FX06 to rescue SARS-CoV-2-induced acute respiratory distress syndrome: a randomized clinical trial
et al., Critical Care, doi:10.1186/s13054-023-04616-1, NCT04618042, Aug 2023
RCT 49 patients with COVID-19-associated ARDS showing no significant effect of FX06 on vascular leakage or mortality.
|
risk of death, 9.7% higher, RR 1.10, p = 1.00, treatment 8 of 25 (32.0%), control 7 of 24 (29.2%), day 60.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Guérin et al., 29 Aug 2023, Double Blind Randomized Controlled Trial, placebo-controlled, France, peer-reviewed, median age 64.0, 14 authors, study period 11 November, 2020 - 15 April, 2021, average treatment delay 13.0 days, trial NCT04618042 (history).
Contact: nicolas.brechot@aphp.fr.
FX06 to rescue SARS-CoV-2-induced acute respiratory distress syndrome: a randomized clinical trial
Critical Care, doi:10.1186/s13054-023-04616-1
Background Vascular leakage is a major feature of acute respiratory distress syndrome (ARDS). We aimed to evaluate the efficacy of FX06, a drug under development that stabilizes interendothelial cell junctions, at reducing vascular leakage during SARS-CoV-2-induced ARDS. Methods This multicenter, double-blinded, randomized trial included adults with COVID-19-associated ARDS who had received invasive mechanical ventilation for < 5 days and were randomized to receive either intravenous FX06 (400 mg/d, for 5 days) or its vehicle as placebo. The primary endpoint was the lowering-from day 1 to day 7-of the transpulmonary thermodilution-derived extravascular lung-water index (EVLWi).
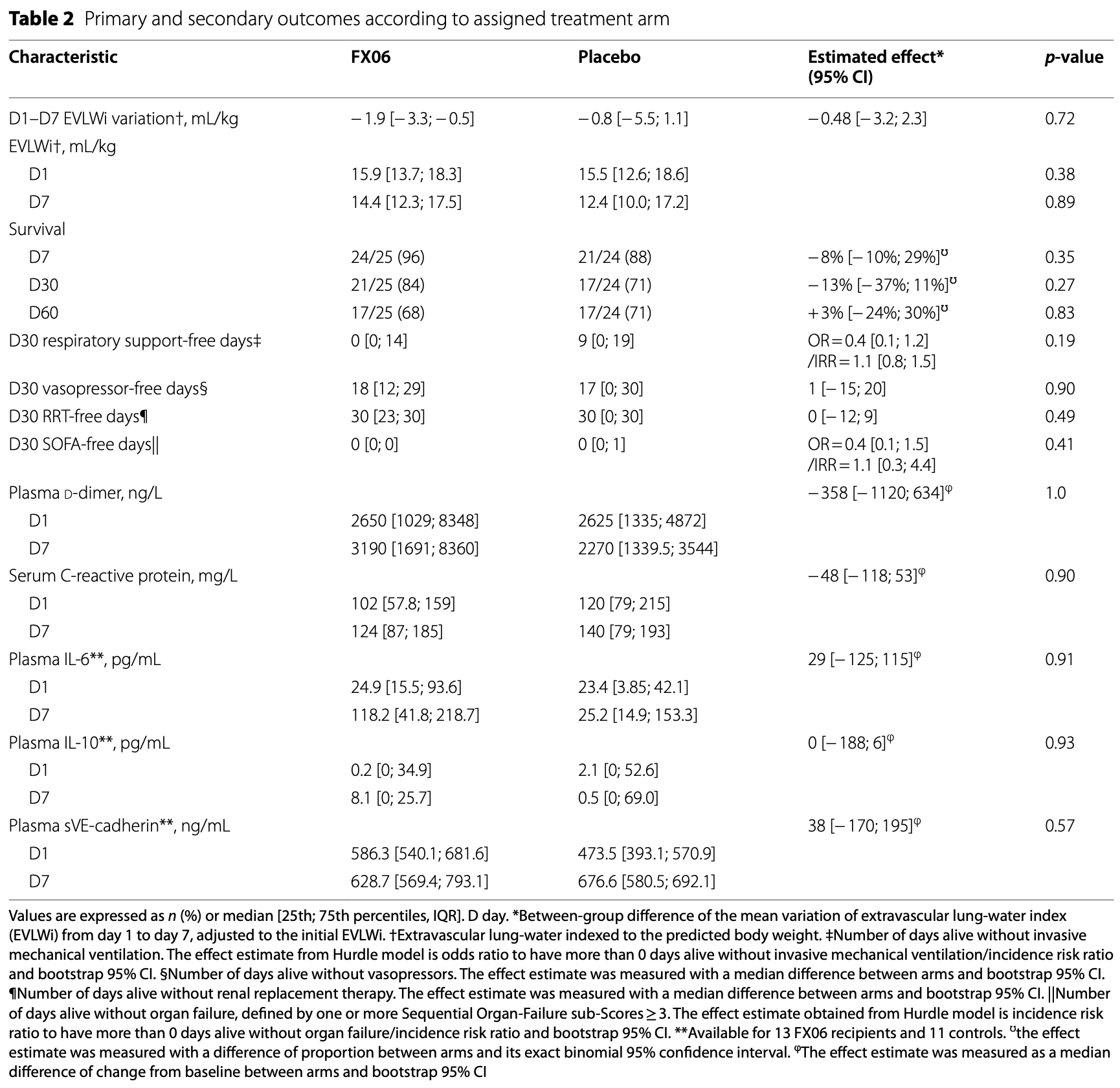
Results Twenty-five patients were randomized to receive FX06 and 24 the placebo. Although EVLWi was elevated at baseline (median [IQR] 15.6 mL/kg [13.5; 18.5]), its declines from day 1 to day 7 were comparable for FX06 recipients and controls (respectively, -1.9 [-3.3; -0.5] vs. -0.8 [-5.5; -1.1] mL/kg; estimated effect -0.8 [-3.1; + 2.4], p = 0.51). Cardiac indexes, pulmonary vascular permeability indexes, and fluid balances were also comparable, as were PaO 2 / FiO 2 ratios and durations of mechanical ventilation. Adverse event rates were similar for the 2 groups, although more FX06 recipients developed ventilator-associated pneumonia (16/25 (64%) vs. 6/24 (24%), p = 0.009).
