High risk of malnutrition among hospitalised coronavirus disease 2019 (COVID-19) patients is associated with mortality and other clinical outcomes
et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2024.02.023, Mar 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
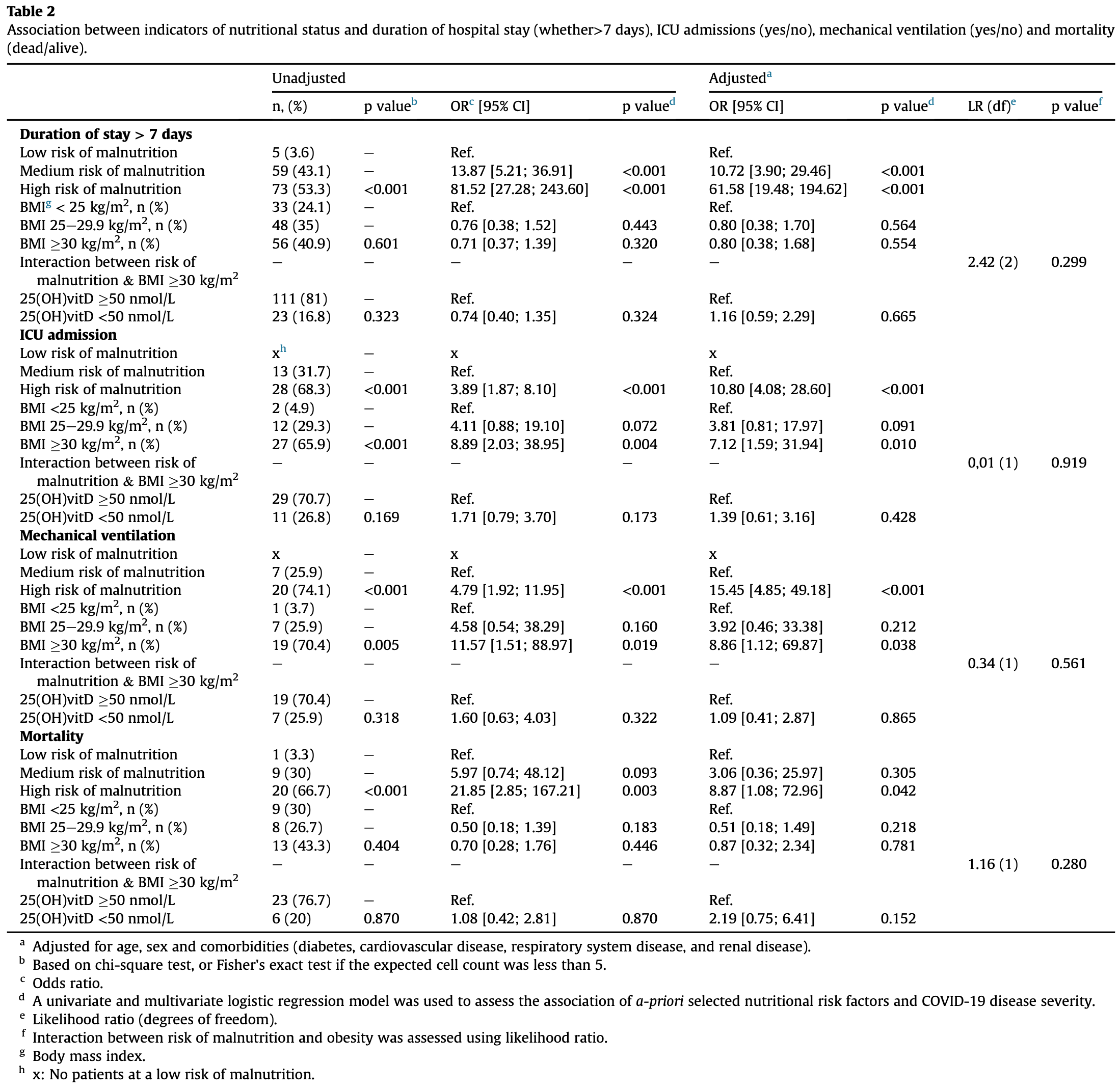
Retrospective 273 hospitalized COVID-19 patients in Iceland showing high risk of malnutrition associated with ICU admission, mechanical ventilation, and mortality. Mortality was higher with vitamin D insufficiency, but this result was not statistically significant.
This is the 195th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 54.3% lower, OR 0.46, p = 0.15, high D levels (≥50nmol/L) 221, low D levels (<50nmol/L) 52, adjusted per study, inverted to make OR<1 favor high D levels (≥50nmol/L), multivariable, RR approximated with OR.
|
|
risk of mechanical ventilation, 8.3% lower, OR 0.92, p = 0.86, high D levels (≥50nmol/L) 221, low D levels (<50nmol/L) 52, adjusted per study, inverted to make OR<1 favor high D levels (≥50nmol/L), multivariable, RR approximated with OR.
|
|
risk of ICU admission, 28.1% lower, OR 0.72, p = 0.43, high D levels (≥50nmol/L) 221, low D levels (<50nmol/L) 52, adjusted per study, inverted to make OR<1 favor high D levels (≥50nmol/L), multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Guðnadóttir et al., 4 Mar 2024, retrospective, Iceland, peer-reviewed, 4 authors, study period February 2020 - March 2021.
Contact: sandradg@landspitali.is.
