerji, Structures of the Cd44-hyaluronan complex provide insight into a fundamental carbohydrate-protein interaction, Nat Struct Mol Biol
Bano, Structure and unusual binding mechanism of the hyaluronan receptor LYVE-1 mediating leucocyte entry to lymphatics, Nat Commun
Baranova, Incorporation of Pentraxin 3 into Hyaluronan Matrices Is Tightly Regulated and Promotes Matrix Cross-linking, Journal of Biological Chemistry
Bell, Defective lung function following influenza virus is due to prolonged, reversible hyaluronan synthesis, Matrix Biol
Boivin, Durable and controlled depletion of neutrophils in mice, Nat Commun
Bono, Layilin, a Novel Integral Membrane Protein, Is a Hyaluronan Receptor, Mol Biol Cell
Briggs, Inter-α-inhibitor heavy chain-1 has an integrin-like 3D structure mediating immune regulatory activities and matrix stabilization during ovulation, Journal of Biological Chemistry
Camp, CD44 is necessary for optimal contact allergic responses but is not required for normal leukocyte extravasation, Journal of Experimental Medicine
Cavalli, Interleukin-1 and interleukin-6 inhibition compared with standard management in patients with COVID-19 and hyperinflammation: a cohort study, The Lancet Rheumatology
Chan, The Roles of Neutrophils in Cytokine Storms, Viruses
Clark, Mapping the Differential Distribution of Glycosaminoglycans in the Adult Human Retina, Choroid, and Sclera, Invest. Ophthalmol. Vis. Sci
Day, Milner, TSG-6: A multifunctional protein with anti-inflammatory and tissue-protective properties, Matrix Biology
De La Rosa, The CD44-Mediated Uptake of Hyaluronic Acid-Based Carriers in Macrophages, Advanced Healthcare Materials
Dinnon, A mouse-adapted model of SARS-CoV-2 to test COVID-19 countermeasures, Nature
Dinnon, SARS-CoV-2 infection produces chronic pulmonary epithelial and immune cell dysfunction with fibrosis in mice, Science Translational Medicine
Dodd, Injury From Nematode Lung Migration Induces an IL-13-Dependent Hyaluronan Matrix, Proteoglycan Research
Fielding, IL-6 Regulates Neutrophil Trafficking during Acute Inflammation via STAT31, J Immunol
Forteza, Hyaluronan and Layilin Mediate Loss of Airway Epithelial Barrier Function Induced by Cigarette Smoke by Decreasing E-cadherin, Journal of Biological Chemistry
Gao, Hypoxia-Induced Alterations in Hyaluronan and Hyaluronidase
George, A persistent neutrophil-associated immune signature characterizes post-COVID-19 pulmonary sequelae, Science Translational Medicine
Hasan, Targeting CD44 Expressed on Neutrophils Inhibits Lung Damage in Abdominal Sepsis, Shock
Heldin, Involvement of hyaluronan and CD44 in cancer and viral infections, Cellular Signalling
Jackson, Hyaluronan in the lymphatics: The key role of the hyaluronan receptor LYVE-1 in leucocyte trafficking, Matrix Biol
Kawaoka, Neutrophil adhesion to vessel walls impairs pulmonary circulation in COVID-19 pathology, Review
Kennel, CD44 expression on murine tissues, J Cell Sci
Kesmez Can, Effect of IL-6, IL-8/CXCL8, IP-10/CXCL 10 levels on the severity in COVID 19 infection, International Journal of Clinical Practice
Km, SouthernBiotech, catalog no. 1500-01) or 50µg of each of two isotype-matched control antibodies (IgG2b, BD Biosciences
Leist, A Mouse-Adapted SARS-CoV-2 Induces Acute Lung Injury and Mortality in Standard Laboratory Mice, Cell
Lesley, TSG-6 Modulates the Interaction between Hyaluronan and Cell Surface CD44 *, Journal of Biological Chemistry
Lucas, Longitudinal analyses reveal immunological misfiring in severe COVID-19, Nature
Mcdonald, Interaction of CD44 and hyaluronan is the dominant mechanism for neutrophil sequestration in inflamed liver sinusoids, J Exp Med
Mcdonald, Kubes, Interactions between CD44 and Hyaluronan in Leukocyte Trafficking, Front. Immunol
Mikecz, Modulation of hyaluronan receptor (CD44) function in vivo in a murine model of rheumatoid arthritis, Arthritis & Rheumatism
Morrissey, A specific low-density neutrophil population correlates with hypercoagulation and disease severity in hospitalized COVID-19 patients, JCI Insight
Ontong, Prachayasittikul, Unraveled roles of hyaluronan in severe COVID-19, EXCLI Journal