Conclusions In this unique-dosing-regimen study, FX06 did not lower SARS-CoV-2-induced pulmonary vascular leakage. Future investigations will need to evaluate its efficacy at earlier times during the disease or using other regimens.
Abbreviations
ARDS Acute respiratory distress syndrome ECMO Extracorporeal membrane oxygenation EVLWi Extravascular lung-water index (s)VE-cadherin (soluble) vascular endothelial cadherin SARS-CoV-2 Severe acute respiratory syndrome-coronavirus-2 COVID- 19 Coronavirus disease 2019
Supplementary Information The online version contains supplementary material available at https:// doi. org/ 10. 1186/ s13054-023-04616-1 . Additional file 1. The study protocol. Additional file 2. The supplementary data.
Author contributions NB had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. • fast, convenient online submission • thorough peer review by experienced researchers in your field • rapid publication on acceptance • support for research data, including large and complex data types • gold Open Access which fosters wider collaboration and increased citations maximum visibility for your research: over 100M website views per year
• At BMC, research is always in progress.
Learn more biomedcentral.com/submissions Ready to submit your research Ready to submit your research ? Choose BMC and benefit from: ? Choose BMC and benefit from:
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Ackermann, Verleden, Kuehnel, Haverich, Welte et al., Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19, N Engl J Med
Adam, Schmid, Sonntagbauer, Kranke, Zacharowski et al., Fibrin-derived peptide Bβ15-42 (FX06) as salvage treatment in critically ill patients with COVID-19-associated acute respiratory distress syndrome, Crit Care
Ards Definition, Force, Ranieri, Rubenfeld, Thompson et al., Acute respiratory distress syndrome: the Berlin Definition, JAMA
Atar, Petzelbauer, Schwitter, Huber, Rensing et al., Effect of intravenous FX06 as an adjunct to primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction results of the F.I.R.E. (Efficacy of FX06 in the Prevention of Myocardial Reperfusion Injury) trial, J Am Coll Cardiol
Bach, Barsigian, Yaen, Martinez, Endothelial cell VE-cadherin functions as a receptor for the beta15-42 sequence of fibrin, J Biol Chem
Bergt, Gruenewald, Beltschany, Grub, Neumann et al., The Fibrin-Derived Peptide Bβ15-42 (FX06) Ameliorates Vascular Leakage and Improves Survival and Neurocognitive Recovery: Implications From Two Animal Models of Cardiopulmonary Resuscitation, Crit Care Med
Bréchot, Demondion, Santi, Lebreton, Pham et al., Intra-aortic balloon pump protects against hydrostatic pulmonary oedema during peripheral venoarterial-extracorporeal membrane oxygenation, Eur Heart J Acute Cardiovasc Care
Clajus, Lukasz, David, Hertel, Lichtinghagen et al., Angiopoietin-2 is a potential mediator of endothelial barrier dysfunction following cardiopulmonary bypass, Cytokine
D' Agnillo, Walters, Xiao, Sheng, Scherler et al., Lung epithelial and endothelial damage, loss of tissue repair, inhibition of fibrinolysis, and cellular senescence in fatal COVID-19, Sci Transl Med
Dupont, Rauch, Staessens, Moussa, Rosa et al., Vascular Endothelial Damage in the Pathogenesis of Organ Injury in Severe COVID-19, Arterioscler Thromb Vasc Biol
Flemming, Burkard, Renschler, Vielmuth, Meir et al., Soluble VE-cadherin is involved in endothelial barrier breakdown in systemic inflammation and sepsis, Cardiovasc Res
Giannotta, Trani, Dejana, VE-cadherin and endothelial adherens junctions: active guardians of vascular integrity, Dev Cell
Gröger, Pasteiner, Ignatyev, Matt, Knapp et al., Peptide Bbeta(15-42) preserves endothelial barrier function in shock, PLoS ONE
Herner, Lahmer, Mayr, Rasch, Schneider et al., Transpulmonary thermodilution before and during veno-venous extracorporeal membrane oxygenation ECMO: an observational study on a potential loss of indicator into the extra-corporeal circuit, J Clin Monit Comput