High risk of malnutrition among hospitalised coronavirus disease 2019 (COVID-19) patients is associated with mortality and other clinical outcomes
Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2024.02.023
Introduction: Increasing evidence indicates an association between nutritional status and Coronavirus disease 2019 (COVID-19) disease severity. The aim of the study was to describe the risk of malnutrition, body mass index (BMI) and vitamin D status of hospitalised COVID-19 patients and assess whether they are associated with duration of hospital stay, intensive care unit (ICU) admission, mechanical ventilation, and mortality. Methods: The study is a descriptive retrospective study of 273 patients with COVID-19 admitted to Hospital from February 2020 to March 2021. Patients were screened for risk of malnutrition using a validated screening tool. BMI was calculated from height and weight. Insufficient Vitamin D status was defined as 25(OH)vitD <50 nmol/L. Logistic regression analysis was used to assess the association between indicators of nutritional status of patients with COVID-19, and outcomes such as duration of stay >7 days, ICU admission, mechanical ventilation, and mortality. Interaction between risk of malnutrition and BMI of 30 kg/m 2 was assessed using the likelihood ratio test with hospital stay, ICU admission, mechanical ventilation, and mortality as outcomes. Results: Screening for risk of malnutrition identified 201 (74%) patients at a medium to high risk of malnutrition. Patients defined as being at a medium or high risk of malnutrition were more likely to be hospitalised for >7 days compared to those defined as low risk (OR: 10.72; 95% CI: 3.9e29.46; p < 0.001 and OR: 61.57; 95% CI: 19.48e194.62; p < 0.001, respectively). All patients who were admitted to ICU (n ¼ 41) and required mechanical ventilation (n ¼ 27) were defined as having medium or high risk of malnutrition. High risk of malnutrition was also associated with increased odds of mortality (OR: 8.87; 955 CI 1.08e72,96; p ¼ 0.042). BMI of 30 kg/m 2 (43%) and 25(OH)vitD <50 nmol/L (20%) were not associated with duration of stay >7 days or mortality, although BMI 30 kg/m 2 was associated with increased risk of ICU admission (OR: 7.12; 95% CI: 1.59e31.94; p ¼ 0.010) and mechanical ventilation (OR: 8.86; 95% CI: 1.12e69.87; p ¼ 0.038). Interactions between risk of malnutrition and BMI 30 kg/m 2 were not significant to explain the outcomes of hospital stay >7 days, ICU admission, mechanical ventilation, or mortality. Conclusion: High risk of malnutrition among hospitalised COVID-19 patients was associated with longer duration of hospital stay, ICU admission, mechanical ventilation and mortality, and BMI 30 kg/m 2 was associated with ICU admission and mechanical ventilation. Insufficient Vitamin D status was not associated with duration of hospital stay, ICU admission, mechanical ventilation, or mortality.
Author contribution Sandra D€ ogg Guðnad ottir: Formal analysis, Investigation, Writing-Original Draft, Visualization, Funding acquisition. Ar ora R os Ingad ottir: Conceptualization, Methodology, Writing e Review and Editing, Visualization, Supervision, Funding acquisition. Ingibj€ org Gunnarsd ottir: Writing e Review and Editing, Visualization, Supervision, Funding acquisition. Ubaldo Benitez Hernandez: Statistical consulting.
Declaration of competing interest The authors have no conflict of interest to declare.
Appendix A. Supplementary data Supplementary data to this article can be found online at https://doi.org/10.1016/j.clnesp.2024.02.023.
References
Abate, Chekole, Estifanos, Abate, Kabthymer, Prevalence and outcomes of malnutrition among hospitalized COVID-19 patients: a systematic review and meta-analysis, Clin Nutr ESPEN
Afaghi, Tarki, Rahimi, Besharat, Mirhaidari et al., Prevalence and clinical outcomes of vitamin D deficiency in COVID-19 hospitalized patients: a retrospective single-center analysis, Tohoku J Exp Med
Alwarawrah, Kiernan, Maciver, Changes in nutritional status impact immune cell metabolism and function, Front Immunol
Anker, Landmesser, Haehling, Butler, Coats et al., Weight loss, malnutrition, and cachexia in COVID-19: facts and numbers, J Cachexia Sarcopenia Muscle
Antwi, Appiah, Oluwakuse, Abu, The nutrition-COVID-19 interplay: a review, Curr Nutr Rep
Badosa, Tahull, Casas, Sangrador, Faz M Endez et al., Hospital malnutrition screening at admission: malnutrition increases mortality and length of stay, Nutr Hosp
Booth, Reed, Ponzo, Yassaee, Aral et al., Population risk factors for severe disease and mortality in COVID-19: a global systematic review and meta-analysis, PLoS One
Bourke, Berkley, Prendergast, Immune dysfunction as a cause and consequence of malnutrition, Trends Immunol
Cai, Yang, Zhang, Obesity is associated with severe disease and mortality in patients with coronavirus disease 2019 (COVID-19): a meta-analysis, BMC Publ Health
Cederholm, Jensen, Correia, Gonzalez, Fukushima et al., GLIM criteria for the diagnosis of malnutrition -a consensus report from the global clinical nutrition community, J Cachexia Sarcopenia Muscle
Chew, Kattainen, Haase, Buanes, Kristinsdottir et al., A descriptive study of the surge response and outcomes of ICU patients with COVID-19 during first wave in Nordic countries, Acta Anaesthesiol Scand