Petrey, De La Motte, Thrombin Cleavage of Inter-α-inhibitor Heavy Chain 1 Regulates Leukocyte Binding to an Inflammatory Hyaluronan Matrix*♦, Journal of Biological Chemistry
Petri, Sanz, Neutrophil chemotaxis, Cell Tissue Res
Reeves, Respiratory Syncytial Virus Infection of Human Lung Fibroblasts Induces a Hyaluronan-Enriched Extracellular Matrix That Binds Mast Cells and Enhances Expression of Mast Cell Proteases, Frontiers in Immunology
Rizzo, Dysfunctional Extracellular Matrix Remodeling Supports Perianal Fistulizing Crohn's Disease by a Mechanoregulated Activation of the Epithelial-to-Mesenchymal Transition, Cell Mol Gastroenterol Hepatol
Ruscitti, Recruited atypical Ly6G+ macrophages license alveolar regeneration after lung injury, Science Immunology
Sawant, Neutrophil recruitment by chemokines Cxcl1/KC and Cxcl2/MIP2: Role of Cxcr2 activation and glycosaminoglycan interactions, J Leukoc Biol
Schindelin, Fiji: an open-source platform for biological-image analysis, Nat Methods
Semaniakou, Disrupted local innervation results in less VIP expression in CF mice tissues, Journal of Cystic Fibrosis
Shah, The structural organisation of pentraxin-3 and its interactions with heavy chains of inter-α-inhibitor regulate crosslinking of the hyaluronan matrix, Matrix Biology
Tang, Inter-alpha-trypsin inhibitor (IαI) and hyaluronan modifications enhance the innate immune response to influenza virus in the lung, Matrix Biology
Toya, Cis-acting lnc-Cxcl2 restrains neutrophil-mediated lung inflammation by inhibiting epithelial cell CXCL2 expression in virus infection, Proceedings of the National Academy of Sciences
Varim, Neutrophil count to albumin ratio as a new predictor of mortality in patients with COVID-19 ınfection, Rev. Assoc. Med. Bras
Wang, CD44 Deficiency Leads to Enhanced Neutrophil Migration and Lung Injury in Escherichia coli Pneumonia in Mice, The American Journal of Pathology
Yang, Understanding the role of neutrophils in acute respiratory distress syndrome, Biomedical Journal
Zheng, CXCL12 ameliorates neutrophilia and disease severity in SARS-CoV-2 infection, J Clin Invest
Zheng, Monoclonal antibodies to CD44 and their influence on hyaluronan recognition, J Cell Biol
Zhuo, SHAP Potentiates the CD44-mediated Leukocyte Adhesion to the Hyaluronan Substratum*, Journal of Biological Chemistry
Zhuo, Syringaresinol Resisted Sepsis-Induced Acute Lung Injury by Suppressing Pyroptosis Via the Oestrogen Receptor-β Signalling Pathway, Inflammation
DOI record:
{
"DOI": "10.1101/2025.10.13.682000",
"URL": "http://dx.doi.org/10.1101/2025.10.13.682000",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>The novel respiratory disease COVID-19 caused by the coronavirus SARS-CoV-2 continues to be a public health emergency worldwide, and there is a need for more effective therapy for patients. The relationship between the extracellular matrix and the host immune response to infection is severely understudied. Deposition of the polysaccharide hyaluronan (HA) into the lungs is associated with more severe COVID-19 disease outcomes. HA is a major component of the extracellular matrix in connective tissues and is abundant in many parts of the body, including cartilage, skin, brain, and vitreous body. CD44 is the primary receptor for HA and is found on almost all immune cells in the lung. Known functions of CD44 include mediation of immune cell migration, activation, and differentiation. We hypothesized that increased HA deposition during COVID-19 increases CD44-mediated immune cell infiltration into lungs and results in more severe pathology. Here, we report that in mice infected with a mouse-adapted strain of SARS-CoV-2, treatment with a combination of two anti-CD44 monoclonal antibodies confers a significant survival benefit and reduces weight loss and clinical score of the mice on Day 4 post infection. We show that anti-CD44 treatment decreases many key cytokines and chemokines in the bronchoalveolar lavage fluid on Day 4. With flow cytometry, we show that anti-CD44 reduces the numbers of neutrophils in infected lungs. We also show through immunofluorescence that treatment with anti-CD44 antibodies reduces colocalization of HA and CD45 in lung sections, indicating that HA’s interaction with immune cells contributes to pathology. Our findings demonstrate that disruption of HA-receptor interactions is a way to prevent inflammatory pathology in pulmonary infection.</jats:p>",