Jozwiak, Silva, Persichini, Anguel, Osman et al., Extravascular lung water is an independent prognostic factor in patients with acute respiratory distress syndrome*, Crit Care Med
Loosen, Conrad, Hagman, Essert, Thiel et al., Transpulmonary thermodilution in patients treated with veno-venous extracorporeal membrane oxygenation, Ann Intensive Care
Luyt, Sahnoun, Gautier, Vidal, Burrel et al., Ventilator-associated pneumonia in patients with SARS-CoV-2-associated acute respiratory distress syndrome requiring ECMO: a retrospective cohort study, Ann Intensive Care
Marconi, Ramanan, De Bono, Kartman, Krishnan et al., Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled phase 3 trial, Lancet Respir Med
Matt, Warszawska, Bauer, Dietl, Mesteri et al., Bbeta(15-42) protects against acid-induced acute lung injury and secondary pseudomonas pneumonia in vivo, Am J Respir Crit Care Med
Matthay, Zemans, The acute respiratory distress syndrome: pathogenesis and treatment, Annu Rev Pathol
Michalick, Weidenfeld, Grimmer, Fatykhova, Solymosi et al., Plasma mediators in patients with severe COVID-19 cause lung endothelial barrier failure, Eur Respir J
Petzelbauer, Zacharowski, Miyazaki, Friedl, Wickenhauser et al., The fibrin-derived peptide Bbeta15-42 protects the myocardium against ischemia-reperfusion injury, Nat Med
Rasch, Schmidle, Sancak, Herner, Huberle et al., Increased extravascular lung water index (EVLWI) reflects rapid noncardiogenic oedema and mortality in COVID-19 associated ARDS, Sci Rep
Rauch, Dupont, Goutay, Caplan, Staessens et al., Endotheliopathy Is Induced by Plasma From Critically Ill Patients and Associated With Organ Failure in Severe COVID-19, Circulation
Recovery Collaborative Group, Horby, Lim, Emberson, Mafham et al., Dexamethasone in Hospitalized Patients with Covid-19 -Preliminary Report, N Engl J Med
Roesner, Petzelbauer, Koch, Mersmann, Zacharowski et al., The fibrin-derived peptide Bbeta15-42 is cardioprotective in a pig model of myocardial ischemia-reperfusion injury, Crit Care Med
Shi, Lai, Teboul, Dres, Moretto et al., COVID-19 ARDS is characterized by higher extravascular lung water than non-COVID-19 ARDS: the PiCCOVID study, Crit Care Lond Engl
Spadaro, Fogagnolo, Campo, Zucchetti, Verri et al., Markers of endothelial and epithelial pulmonary injury in mechanically ventilated COVID-19 ICU patients, Crit Care
Tagami, Kushimoto, Yamamoto, Atsumi, Tosa et al., Validation of extravascular lung water measurement by single transpulmonary thermodilution: human autopsy study, Crit Care
Tagami, Ong, Extravascular lung water measurements in acute respiratory distress syndrome: why, how, and when?, Curr Opin Crit Care
Teuwen, Geldhof, Pasut, Carmeliet, COVID-19: the vasculature unleashed, Nat Rev Immunol
Van De Weg, Pannuti, Van Den Ham, De Araújo, Boas et al., Serum angiopoietin-2 and soluble VEGF receptor 2 are surrogate markers for plasma leakage in patients with acute dengue virus infection, J Clin Virol Off Publ Pan Am Soc Clin Virol
Varga, Flammer, Steiger, Haberecker, Andermatt et al., Endothelial cell infection and endotheliitis in COVID-19, Lancet
Vassiliou, Keskinidou, Jahaj, Gallos, Dimopoulou et al., ICU Admission Levels of Endothelial Biomarkers as Predictors of Mortality in Critically Ill COVID-19 Patients, Cells
Wang, Cui, Su, Long, Wang et al., Prognostic value of extravascular lung water and its potential role in guiding fluid therapy in septic shock after initial resuscitation, J Crit Care
Wichmann, Sperhake, Lütgehetmann, Steurer, Edler et al., Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study, Ann Intern Med
Wolf, Kann, Becker, Stephan, Brodt et al., Severe Ebola virus disease with vascular leakage and multiorgan failure: treatment of a patient in intensive care, Lancet Lond Engl
Wollborn, Hassenzahl, Reker, Staehle, Omlor et al., Diagnosing capillary leak in critically ill patients: development of an innovative scoring instrument for non-invasive detection, Ann Intensive Care
Yakovlev, Gao, Cao, Chen, Strickland et al., Interaction of fibrin with VE-cadherin and anti-inflammatory effect of fibrin-derived fragments, J Thromb Haemost JTH