Dana, Bannay, Bourst, Ziegler, Losser et al., Obesity and mortality in critically ill COVID-19 patients with respiratory failure, Int J Obes
De Siqueira, Almeida, Zica, Brum, Barcel O A et al., Impact of obesity on hospitalizations and mortality, due to COVID-19: a systematic review, Obes Res Clin Pract
Deer, Hosein, Harvey, Nguyen, Givan et al., Impact of COVID-19 infection and persistent lingering symptoms on patient reported indicators of nutritional risk and malnutrition, Nutrients
Deng, Zhang, Wang, Chen, Obesity is associated with severe COVID-19 but not death: a dose-response meta-analysis, Epidemiol Infect
Dhama, Khan, Tiwari, Sircar, Bhat et al., Coronavirus disease 2019-COVID-19, Clin Microbiol Rev
Dissanayake, Silva, Sumanatilleke, De Silva, Gamage et al., Prognostic and therapeutic role of vitamin D in COVID-19: systematic review and meta-analysis, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab892
Ebrahimzadeh, Mohseni, Narimani, Ebrahimzadeh, Kazemi et al., Association between vitamin D status and risk of covid-19 in-hospital mortality: a systematic review and meta-analysis of observational studies, Crit Rev Food Sci Nutr
Erdfelder, Faul, Buchner, GPOWER: a general power analysis program, Behav Res Methods Instrum Comput
Faul, Erdfelder, Lang, Buchner, Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences, Behav Res Methods
Gerriets, Maciver, Role of T cells in malnutrition and obesity, Front Immunol
Gudbjartsson, Helgason, Jonsson, Magnusson, Melsted et al., Spread of SARS-CoV-2 in the Icelandic population, N Engl J Med
Helvaci, Eyupoglu, Karabulut, Yildiz, Prevalence of obesity and its impact on outcome in patients with COVID-19: a systematic review and metaanalysis, Front Endocrinol
Hern Andez, Nan, Fernandez-Ayala, García-Unzueta, Hern Andez-Hern Andez et al., Vitamin D status in hospitalized patients with SARS-CoV-2 infection, J Clin Endocrinol Metabol
Hu, Deng, Wang, Chen, Gu et al., Predictive value of the prognostic nutritional index for the severity of coronavirus disease 2019, Nutrition
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat Rev Microbiol
Huang, Lu, Huang, Wang, Ling et al., Obesity in patients with COVID-19: a systematic review and meta-analysis, Metabolism
Ingadottir, Beck, Baldwin, Weekes, Geirsdottir et al., Two components of the new ESPEN diagnostic criteria for malnutrition are independent predictors of lung function in hospitalized patients with chronic obstructive pulmonary disease (COPD), Clin Nutr
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci Rep
Karahan, Katkat, Impact of serum 25(OH) vitamin D level on mortality in patients with COVID-19 in Turkey, J Nutr Health Aging
Kashif, Chaudhry, Fayyaz, Abdullah, Malik et al., Follow-up of COVID-19 recovered patients with mild disease, Sci Rep
Kristinsson, Kristinsdottir, Blondal, Thormar, Kristjansson et al., Nationwide incidence and outcomes of patients with coronavirus disease 2019 requiring intensive care in Iceland, Crit Care Med
Li, Ashcroft, Chung, Dighero, Dozier et al., Risk factors for poor outcomes in hospitalised COVID-19 patients: a systematic review and meta-analysis, J Glob Health
Li, Zhu, Zhang, Liu, Ji et al., Nutritional status is closely related to the severity of COVID-19: a multi-center retrospective study, J Infect Dev Ctries
Liu, Cong, Wang, Mei, Peng et al., Risk of malnutrition is common in patients with coronavirus disease 2019 (COVID-19) in wuhan, China: a cross-sectional study, J Nutr
Liu, Zhou, Wang, Wang, Qu et al., Malnutrition is associated with hyperinflammation and immunosuppression in COVID-19 patients: a prospective observational study, Nutr Clin Pract
Mertens, Peñalvo, The burden of malnutrition and fatal COVID-19: a global burden of disease analysis, Front Nutr
Moriconi, Masi, Rebelos, Virdis, Manca et al., Obesity prolongs the hospital stay in patients affected by COVID-19, and may impact on SARS-COV-2 shedding, Obes Res Clin Pract
Myoung, Two years of COVID-19 pandemic: where are we now?, J Microbiol
Nair, Maseeh, Vitamin D: the "sunshine" vitamin, J Pharmacol Pharmacother
Palaiodimos, Kokkinidis, Li, Karamanis, Ognibene et al., Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York, Metabolism
Pettit, Mackenzie, Ridgway, Pursell, Ash et al., Obesity is associated with increased risk for mortality among hospitalized patients with COVID-19, Obesity
Popkin, Corvalan, Grummer-Strawn, Dynamics of the double burden of malnutrition and the changing nutrition reality, Lancet
Riesgo, Castro, Del Amo, Ceferino, Izaola et al., Prevalence of risk of malnutrition and risk of sarcopenia in a reference hospital for COVID-19: relationship with mortality, Ann Nutr Metabol
Savino, Dardenne, Velloso, Silva-Barbosa, The thymus is a common target in malnutrition and infection, Br J Nutr
Sigurdardottir, Sigurdsson, Olafsson, Sverrisdottir, Gunnarsdottir et al., Prevalence of modifiable risk factors in primary elective arthroplasty and their association with infections, Acta Orthop
Simonnet, Chetboun, Poissy, Raverdy, Noulette et al., High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obesity