"accepted": {
"date-parts": [
[
2025,
10,
14
]
]
},
"author": [
{
"ORCID": "https://orcid.org/0000-0003-0106-6020",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hart",
"given": "Duncan J.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Uddin",
"given": "Md. Jashim",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dodd",
"given": "Rebecca J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Brovero",
"given": "Savannah G.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fleming",
"given": "Claire",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moreau",
"given": "G. Brett",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Natale",
"given": "Nick R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mann",
"given": "Barbara J.",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-9334-8206",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sutherland",
"given": "Tara E.",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-3829-066X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Allen",
"given": "Judith E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Day",
"given": "Anthony J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Petri",
"given": "William A.",
"sequence": "additional",
"suffix": "Jr."
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
10,
14
]
],
"date-time": "2025-10-14T23:55:14Z",
"timestamp": 1760486114000
},
"deposited": {
"date-parts": [
[
2025,
10,
17
]
],
"date-time": "2025-10-17T16:50:24Z",
"timestamp": 1760719824000
},
"group-title": "Immunology",
"indexed": {
"date-parts": [
[
2025,
10,
17
]
],
"date-time": "2025-10-17T17:11:16Z",
"timestamp": 1760721076228,
"version": "build-2065373602"
},
"institution": [
{
"name": "bioRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2025,
10,
14
]
]
},
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
10,
14
]
],
"date-time": "2025-10-14T00:00:00Z",
"timestamp": 1760400000000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2025.10.13.682000",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2025,
10,
14
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2025,
10,
14
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference": [
{
"DOI": "10.1016/J.CELL.2020.08.001",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.1"
},
{
"DOI": "10.1172/jci.insight.147472",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.2",
"unstructured": "Queisser, K.A. et al. COVID-19 generates hyaluronan fragments that directly induce endothelial barrier dysfunction. JCI Insight 6, e147472"
},
{
"article-title": "SARS-CoV-2 infection induces hyaluronan production in vitro and hyaluronan levels in COVID-19 patients relate to morbidity and long-term lung impairment: a prospective cohort study",
"first-page": "e01303",
"journal-title": "mBio",
"key": "2025101709501082000_2025.10.13.682000v1.3",
"volume": "15",
"year": "2024"
},
{
"DOI": "10.1172/jci.insight.150107",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.4",
"unstructured": "Donlan, A.N., et al. (2021) IL-13 is a driver of COVID-19 severity. JCI Insight 6"
},
{
"DOI": "10.1172/jci.insight.152629",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.5",
"unstructured": "Kratochvil, M.J., et al. (2022) Biochemical, biophysical, and immunological characterization of respiratory secretions in severe SARS-CoV-2 infections. JCI Insight 7"
},
{
"DOI": "10.1038/s41598-025-09245-y",
"article-title": "Inflammatory, fibrotic and endothelial biomarker profiles in COVID-19 patients during and following hospitalization",
"doi-asserted-by": "crossref",
"first-page": "24850",
"journal-title": "Sci Rep",
"key": "2025101709501082000_2025.10.13.682000v1.6",
"volume": "15",
"year": "2025"
},
{