Yu, Mcneil, Wickersham, Shaver, Bastarache et al., Vascular endothelial cadherin shedding is more severe in sepsis patients with severe acute kidney injury, Crit Care
DOI record:
{
"DOI": "10.1186/s13054-023-04616-1",
"ISSN": [
"1364-8535"
],
"URL": "http://dx.doi.org/10.1186/s13054-023-04616-1",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Vascular leakage is a major feature of acute respiratory distress syndrome (ARDS). We aimed to evaluate the efficacy of FX06, a drug under development that stabilizes interendothelial cell junctions, at reducing vascular leakage during SARS-CoV-2-induced ARDS.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>This multicenter, double-blinded, randomized trial included adults with COVID-19-associated ARDS who had received invasive mechanical ventilation for < 5 days and were randomized to receive either intravenous FX06 (400 mg/d, for 5 days) or its vehicle as placebo. The primary endpoint was the lowering—from day 1 to day 7—of the transpulmonary thermodilution-derived extravascular lung-water index (EVLWi).</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Twenty-five patients were randomized to receive FX06 and 24 the placebo. Although EVLWi was elevated at baseline (median [IQR] 15.6 mL/kg [13.5; 18.5]), its declines from day 1 to day 7 were comparable for FX06 recipients and controls (respectively, − 1.9 [− 3.3; − 0.5] vs. − 0.8 [− 5.5; − 1.1] mL/kg; estimated effect − 0.8 [− 3.1; + 2.4], <jats:italic>p</jats:italic> = 0.51). Cardiac indexes, pulmonary vascular permeability indexes, and fluid balances were also comparable, as were PaO<jats:sub>2</jats:sub>/FiO<jats:sub>2</jats:sub> ratios and durations of mechanical ventilation. Adverse event rates were similar for the 2 groups, although more FX06 recipients developed ventilator-associated pneumonia (16/25 (64%) vs. 6/24 (24%), <jats:italic>p</jats:italic> = 0.009).</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>In this unique-dosing–regimen study, FX06 did not lower SARS-CoV-2-induced pulmonary vascular leakage. Future investigations will need to evaluate its efficacy at earlier times during the disease or using other regimens.</jats:p>\n <jats:p><jats:italic>Trial registration</jats:italic> NCT04618042. Registered 5 November 2020.</jats:p>\n </jats:sec>",
"alternative-id": [
"4616"
],
"article-number": "331",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "9 February 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "16 August 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "29 August 2023"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The independent ethics review board CPP Ouest VI, Brest, France, approved the trial protocol (CPP 1306-EudraCT 2020-002056-20/RIPH 20.06.15.56627). The trial was conducted in accordance with the ethical principles of the Declaration of Helsinki, the International Conference on Harmonisation–Good Clinical Practice (ICH-GCP) guideline, the Quality Management Standards for Drug Clinical Trials of the French Food and Drug Administration (ANSM, Agence Nationale de Sécurité du Médicament et des Produits de Santé). According to the specifications of emergency consent, randomization without a close relative or surrogate consent could be performed, but informed consent by the patient or patient’s relatives was obtained for all patients."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Not applicable."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "Dr Bréchot is on the F4-Pharma advisory board, without any financial competing interest. He received a grant from the French Ministry of Health for another study evaluating FX06. He receives fees from Findimmune, outside the scope of this study. Dr Luyt reported receiving grants from French Ministry of Health during the conduct of the study; personal fees from Bayer Healthcare, Carmat, Faron, Merck Sharp & Dohme, ThermoFisher Brahms, and BioMérieux, outside the submitted work. Dr. Combes reports receiving grant support and lecture fees from Maquet and Baxter, and consulting fees from Hemovent."