Sj€ Ogren, Stenberg, Thuccani, Martikainen, Rylander et al., Impact of obesity on intensive care outcomes in patients with COVID-19 in Sweden-A cohort study, PLoS One
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH) D level on hospital admission associated with COVID-19 stage and mortality, Am J Clin Pathol
Sooriyaarachchi, Jeyakumar, King, Jayawardena, Impact of vitamin D deficiency on COVID-19, Clin Nutr ESPEN
Statacorp, Stata statistical software: release
Stefano, Emanuela, Daniela, Malnutrition risk as a negative prognostic factor in COVID-19 patients, Clin Nutr ESPEN
Steinberg, Wright, Kushner, In young adults with COVID-19, obesity is associated with adverse outcomes, West J Emerg Med
Thorsd Ottir, Eriksen, Eysteinsd Ottir S, Nutritional status at submission for dietetic services and screening for malnutrition at admission to hospital, Clin Nutr
Thorsdottir, Gunnarsdottir, Eriksen, Screening method evaluated by nutritional status measurements can be used to detect malnourishment in chronic obstructive pulmonary disease, J Am Diet Assoc
Venter, Eyerich, Sarin, Klatt, Nutrition and the immune system: a complicated tango, Nutrients
Wang, Li, Wang, Sarcopenia: an underlying treatment target during the COVID-19 pandemic, Nutrition
Wei, Liu, Li, Zhang, Zhong et al., Evaluation of the nutritional status in patients with COVID-19, J Clin Biochem Nutr
Wierdsma, Kruizenga, Konings, Krebbers, Jorissen et al., Poor nutritional status, risk of sarcopenia and nutrition related complaints are prevalent in COVID-19 patients during and after hospital admission, Clin Nutr ESPEN
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention, JAMA
Yisak, Ewunetei, Kefale, Mamuye, Teshome et al., Effects of vitamin D on COVID-19 infection and prognosis: a systematic review, Risk Manag Healthc Pol
Yu, Ye, Chen, Jiang, Lu, Malnutrition prolongs the hospitalization of patients with COVID-19 infection: a clinical epidemiological analysis, J Nutr Health Aging
Zabetakis, Lordan, Norton, Tsoupras, COVID-19: the inflammation link and the role of nutrition in potential mitigation, Nutrients
Zeng, Cao, Ma, Chen, Shi et al., Appetite loss, death anxiety and medical coping modes in COVID-19 patients: a cross-sectional study, Nurs Open
Zhang, Lewis, Moley, Brestoff, A systematic review and metaanalysis of obesity and COVID-19 outcomes, Sci Rep
Zhou, Ma, Liu, Xiang, Tao et al., A correlation analysis between the nutritional status and prognosis of COVID-19 patients, J Nutr Health Aging
Zmijewski, Vitamin D and human health, Int J Mol Sci
DOI record:
{
"DOI": "10.1016/j.clnesp.2024.02.023",
"ISSN": [
"2405-4577"
],
"URL": "http://dx.doi.org/10.1016/j.clnesp.2024.02.023",
"alternative-id": [
"S2405457724000469"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "High risk of malnutrition among hospitalised coronavirus disease 2019 (COVID-19) patients is associated with mortality and other clinical outcomes"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Clinical Nutrition ESPEN"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.clnesp.2024.02.023"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2024 The Author(s). Published by Elsevier Ltd on behalf of European Society for Clinical Nutrition and Metabolism."
}
],
"author": [
{
"ORCID": "http://orcid.org/0009-0000-4147-4980",
"affiliation": [],
"authenticated-orcid": false,
"family": "Guðnadóttir",
"given": "Sandra Dögg",
"sequence": "first"
},
{
"affiliation": [],
"family": "Gunnarsdóttir",
"given": "Ingibjörg",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5214-8141",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hernandez",
"given": "Ubaldo Benitez",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4593-3739",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ingadóttir",
"given": "Áróra Rós",
"sequence": "additional"
}
],
"container-title": "Clinical Nutrition ESPEN",
"container-title-short": "Clinical Nutrition ESPEN",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.com.au",
"clinicalkey.es",
"clinicalkey.com",
"clinicalnutritionespen.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2024,
3,
4
]
],
"date-time": "2024-03-04T08:01:16Z",
"timestamp": 1709539276000
},
"deposited": {
"date-parts": [
[
2024,
3,
11
]
],
"date-time": "2024-03-11T03:06:58Z",
"timestamp": 1710126418000
},
"funder": [
{
"DOI": "10.13039/501100005415",
"doi-asserted-by": "publisher",
"name": "University of Iceland"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
12
]
],
"date-time": "2024-03-12T00:23:03Z",
"timestamp": 1710202983531
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
6
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
6,
1
]
],
"date-time": "2024-06-01T00:00:00Z",
"timestamp": 1717200000000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
2,
26
]
],
"date-time": "2024-02-26T00:00:00Z",
"timestamp": 1708905600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2405457724000469?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2405457724000469?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "1-7",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2024,
6
]
]
},
"published-print": {
"date-parts": [
[
2024,
6
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1128/CMR.00028-20",
"article-title": "Coronavirus disease 2019-COVID-19",