"DOI": "10.1002/pgr2.70007",
"article-title": "Hyaluronan-protein interactions: Lilliput revisited",
"doi-asserted-by": "crossref",
"first-page": "e70007",
"journal-title": "Proteoglycan Research",
"key": "2025101709501082000_2025.10.13.682000v1.7",
"volume": "2",
"year": "2024"
},
{
"DOI": "10.1126/science.abp8964",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.8"
},
{
"DOI": "10.3389/fimmu.2014.00101",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.9",
"unstructured": "Petrey, A.C. and de la Motte, C.A. (2014) Hyaluronan, a Crucial Regulator of Inflammation. Front. Immunol. 5"
},
{
"DOI": "10.3389/fimmu.2018.02787",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.10"
},
{
"DOI": "10.1136/thx.44.2.126",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.11"
},
{
"article-title": "Hyaluronan in COVID-19: a matrix for understanding lung disease",
"first-page": "e02609",
"journal-title": "mBio",
"key": "2025101709501082000_2025.10.13.682000v1.12",
"volume": "15",
"year": "2024"
},
{
"DOI": "10.1074/jbc.AC120.015967",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.13"
},
{
"DOI": "10.1165/rcmb.2006-0018OC",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.14"
},
{
"DOI": "10.1016/j.matbio.2018.06.006",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.15"
},
{
"DOI": "10.1002/pgr2.70012",
"article-title": "Injury From Nematode Lung Migration Induces an IL-13-Dependent Hyaluronan Matrix",
"doi-asserted-by": "crossref",
"first-page": "e70012",
"journal-title": "Proteoglycan Research",
"key": "2025101709501082000_2025.10.13.682000v1.16",
"volume": "2",
"year": "2024"
},
{
"article-title": "Unraveled roles of hyaluronan in severe COVID-19",
"first-page": "117",
"journal-title": "EXCLI Journal",
"key": "2025101709501082000_2025.10.13.682000v1.17",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1007/0-387-26206-7_33",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.18",
"unstructured": "Gao, F. et al. (2005) Hypoxia-Induced Alterations in Hyaluronan and Hyaluronidase. In Oxygen Transport to Tissue XXVI, Boston, MA, pp. 249–256"
},
{
"DOI": "10.1016/j.matbio.2023.06.007",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.19"
},
{
"DOI": "10.1016/j.jcmgh.2022.12.006",
"article-title": "Dysfunctional Extracellular Matrix Remodeling Supports Perianal Fistulizing Crohn’s Disease by a Mechanoregulated Activation of the Epithelial-to-Mesenchymal Transition",
"doi-asserted-by": "crossref",
"first-page": "741",
"journal-title": "Cell Mol Gastroenterol Hepatol",
"key": "2025101709501082000_2025.10.13.682000v1.20",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1097/SHK.0b013e3182144935",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.21"
},
{
"DOI": "10.1242/jcs.104.2.373",
"article-title": "CD44 expression on murine tissues",
"doi-asserted-by": "crossref",
"first-page": "373",
"journal-title": "J Cell Sci",
"key": "2025101709501082000_2025.10.13.682000v1.22",
"volume": "104",
"year": "1993"
},
{
"DOI": "10.3389/fimmu.2015.00068",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.23",
"unstructured": "McDonald, B. and Kubes, P . (2015) Interactions between CD44 and Hyaluronan in Leukocyte Trafficking. Front. Immunol. 6"
},
{
"DOI": "10.1016/j.cellsig.2019.109427",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.24"
},
{
"DOI": "10.1016/j.matbio.2018.01.011",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.25",
"unstructured": "Day, A.J. and Milner, C.M . (2019) TSG-6: A multifunctional protein with anti-inflammatory and tissue-protective properties. Matrix Biology 78–79, 60–83"
},
{
"DOI": "10.1016/j.matbio.2024.01.004",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.26"
},
{
"DOI": "10.1074/jbc.RA119.011916",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.27"
},
{
"DOI": "10.1016/j.matbio.2025.01.002",
"article-title": "The structural organisation of pentraxin-3 and its interactions with heavy chains of inter-α-inhibitor regulate crosslinking of the hyaluronan matrix",
"doi-asserted-by": "crossref",
"first-page": "52",
"journal-title": "Matrix Biology",