}
],
"author": [
{
"affiliation": [],
"family": "Guérin",
"given": "Emmanuelle",
"sequence": "first"
},
{
"affiliation": [],
"family": "Belin",
"given": "Lisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Franchineau",
"given": "Guillaume",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Le Guennec",
"given": "Loïc",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hajage",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Diallo",
"given": "Mamadou Hassimiou",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Frapard",
"given": "Thomas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Le Fèvre",
"given": "Lucie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Luyt",
"given": "Charles-Edouard",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Combes",
"given": "Alain",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Germain",
"given": "Stéphane",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hayon",
"given": "Jan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Asfar",
"given": "Pierre",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bréchot",
"given": "Nicolas",
"sequence": "additional"
}
],
"container-title": "Critical Care",
"container-title-short": "Crit Care",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2023,
8,
29
]
],
"date-time": "2023-08-29T02:01:44Z",
"timestamp": 1693274504000
},
"deposited": {
"date-parts": [
[
2023,
11,
19
]
],
"date-time": "2023-11-19T13:37:58Z",
"timestamp": 1700401078000
},
"indexed": {
"date-parts": [
[
2023,
11,
20
]
],
"date-time": "2023-11-20T00:14:00Z",
"timestamp": 1700439240890
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2023,
8,
29
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2023,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
8,
29
]
],
"date-time": "2023-08-29T00:00:00Z",
"timestamp": 1693267200000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
8,
29
]
],
"date-time": "2023-08-29T00:00:00Z",
"timestamp": 1693267200000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s13054-023-04616-1.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s13054-023-04616-1/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s13054-023-04616-1.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2023,
8,
29
]
]
},
"published-online": {
"date-parts": [
[
2023,
8,
29
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1146/annurev-pathol-011110-130158",
"author": "MA Matthay",
"doi-asserted-by": "publisher",
"first-page": "147",
"journal-title": "Annu Rev Pathol",
"key": "4616_CR1",
"unstructured": "Matthay MA, Zemans RL. The acute respiratory distress syndrome: pathogenesis and treatment. Annu Rev Pathol. 2011;6:147–63.",
"volume": "6",
"year": "2011"
},
{
"DOI": "10.1097/MCC.0000000000000503",
"author": "T Tagami",
"doi-asserted-by": "publisher",
"first-page": "209",
"journal-title": "Curr Opin Crit Care",
"key": "4616_CR2",
"unstructured": "Tagami T, Ong MEH. Extravascular lung water measurements in acute respiratory distress syndrome: why, how, and when? Curr Opin Crit Care. 2018;24:209–15.",
"volume": "24",
"year": "2018"
},
{
"DOI": "10.1097/CCM.0b013e31826ab377",
"author": "M Jozwiak",
"doi-asserted-by": "publisher",
"first-page": "472",
"journal-title": "Crit Care Med",
"key": "4616_CR3",
"unstructured": "Jozwiak M, Silva S, Persichini R, Anguel N, Osman D, Richard C, et al. Extravascular lung water is an independent prognostic factor in patients with acute respiratory distress syndrome*. Crit Care Med. 2013;41:472–80.",
"volume": "41",
"year": "2013"
},
{
"DOI": "10.1186/s13054-021-03594-6",
"author": "R Shi",
"doi-asserted-by": "publisher",
"first-page": "186",
"journal-title": "Crit Care Lond Engl",
"key": "4616_CR4",
"unstructured": "Shi R, Lai C, Teboul J-L, Dres M, Moretto F, De Vita N, et al. COVID-19 ARDS is characterized by higher extravascular lung water than non-COVID-19 ARDS: the PiCCOVID study. Crit Care Lond Engl. 2021;25:186.",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-91043-3",
"author": "S Rasch",
"doi-asserted-by": "publisher",
"first-page": "11524",
"journal-title": "Sci Rep",
"key": "4616_CR5",
"unstructured": "Rasch S, Schmidle P, Sancak S, Herner A, Huberle C, Schulz D, et al. Increased extravascular lung water index (EVLWI) reflects rapid non-cardiogenic oedema and mortality in COVID-19 associated ARDS. Sci Rep. 2021;11:11524.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(21)00331-3",
"author": "VC Marconi",
"doi-asserted-by": "publisher",
"first-page": "1407",
"journal-title": "Lancet Respir Med",
"key": "4616_CR6",
"unstructured": "Marconi VC, Ramanan AV, de Bono S, Kartman CE, Krishnan V, Liao R, et al. Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled phase 3 trial. Lancet Respir Med. 2021;9:1407–18.",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1111/j.1538-7836.2011.04438.x",
"author": "S Yakovlev",
"doi-asserted-by": "publisher",
"first-page": "1847",
"journal-title": "J Thromb Haemost JTH",
"key": "4616_CR7",
"unstructured": "Yakovlev S, Gao Y, Cao C, Chen L, Strickland DK, Zhang L, et al. Interaction of fibrin with VE-cadherin and anti-inflammatory effect of fibrin-derived fragments. J Thromb Haemost JTH. 2011;9:1847–55.",
"volume": "9",
"year": "2011"
},
{
"DOI": "10.1074/jbc.273.46.30719",
"author": "TL Bach",
"doi-asserted-by": "publisher",
"first-page": "30719",
"journal-title": "J Biol Chem",
"key": "4616_CR8",
"unstructured": "Bach TL, Barsigian C, Yaen CH, Martinez J. Endothelial cell VE-cadherin functions as a receptor for the beta15-42 sequence of fibrin. J Biol Chem. 1998;273:30719–28.",
"volume": "273",
"year": "1998"
},
{
"DOI": "10.1371/journal.pone.0005391",
"author": "M Gröger",
"doi-asserted-by": "publisher",
"journal-title": "PLoS ONE",
"key": "4616_CR9",
"unstructured": "Gröger M, Pasteiner W, Ignatyev G, Matt U, Knapp S, Atrasheuskaya A, et al. Peptide Bbeta(15–42) preserves endothelial barrier function in shock. PLoS ONE. 2009;4: e5391.",
"volume": "4",
"year": "2009"
},
{
"DOI": "10.1164/rccm.200904-0626OC",
"author": "U Matt",
"doi-asserted-by": "publisher",
"first-page": "1208",
"journal-title": "Am J Respir Crit Care Med",
"key": "4616_CR10",
"unstructured": "Matt U, Warszawska JM, Bauer M, Dietl W, Mesteri I, Doninger B, et al. Bbeta(15–42) protects against acid-induced acute lung injury and secondary pseudomonas pneumonia in vivo. Am J Respir Crit Care Med. 2009;180:1208–17.",
"volume": "180",
"year": "2009"
},
{
"DOI": "10.1016/j.jacc.2008.12.017",
"doi-asserted-by": "crossref",
"key": "4616_CR11",
"unstructured": "Atar D, Petzelbauer P, Schwitter J, Huber K, Rensing B, Kasprzak JD, et al. Effect of intravenous FX06 as an adjunct to primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction results of the F.I.R.E. (Efficacy of FX06 in the Prevention of Myocardial Reperfusion Injury) trial. J Am Coll Cardiol. 2009;53:720–9."