"author": "Dhama",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "Clin Microbiol Rev",
"key": "10.1016/j.clnesp.2024.02.023_bib1",
"volume": "33",
"year": "2020"
},
{
"article-title": "Two years of COVID-19 pandemic: where are we now?",
"author": "Myoung",
"first-page": "235",
"issue": "3",
"journal-title": "J Microbiol",
"key": "10.1016/j.clnesp.2024.02.023_bib2",
"volume": "60",
"year": "2022"
},
{
"author": "The Directorate of Health",
"key": "10.1016/j.clnesp.2024.02.023_bib3",
"series-title": "Iceland: COVID-19 in Iceland - statistics",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2006100",
"article-title": "Spread of SARS-CoV-2 in the Icelandic population",
"author": "Gudbjartsson",
"doi-asserted-by": "crossref",
"first-page": "2302",
"issue": "24",
"journal-title": "N Engl J Med",
"key": "10.1016/j.clnesp.2024.02.023_bib4",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"article-title": "Characteristics of SARS-CoV-2 and COVID-19",
"author": "Hu",
"doi-asserted-by": "crossref",
"first-page": "141",
"issue": "3",
"journal-title": "Nat Rev Microbiol",
"key": "10.1016/j.clnesp.2024.02.023_bib5",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.2648",
"article-title": "Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "1239",
"issue": "13",
"journal-title": "JAMA",
"key": "10.1016/j.clnesp.2024.02.023_bib6",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0247461",
"article-title": "Population risk factors for severe disease and mortality in COVID-19: a global systematic review and meta-analysis",
"author": "Booth",
"doi-asserted-by": "crossref",
"issue": "3",
"journal-title": "PLoS One",
"key": "10.1016/j.clnesp.2024.02.023_bib7",
"volume": "16",
"year": "2021"
},
{
"article-title": "Risk factors for poor outcomes in hospitalised COVID-19 patients: a systematic review and meta-analysis",
"author": "Li",
"journal-title": "J Glob Health",
"key": "10.1016/j.clnesp.2024.02.023_bib8",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.clnesp.2021.03.002",
"article-title": "Prevalence and outcomes of malnutrition among hospitalized COVID-19 patients: a systematic review and meta-analysis",
"author": "Abate",
"doi-asserted-by": "crossref",
"first-page": "174",
"journal-title": "Clin Nutr ESPEN",
"key": "10.1016/j.clnesp.2024.02.023_bib9",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.1016/j.clnesp.2021.07.016",
"article-title": "Malnutrition risk as a negative prognostic factor in COVID-19 patients",
"author": "Stefano",
"doi-asserted-by": "crossref",
"first-page": "369",
"journal-title": "Clin Nutr ESPEN",
"key": "10.1016/j.clnesp.2024.02.023_bib10",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.3390/nu12030818",
"article-title": "Nutrition and the immune system: a complicated tango",
"author": "Venter",
"doi-asserted-by": "crossref",
"first-page": "818",
"issue": "3",
"journal-title": "Nutrients",
"key": "10.1016/j.clnesp.2024.02.023_bib11",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/nu12051466",
"article-title": "COVID-19: the inflammation link and the role of nutrition in potential mitigation",
"author": "Zabetakis",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Nutrients",
"key": "10.1016/j.clnesp.2024.02.023_bib12",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1007/s12603-020-1457-6",
"article-title": "A correlation analysis between the nutritional status and prognosis of COVID-19 patients",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "84",
"issue": "1",
"journal-title": "J Nutr Health Aging",
"key": "10.1016/j.clnesp.2024.02.023_bib13",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1016/j.metabol.2020.154378",
"article-title": "Obesity in patients with COVID-19: a systematic review and meta-analysis",
"author": "Huang",
"doi-asserted-by": "crossref",
"journal-title": "Metabolism",
"key": "10.1016/j.clnesp.2024.02.023_bib14",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1016/j.clnesp.2021.05.011",
"article-title": "Impact of vitamin D deficiency on COVID-19",
"author": "Sooriyaarachchi",
"doi-asserted-by": "crossref",
"first-page": "372",
"journal-title": "Clin Nutr ESPEN",
"key": "10.1016/j.clnesp.2024.02.023_bib15",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.3855/jidc.14178",
"article-title": "Nutritional status is closely related to the severity of COVID-19: a multi-center retrospective study",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "490",
"issue": "4",
"journal-title": "J Infect Dev Ctries",
"key": "10.1016/j.clnesp.2024.02.023_bib16",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1017/S0950268820003179",
"article-title": "Obesity is associated with severe COVID-19 but not death: a dose-response meta-analysis",
"author": "Deng",
"doi-asserted-by": "crossref",
"first-page": "e144",
"journal-title": "Epidemiol Infect",
"key": "10.1016/j.clnesp.2024.02.023_bib17",
"volume": "149",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgab892",
"article-title": "Prognostic and therapeutic role of vitamin D in COVID-19: systematic review and meta-analysis",
"author": "Dissanayake",
"doi-asserted-by": "crossref",
"first-page": "1484",
"issue": "5",
"journal-title": "J Clin Endocrinol Metab",
"key": "10.1016/j.clnesp.2024.02.023_bib18",
"volume": "107",