"key": "2025101709501082000_2025.10.13.682000v1.28",
"volume": "136",
"year": "2025"
},
{
"DOI": "10.1074/jbc.M114.568154",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.29"
},
{
"DOI": "10.1074/jbc.M506703200",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.30"
},
{
"DOI": "10.1074/jbc.M116.755660",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.31"
},
{
"DOI": "10.1016/S0002-9440(10)64498-7",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.32"
},
{
"DOI": "10.3390/v13112318",
"article-title": "The Roles of Neutrophils in Cytokine Storms",
"doi-asserted-by": "crossref",
"first-page": "2318",
"journal-title": "Viruses",
"key": "2025101709501082000_2025.10.13.682000v1.33",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1172/jci.insight.148435",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.34",
"unstructured": "Morrissey, S.M., et al. (2021) A specific low-density neutrophil population correlates with hypercoagulation and disease severity in hospitalized COVID-19 patients. JCI Insight 6"
},
{
"DOI": "10.1590/1806-9282.66.s2.77",
"article-title": "Neutrophil count to albumin ratio as a new predictor of mortality in patients with COVID-19 ınfection",
"doi-asserted-by": "crossref",
"first-page": "77",
"journal-title": "Rev. Assoc. Med. Bras",
"key": "2025101709501082000_2025.10.13.682000v1.35",
"volume": "66",
"year": "2020"
},
{
"DOI": "10.1126/scitranslmed.abo5795",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.36"
},
{
"DOI": "10.1172/jci.insight.157342",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.37",
"unstructured": "Adrover, J.M. et al. Disulfiram inhibits neutrophil extracellular trap formation and protects rodents from acute lung injury and SARS-CoV-2 infection. JCI Insight 7, e157342"
},
{
"DOI": "10.1016/S2665-9913(21)00012-6",
"article-title": "Interleukin-1 and interleukin-6 inhibition compared with standard management in patients with COVID-19 and hyperinflammation: a cohort study",
"doi-asserted-by": "crossref",
"first-page": "e253",
"journal-title": "The Lancet Rheumatology",
"key": "2025101709501082000_2025.10.13.682000v1.38",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2588-y",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.39"
},
{
"article-title": "Effect of IL-6, IL-8/CXCL8, IP-10/CXCL 10 levels on the severity in COVID 19 infection",
"first-page": "e14970",
"journal-title": "International Journal of Clinical Practice",
"key": "2025101709501082000_2025.10.13.682000v1.40",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1084/jem.20071765",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.41"
},
{
"DOI": "10.1016/j.cell.2020.09.050",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.42"
},
{
"article-title": "SARS-CoV-2 infection produces chronic pulmonary epithelial and immune cell dysfunction with fibrosis in mice",
"first-page": "eabo5070",
"journal-title": "Science Translational Medicine",
"key": "2025101709501082000_2025.10.13.682000v1.43",
"volume": "0",
"year": "2022"
},
{
"DOI": "10.3390/v13010132",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.44"
},
{
"DOI": "10.1083/jcb.130.2.485",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.45"
},
{
"DOI": "10.1084/jem.178.2.497",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.46"
},
{
"DOI": "10.1002/1529-0131(199904)42:4<659::AID-ANR8>3.0.CO;2-Z",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.47"
},
{
"DOI": "10.1007/s10753-021-01587-9",
"article-title": "Syringaresinol Resisted Sepsis-Induced Acute Lung Injury by Suppressing Pyroptosis Via the Oestrogen Receptor-β Signalling Pathway",
"doi-asserted-by": "crossref",
"first-page": "824",
"journal-title": "Inflammation",
"key": "2025101709501082000_2025.10.13.682000v1.48",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.4049/jimmunol.181.3.2189",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.49"
},
{
"DOI": "10.1002/JLB.3A0820-207R",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.50"
},
{
"DOI": "10.1007/s00441-017-2776-8",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.51"
},
{