},
{
"DOI": "10.1016/S0140-6736(14)62384-9",
"author": "T Wolf",
"doi-asserted-by": "publisher",
"first-page": "1428",
"journal-title": "Lancet Lond Engl",
"key": "4616_CR12",
"unstructured": "Wolf T, Kann G, Becker S, Stephan C, Brodt H-R, de Leuw P, et al. Severe Ebola virus disease with vascular leakage and multiorgan failure: treatment of a patient in intensive care. Lancet Lond Engl. 2015;385:1428–35.",
"volume": "385",
"year": "2015"
},
{
"DOI": "10.1186/s13054-020-03293-8",
"author": "EH Adam",
"doi-asserted-by": "publisher",
"first-page": "574",
"journal-title": "Crit Care",
"key": "4616_CR13",
"unstructured": "Adam EH, Schmid B, Sonntagbauer M, Kranke P, Zacharowski K, Meybohm P. Fibrin-derived peptide Bβ15-42 (FX06) as salvage treatment in critically ill patients with COVID-19-associated acute respiratory distress syndrome. Crit Care. 2020;24:574.",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1001/jama.2012.5669",
"doi-asserted-by": "crossref",
"key": "4616_CR14",
"unstructured": "ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–33."
},
{
"DOI": "10.1177/2048872617711169",
"author": "N Bréchot",
"doi-asserted-by": "publisher",
"first-page": "62",
"journal-title": "Eur Heart J Acute Cardiovasc Care",
"key": "4616_CR15",
"unstructured": "Bréchot N, Demondion P, Santi F, Lebreton G, Pham T, Dalakidis A, et al. Intra-aortic balloon pump protects against hydrostatic pulmonary oedema during peripheral venoarterial-extracorporeal membrane oxygenation. Eur Heart J Acute Cardiovasc Care. 2018;7:62–9.",
"volume": "7",
"year": "2018"
},
{
"DOI": "10.1016/j.jcrc.2016.02.011",
"author": "H Wang",
"doi-asserted-by": "publisher",
"first-page": "106",
"journal-title": "J Crit Care",
"key": "4616_CR16",
"unstructured": "Wang H, Cui N, Su L, Long Y, Wang X, Zhou X, et al. Prognostic value of extravascular lung water and its potential role in guiding fluid therapy in septic shock after initial resuscitation. J Crit Care. 2016;33:106–13.",
"volume": "33",
"year": "2016"
},
{
"DOI": "10.1186/s13613-020-00775-4",
"doi-asserted-by": "crossref",
"key": "4616_CR17",
"unstructured": "Luyt C-E, Sahnoun T, Gautier M, Vidal P, Burrel S, Pineton de Chambrun M, et al. Ventilator-associated pneumonia in patients with SARS-CoV-2-associated acute respiratory distress syndrome requiring ECMO: a retrospective cohort study. Ann Intensive Care. 2020;10:158."
},
{
"DOI": "10.1056/NEJMoa2015432",
"author": "M Ackermann",
"doi-asserted-by": "publisher",
"first-page": "120",
"journal-title": "N Engl J Med",
"key": "4616_CR18",
"unstructured": "Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020;383:120–8.",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.7326/M20-2003",
"author": "D Wichmann",
"doi-asserted-by": "publisher",
"first-page": "268",
"journal-title": "Ann Intern Med",
"key": "4616_CR19",
"unstructured": "Wichmann D, Sperhake J-P, Lütgehetmann M, Steurer S, Edler C, Heinemann A, et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study. Ann Intern Med. 2020;173:268–77.",
"volume": "173",
"year": "2020"
},
{
"DOI": "10.1126/scitranslmed.abj7790",
"doi-asserted-by": "crossref",
"key": "4616_CR20",
"unstructured": "D’Agnillo F, Walters K-A, Xiao Y, Sheng Z-M, Scherler K, Park J, et al. Lung epithelial and endothelial damage, loss of tissue repair, inhibition of fibrinolysis, and cellular senescence in fatal COVID-19. Sci Transl Med. 2021;13:eabj7790."