"year": "2022"
},
{
"DOI": "10.3389/fendo.2021.598249",
"article-title": "Prevalence of obesity and its impact on outcome in patients with COVID-19: a systematic review and meta-analysis",
"author": "Helvaci",
"doi-asserted-by": "crossref",
"journal-title": "Front Endocrinol",
"key": "10.1016/j.clnesp.2024.02.023_bib19",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"article-title": "Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers",
"author": "Jain",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "Sci Rep",
"key": "10.1016/j.clnesp.2024.02.023_bib20",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1620/tjem.255.127",
"article-title": "Prevalence and clinical outcomes of vitamin D deficiency in COVID-19 hospitalized patients: a retrospective single-center analysis",
"author": "Afaghi",
"doi-asserted-by": "crossref",
"first-page": "127",
"issue": "2",
"journal-title": "Tohoku J Exp Med",
"key": "10.1016/j.clnesp.2024.02.023_bib21",
"volume": "255",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgaa733",
"article-title": "Vitamin D status in hospitalized patients with SARS-CoV-2 infection",
"author": "Hernández",
"doi-asserted-by": "crossref",
"first-page": "e1343",
"issue": "3",
"journal-title": "J Clin Endocrinol Metabol",
"key": "10.1016/j.clnesp.2024.02.023_bib22",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1111/aas.13983",
"article-title": "A descriptive study of the surge response and outcomes of ICU patients with COVID-19 during first wave in Nordic countries",
"author": "Chew",
"doi-asserted-by": "crossref",
"first-page": "56",
"issue": "1",
"journal-title": "Acta Anaesthesiol Scand",
"key": "10.1016/j.clnesp.2024.02.023_bib23",
"volume": "66",
"year": "2022"
},
{
"DOI": "10.1097/CCM.0000000000004582",
"article-title": "Nationwide incidence and outcomes of patients with coronavirus disease 2019 requiring intensive care in Iceland",
"author": "Kristinsson",
"doi-asserted-by": "crossref",
"first-page": "e1102",
"issue": "11",
"journal-title": "Crit Care Med",
"key": "10.1016/j.clnesp.2024.02.023_bib24",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.1016/S0261-5614(99)80044-2",
"article-title": "Nutritional status at submission for dietetic services and screening for malnutrition at admission to hospital",
"author": "Thorsdóttir",
"doi-asserted-by": "crossref",
"first-page": "15",
"issue": "1",
"journal-title": "Clin Nutr",
"key": "10.1016/j.clnesp.2024.02.023_bib25",
"volume": "18",
"year": "1999"
},
{
"DOI": "10.1016/j.clnu.2017.05.031",
"article-title": "Two components of the new ESPEN diagnostic criteria for malnutrition are independent predictors of lung function in hospitalized patients with chronic obstructive pulmonary disease (COPD)",
"author": "Ingadottir",
"doi-asserted-by": "crossref",
"first-page": "1323",
"issue": "4",
"journal-title": "Clin Nutr",
"key": "10.1016/j.clnesp.2024.02.023_bib26",
"volume": "37",
"year": "2018"
},
{
"DOI": "10.1016/S0002-8223(01)00163-8",
"article-title": "Screening method evaluated by nutritional status measurements can be used to detect malnourishment in chronic obstructive pulmonary disease",
"author": "Thorsdottir",
"doi-asserted-by": "crossref",
"first-page": "648",
"issue": "6",
"journal-title": "J Am Diet Assoc",
"key": "10.1016/j.clnesp.2024.02.023_bib27",
"volume": "101",
"year": "2001"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"article-title": "Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality",
"author": "De Smet",
"doi-asserted-by": "crossref",
"first-page": "381",
"issue": "3",
"journal-title": "Am J Clin Pathol",
"key": "10.1016/j.clnesp.2024.02.023_bib28",
"volume": "155",
"year": "2021"
},
{
"DOI": "10.1007/s12603-020-1479-0",
"article-title": "Impact of serum 25(OH) vitamin D level on mortality in patients with COVID-19 in Turkey",
"author": "Karahan",
"doi-asserted-by": "crossref",
"first-page": "189",
"issue": "2",
"journal-title": "J Nutr Health Aging",
"key": "10.1016/j.clnesp.2024.02.023_bib29",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.3758/BF03193146",
"article-title": "∗Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences",
"author": "Faul",
"doi-asserted-by": "crossref",
"first-page": "175",
"issue": "2",
"journal-title": "Behav Res Methods",
"key": "10.1016/j.clnesp.2024.02.023_bib30",
"volume": "39",
"year": "2007"
},
{
"DOI": "10.3758/BF03203630",
"article-title": "GPOWER: a general power analysis program",
"author": "Erdfelder",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Behav Res Methods Instrum Comput",
"key": "10.1016/j.clnesp.2024.02.023_bib31",
"volume": "28",
"year": "1996"
},
{
"article-title": "Hospital malnutrition screening at admission: malnutrition increases mortality and length of stay",
"author": "Leiva Badosa",
"first-page": "907",
"issue": "4",
"journal-title": "Nutr Hosp",
"key": "10.1016/j.clnesp.2024.02.023_bib32",
"volume": "34",
"year": "2017"
},
{
"key": "10.1016/j.clnesp.2024.02.023_bib33",
"series-title": "jamovi",
"year": "2022"
},
{
"key": "10.1016/j.clnesp.2024.02.023_bib34",
"volume": "vol. 17",
"year": "2021"
},
{
"article-title": "Risk of malnutrition is common in patients with coronavirus disease 2019 (COVID-19) in wuhan, China: a cross-sectional study",
"author": "Liu",