"DOI": "10.1183/16000617.0172-2023",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.52",
"unstructured": "Toya, S. et al. (2024) A narrative review of chemokine receptors CXCR1 and CXCR2 and their role in acute respiratory distress syndrome. European Respiratory Review 33"
},
{
"DOI": "10.1073/pnas.2108276118",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.53"
},
{
"DOI": "10.1126/sciimmunol.ado1227",
"article-title": "Recruited atypical Ly6G+ macrophages license alveolar regeneration after lung injury",
"doi-asserted-by": "crossref",
"first-page": "eado1227",
"journal-title": "Science Immunology",
"key": "2025101709501082000_2025.10.13.682000v1.54",
"volume": "9",
"year": "2024"
},
{
"DOI": "10.1016/j.bj.2020.09.001",
"article-title": "Understanding the role of neutrophils in acute respiratory distress syndrome",
"doi-asserted-by": "crossref",
"first-page": "439",
"journal-title": "Biomedical Journal",
"key": "2025101709501082000_2025.10.13.682000v1.55",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.21203/rs.3.rs-3895679/v1",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.56",
"unstructured": "Kawaoka, Y., et al. (2024) Neutrophil adhesion to vessel walls impairs pulmonary circulation in COVID-19 pathology, In Review"
},
{
"DOI": "10.1172/JCI188222",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.57",
"unstructured": "Zheng, J. et al. (2025) CXCL12 ameliorates neutrophilia and disease severity in SARS-CoV-2 infection. J Clin Invest 135"
},
{
"DOI": "10.1074/jbc.M313319200",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.58"
},
{
"DOI": "10.1002/adhm.201601012",
"article-title": "The CD44-Mediated Uptake of Hyaluronic Acid-Based Carriers in Macrophages",
"doi-asserted-by": "crossref",
"first-page": "1601012",
"journal-title": "Advanced Healthcare Materials",
"key": "2025101709501082000_2025.10.13.682000v1.59",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.1091/mbc.12.4.891",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.60"
},
{
"DOI": "10.1016/j.matbio.2018.02.001",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.61"
},
{
"DOI": "10.1038/s41467-025-57866-8",
"article-title": "Structure and unusual binding mechanism of the hyaluronan receptor LYVE-1 mediating leucocyte entry to lymphatics",
"doi-asserted-by": "crossref",
"first-page": "2754",
"journal-title": "Nat Commun",
"key": "2025101709501082000_2025.10.13.682000v1.62",
"volume": "16",
"year": "2025"
},
{
"DOI": "10.1038/nsmb1201",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.63"
},
{
"DOI": "10.1074/jbc.M112.387795",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.64"
},
{
"DOI": "10.3389/fimmu.2019.03159",
"doi-asserted-by": "crossref",
"key": "2025101709501082000_2025.10.13.682000v1.65",
"unstructured": "Reeves, S.R. et al. (2020) Respiratory Syncytial Virus Infection of Human Lung Fibroblasts Induces a Hyaluronan-Enriched Extracellular Matrix That Binds Mast Cells and Enhances Expression of Mast Cell Proteases. Frontiers in Immunology 10"
},
{
"DOI": "10.1038/s41586-020-2708-8",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.66"
},
{
"DOI": "10.1038/s41467-020-16596-9",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.67"
},
{
"DOI": "10.1016/j.jcf.2020.06.013",
"article-title": "Disrupted local innervation results in less VIP expression in CF mice tissues",
"doi-asserted-by": "crossref",
"first-page": "154",
"journal-title": "Journal of Cystic Fibrosis",
"key": "2025101709501082000_2025.10.13.682000v1.68",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1167/iovs.11-7909",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.69"
},
{
"DOI": "10.1038/nmeth.2019",
"doi-asserted-by": "publisher",
"key": "2025101709501082000_2025.10.13.682000v1.70"
}
],
"reference-count": 70,
"references-count": 70,
"relation": {},
"resource": {
"primary": {
"URL": "http://biorxiv.org/lookup/doi/10.1101/2025.10.13.682000"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"subtype": "preprint",
"title": "The hyaluronan receptor CD44 drives COVID-19 severity through its regulation of neutrophil migration",
"type": "posted-content"
}