},
{
"DOI": "10.1183/13993003.02384-2020",
"author": "L Michalick",
"doi-asserted-by": "publisher",
"first-page": "2002384",
"journal-title": "Eur Respir J",
"key": "4616_CR21",
"unstructured": "Michalick L, Weidenfeld S, Grimmer B, Fatykhova D, Solymosi PD, Behrens F, et al. Plasma mediators in patients with severe COVID-19 cause lung endothelial barrier failure. Eur Respir J. 2021;57:2002384.",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)30937-5",
"author": "Z Varga",
"doi-asserted-by": "publisher",
"first-page": "1417",
"journal-title": "Lancet",
"key": "4616_CR22",
"unstructured": "Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–8.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.050907",
"author": "A Rauch",
"doi-asserted-by": "publisher",
"first-page": "1881",
"journal-title": "Circulation",
"key": "4616_CR23",
"unstructured": "Rauch A, Dupont A, Goutay J, Caplan M, Staessens S, Moussa M, et al. Endotheliopathy Is Induced by Plasma From Critically Ill Patients and Associated With Organ Failure in Severe COVID-19. Circulation. 2020;142:1881–4.",
"volume": "142",
"year": "2020"
},
{
"DOI": "10.1038/s41577-020-0343-0",
"author": "L-A Teuwen",
"doi-asserted-by": "publisher",
"first-page": "389",
"journal-title": "Nat Rev Immunol",
"key": "4616_CR24",
"unstructured": "Teuwen L-A, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat Rev Immunol. 2020;20:389–91.",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/j.devcel.2013.08.020",
"author": "M Giannotta",
"doi-asserted-by": "publisher",
"first-page": "441",
"journal-title": "Dev Cell",
"key": "4616_CR25",
"unstructured": "Giannotta M, Trani M, Dejana E. VE-cadherin and endothelial adherens junctions: active guardians of vascular integrity. Dev Cell. 2013;26:441–54.",
"volume": "26",
"year": "2013"
},
{
"DOI": "10.1097/CCM.0000000000001860",
"author": "S Bergt",
"doi-asserted-by": "publisher",
"first-page": "e988",
"journal-title": "Crit Care Med",
"key": "4616_CR26",
"unstructured": "Bergt S, Gruenewald M, Beltschany C, Grub A, Neumann T, Albrecht M, et al. The Fibrin-Derived Peptide Bβ15-42 (FX06) Ameliorates Vascular Leakage and Improves Survival and Neurocognitive Recovery: Implications From Two Animal Models of Cardiopulmonary Resuscitation. Crit Care Med. 2016;44:e988-995.",
"volume": "44",
"year": "2016"
},
{
"key": "4616_CR27",
"unstructured": "RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report. N Engl J Med. 2020;"
},
{
"DOI": "10.1038/nm1198",
"author": "P Petzelbauer",
"doi-asserted-by": "publisher",
"first-page": "298",
"journal-title": "Nat Med",
"key": "4616_CR28",
"unstructured": "Petzelbauer P, Zacharowski PA, Miyazaki Y, Friedl P, Wickenhauser G, Castellino FJ, et al. The fibrin-derived peptide Bbeta15-42 protects the myocardium against ischemia-reperfusion injury. Nat Med. 2005;11:298–304.",
"volume": "11",
"year": "2005"
},
{
"DOI": "10.1097/01.CCM.0000269035.30231.76",
"author": "JP Roesner",
"doi-asserted-by": "publisher",
"first-page": "1730",
"journal-title": "Crit Care Med",
"key": "4616_CR29",
"unstructured": "Roesner JP, Petzelbauer P, Koch A, Mersmann J, Zacharowski PA, Boehm O, et al. The fibrin-derived peptide Bbeta15-42 is cardioprotective in a pig model of myocardial ischemia-reperfusion injury. Crit Care Med. 2007;35:1730–5.",
"volume": "35",
"year": "2007"
},
{
"DOI": "10.1186/cc9250",
"author": "T Tagami",
"doi-asserted-by": "publisher",
"first-page": "R162",
"journal-title": "Crit Care",
"key": "4616_CR30",
"unstructured": "Tagami T, Kushimoto S, Yamamoto Y, Atsumi T, Tosa R, Matsuda K, et al. Validation of extravascular lung water measurement by single transpulmonary thermodilution: human autopsy study. Crit Care. 2010;14:R162.",
"volume": "14",
"year": "2010"
},
{
"DOI": "10.1186/s13613-021-00965-8",
"author": "J Wollborn",
"doi-asserted-by": "publisher",
"first-page": "175",
"journal-title": "Ann Intensive Care",
"key": "4616_CR31",
"unstructured": "Wollborn J, Hassenzahl LO, Reker D, Staehle HF, Omlor AM, Baar W, et al. Diagnosing capillary leak in critically ill patients: development of an innovative scoring instrument for non-invasive detection. Ann Intensive Care. 2021;11:175.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.jcv.2014.05.001",
"author": "CAM van de Weg",
"doi-asserted-by": "publisher",
"first-page": "328",