"first-page": "1591",
"issue": "6",
"journal-title": "J Nutr",
"key": "10.1016/j.clnesp.2024.02.023_bib35",
"volume": "151",
"year": "2021"
},
{
"DOI": "10.1159/000519485",
"article-title": "Prevalence of risk of malnutrition and risk of sarcopenia in a reference hospital for COVID-19: relationship with mortality",
"author": "Riesgo",
"doi-asserted-by": "crossref",
"first-page": "324",
"issue": "6",
"journal-title": "Ann Nutr Metabol",
"key": "10.1016/j.clnesp.2024.02.023_bib36",
"volume": "77",
"year": "2021"
},
{
"DOI": "10.1007/s12603-020-1541-y",
"article-title": "Malnutrition prolongs the hospitalization of patients with COVID-19 infection: a clinical epidemiological analysis",
"author": "Yu",
"doi-asserted-by": "crossref",
"first-page": "369",
"issue": "3",
"journal-title": "J Nutr Health Aging",
"key": "10.1016/j.clnesp.2024.02.023_bib37",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1016/j.nut.2020.111123",
"article-title": "Predictive value of the prognostic nutritional index for the severity of coronavirus disease 2019",
"author": "Hu",
"doi-asserted-by": "crossref",
"journal-title": "Nutrition",
"key": "10.1016/j.clnesp.2024.02.023_bib38",
"volume": "84",
"year": "2021"
},
{
"DOI": "10.3164/jcbn.20-91",
"article-title": "Evaluation of the nutritional status in patients with COVID-19",
"author": "Wei",
"doi-asserted-by": "crossref",
"first-page": "116",
"issue": "2",
"journal-title": "J Clin Biochem Nutr",
"key": "10.1016/j.clnesp.2024.02.023_bib39",
"volume": "67",
"year": "2020"
},
{
"DOI": "10.1016/j.clnesp.2021.03.021",
"article-title": "Poor nutritional status, risk of sarcopenia and nutrition related complaints are prevalent in COVID-19 patients during and after hospital admission",
"author": "Wierdsma",
"doi-asserted-by": "crossref",
"first-page": "369",
"journal-title": "Clin Nutr ESPEN",
"key": "10.1016/j.clnesp.2024.02.023_bib40",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2018.01055",
"article-title": "Changes in nutritional status impact immune cell metabolism and function",
"author": "Alwarawrah",
"doi-asserted-by": "crossref",
"first-page": "1055",
"journal-title": "Front Immunol",
"key": "10.1016/j.clnesp.2024.02.023_bib41",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1017/S0007114507832880",
"article-title": "The thymus is a common target in malnutrition and infection",
"author": "Savino",
"doi-asserted-by": "crossref",
"first-page": "S11",
"issue": "S1",
"journal-title": "Br J Nutr",
"key": "10.1016/j.clnesp.2024.02.023_bib42",
"volume": "98",
"year": "2007"
},
{
"DOI": "10.3389/fimmu.2014.00379",
"article-title": "Role of T cells in malnutrition and obesity",
"author": "Gerriets",
"doi-asserted-by": "crossref",
"first-page": "379",
"journal-title": "Front Immunol",
"key": "10.1016/j.clnesp.2024.02.023_bib43",
"volume": "5",
"year": "2014"
},
{
"DOI": "10.1002/ncp.10679",
"article-title": "Malnutrition is associated with hyperinflammation and immunosuppression in COVID-19 patients: a prospective observational study",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "863",
"issue": "4",
"journal-title": "Nutr Clin Pract",
"key": "10.1016/j.clnesp.2024.02.023_bib44",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1016/j.nut.2020.111104",
"article-title": "Sarcopenia: an underlying treatment target during the COVID-19 pandemic",
"author": "Wang",
"doi-asserted-by": "crossref",
"journal-title": "Nutrition",
"key": "10.1016/j.clnesp.2024.02.023_bib45",
"volume": "84",
"year": "2021"
},
{
"DOI": "10.1002/jcsm.12674",
"article-title": "Weight loss, malnutrition, and cachexia in COVID-19: facts and numbers",
"author": "Anker",
"doi-asserted-by": "crossref",
"first-page": "9",
"issue": "1",
"journal-title": "J Cachexia Sarcopenia Muscle",
"key": "10.1016/j.clnesp.2024.02.023_bib46",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.it.2016.04.003",
"article-title": "Immune dysfunction as a cause and consequence of malnutrition",
"author": "Bourke",
"doi-asserted-by": "crossref",
"first-page": "386",
"issue": "6",
"journal-title": "Trends Immunol",
"key": "10.1016/j.clnesp.2024.02.023_bib47",
"volume": "37",
"year": "2016"
},
{
"DOI": "10.1002/nop2.1037",
"article-title": "Appetite loss, death anxiety and medical coping modes in COVID-19 patients: a cross-sectional study",
"author": "Zeng",
"doi-asserted-by": "crossref",
"first-page": "3242",
"issue": "6",
"journal-title": "Nurs Open",
"key": "10.1016/j.clnesp.2024.02.023_bib48",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-92717-8",
"article-title": "Follow-up of COVID-19 recovered patients with mild disease",
"author": "Kashif",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "Sci Rep",
"key": "10.1016/j.clnesp.2024.02.023_bib49",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3390/nu14030642",
"article-title": "Impact of COVID-19 infection and persistent lingering symptoms on patient reported indicators of nutritional risk and malnutrition",
"author": "Deer",
"doi-asserted-by": "crossref",
"first-page": "642",
"issue": "3",
"journal-title": "Nutrients",
"key": "10.1016/j.clnesp.2024.02.023_bib50",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1002/oby.22941",
"article-title": "Obesity is associated with increased risk for mortality among hospitalized patients with COVID-19",