"journal-title": "J Clin Virol Off Publ Pan Am Soc Clin Virol",
"key": "4616_CR32",
"unstructured": "van de Weg CAM, Pannuti CS, van den Ham H-J, de Araújo ESA, Boas LSV, Felix AC, et al. Serum angiopoietin-2 and soluble VEGF receptor 2 are surrogate markers for plasma leakage in patients with acute dengue virus infection. J Clin Virol Off Publ Pan Am Soc Clin Virol. 2014;60:328–35.",
"volume": "60",
"year": "2014"
},
{
"DOI": "10.1016/j.cyto.2012.04.002",
"author": "C Clajus",
"doi-asserted-by": "publisher",
"first-page": "352",
"journal-title": "Cytokine",
"key": "4616_CR33",
"unstructured": "Clajus C, Lukasz A, David S, Hertel B, Lichtinghagen R, Parikh SM, et al. Angiopoietin-2 is a potential mediator of endothelial barrier dysfunction following cardiopulmonary bypass. Cytokine. 2012;60:352–9.",
"volume": "60",
"year": "2012"
},
{
"DOI": "10.3390/cells10010186",
"author": "AG Vassiliou",
"doi-asserted-by": "publisher",
"first-page": "186",
"journal-title": "Cells",
"key": "4616_CR34",
"unstructured": "Vassiliou AG, Keskinidou C, Jahaj E, Gallos P, Dimopoulou I, Kotanidou A, et al. ICU Admission Levels of Endothelial Biomarkers as Predictors of Mortality in Critically Ill COVID-19 Patients. Cells. 2021;10:186.",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1186/s13054-021-03499-4",
"author": "S Spadaro",
"doi-asserted-by": "publisher",
"first-page": "74",
"journal-title": "Crit Care",
"key": "4616_CR35",
"unstructured": "Spadaro S, Fogagnolo A, Campo G, Zucchetti O, Verri M, Ottaviani I, et al. Markers of endothelial and epithelial pulmonary injury in mechanically ventilated COVID-19 ICU patients. Crit Care. 2021;25:74.",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1161/ATVBAHA.120.315595",
"author": "A Dupont",
"doi-asserted-by": "publisher",
"first-page": "1760",
"journal-title": "Arterioscler Thromb Vasc Biol",
"key": "4616_CR36",
"unstructured": "Dupont A, Rauch A, Staessens S, Moussa M, Rosa M, Corseaux D, et al. Vascular Endothelial Damage in the Pathogenesis of Organ Injury in Severe COVID-19. Arterioscler Thromb Vasc Biol. 2021;41:1760–73.",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1093/cvr/cvv144",
"author": "S Flemming",
"doi-asserted-by": "publisher",
"first-page": "32",
"journal-title": "Cardiovasc Res",
"key": "4616_CR37",
"unstructured": "Flemming S, Burkard N, Renschler M, Vielmuth F, Meir M, Schick MA, et al. Soluble VE-cadherin is involved in endothelial barrier breakdown in systemic inflammation and sepsis. Cardiovasc Res. 2015;107:32–44.",
"volume": "107",
"year": "2015"
},
{
"DOI": "10.1186/s13054-019-2315-y",
"author": "W-K Yu",
"doi-asserted-by": "publisher",
"first-page": "18",
"journal-title": "Crit Care",
"key": "4616_CR38",
"unstructured": "Yu W-K, McNeil JB, Wickersham NE, Shaver CM, Bastarache JA, Ware LB. Vascular endothelial cadherin shedding is more severe in sepsis patients with severe acute kidney injury. Crit Care. 2019;23:18.",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1186/s13613-021-00890-w",
"author": "G Loosen",
"doi-asserted-by": "publisher",
"first-page": "101",
"journal-title": "Ann Intensive Care",
"key": "4616_CR39",
"unstructured": "Loosen G, Conrad AM, Hagman M, Essert N, Thiel M, Luecke T, et al. Transpulmonary thermodilution in patients treated with veno-venous extracorporeal membrane oxygenation. Ann Intensive Care. 2021;11:101.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1007/s10877-019-00398-6",
"author": "A Herner",
"doi-asserted-by": "publisher",
"first-page": "923",
"journal-title": "J Clin Monit Comput",
"key": "4616_CR40",
"unstructured": "Herner A, Lahmer T, Mayr U, Rasch S, Schneider J, Schmid RM, et al. Transpulmonary thermodilution before and during veno-venous extra-corporeal membrane oxygenation ECMO: an observational study on a potential loss of indicator into the extra-corporeal circuit. J Clin Monit Comput. 2020;34:923–36.",
"volume": "34",
"year": "2020"
}
],
"reference-count": 40,
"references-count": 40,
"relation": {},
"resource": {
"primary": {
"URL": "https://ccforum.biomedcentral.com/articles/10.1186/s13054-023-04616-1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "FX06 to rescue SARS-CoV-2-induced acute respiratory distress syndrome: a randomized clinical trial",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "27"
}