"author": "Pettit",
"doi-asserted-by": "crossref",
"first-page": "1806",
"issue": "10",
"journal-title": "Obesity",
"key": "10.1016/j.clnesp.2024.02.023_bib51",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1002/oby.22831",
"article-title": "High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation",
"author": "Simonnet",
"doi-asserted-by": "crossref",
"first-page": "1195",
"issue": "7",
"journal-title": "Obesity",
"key": "10.1016/j.clnesp.2024.02.023_bib52",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0257891",
"article-title": "Impact of obesity on intensive care outcomes in patients with COVID-19 in Sweden-A cohort study",
"author": "Sjögren",
"doi-asserted-by": "crossref",
"issue": "10",
"journal-title": "PLoS One",
"key": "10.1016/j.clnesp.2024.02.023_bib53",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-86694-1",
"article-title": "A systematic review and meta-analysis of obesity and COVID-19 outcomes",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "7193",
"issue": "1",
"journal-title": "Sci Rep",
"key": "10.1016/j.clnesp.2024.02.023_bib54",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.5811/westjem.2020.5.47972",
"article-title": "In young adults with COVID-19, obesity is associated with adverse outcomes",
"author": "Steinberg",
"doi-asserted-by": "crossref",
"first-page": "752",
"issue": "4",
"journal-title": "West J Emerg Med",
"key": "10.1016/j.clnesp.2024.02.023_bib55",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2020.154262",
"article-title": "Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York",
"author": "Palaiodimos",
"doi-asserted-by": "crossref",
"journal-title": "Metabolism",
"key": "10.1016/j.clnesp.2024.02.023_bib56",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.1016/j.orcp.2020.05.009",
"article-title": "Obesity prolongs the hospital stay in patients affected by COVID-19, and may impact on SARS-COV-2 shedding",
"author": "Moriconi",
"doi-asserted-by": "crossref",
"first-page": "205",
"issue": "3",
"journal-title": "Obes Res Clin Pract",
"key": "10.1016/j.clnesp.2024.02.023_bib57",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.orcp.2020.07.005",
"article-title": "Impact of obesity on hospitalizations and mortality, due to COVID-19: a systematic review",
"author": "de Siqueira",
"doi-asserted-by": "crossref",
"first-page": "398",
"issue": "5",
"journal-title": "Obes Res Clin Pract",
"key": "10.1016/j.clnesp.2024.02.023_bib58",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1038/s41366-021-00872-9",
"article-title": "Obesity and mortality in critically ill COVID-19 patients with respiratory failure",
"author": "Dana",
"doi-asserted-by": "crossref",
"first-page": "2028",
"issue": "9",
"journal-title": "Int J Obes",
"key": "10.1016/j.clnesp.2024.02.023_bib59",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.1186/s12889-021-11546-6",
"article-title": "Obesity is associated with severe disease and mortality in patients with coronavirus disease 2019 (COVID-19): a meta-analysis",
"author": "Cai",
"doi-asserted-by": "crossref",
"first-page": "1505",
"issue": "1",
"journal-title": "BMC Publ Health",
"key": "10.1016/j.clnesp.2024.02.023_bib60",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.2340/17453674.2023.8480",
"article-title": "Prevalence of modifiable risk factors in primary elective arthroplasty and their association with infections",
"author": "Sigurdardottir",
"doi-asserted-by": "crossref",
"first-page": "38",
"journal-title": "Acta Orthop",
"key": "10.1016/j.clnesp.2024.02.023_bib61",
"volume": "94",
"year": "2023"
},
{
"article-title": "Vitamin D: the \"sunshine\" vitamin",
"author": "Nair",
"first-page": "118",
"issue": "2",
"journal-title": "J Pharmacol Pharmacother",
"key": "10.1016/j.clnesp.2024.02.023_bib62",
"volume": "3",
"year": "2012"
},
{
"DOI": "10.3390/ijms20010145",
"article-title": "Vitamin D and human health",
"author": "Zmijewski",
"doi-asserted-by": "crossref",
"first-page": "145",
"issue": "1",
"journal-title": "Int J Mol Sci",
"key": "10.1016/j.clnesp.2024.02.023_bib63",
"volume": "20",
"year": "2019"
},
{
"key": "10.1016/j.clnesp.2024.02.023_bib64",
"series-title": "National dietary survey in Iceland 2019–2021. Other nutritions",
"year": "2021"
},
{
"article-title": "Association between vitamin D status and risk of covid-19 in-hospital mortality: a systematic review and meta-analysis of observational studies",
"author": "Ebrahimzadeh",
"first-page": "1",
"journal-title": "Crit Rev Food Sci Nutr",
"key": "10.1016/j.clnesp.2024.02.023_bib65",
"year": "2021"
},
{
"DOI": "10.2147/RMHP.S291584",
"article-title": "Effects of vitamin D on COVID-19 infection and prognosis: a systematic review",
"author": "Yisak",
"doi-asserted-by": "crossref",
"first-page": "31",
"journal-title": "Risk Manag Healthc Pol",
"key": "10.1016/j.clnesp.2024.02.023_bib66",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1007/s13668-021-00380-2",
"article-title": "The nutrition-COVID-19 interplay: a review",
"author": "Antwi",
"doi-asserted-by": "crossref",
"first-page": "364",
"issue": "4",
"journal-title": "Curr Nutr Rep",
"key": "10.1016/j.clnesp.2024.02.023_bib67",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(19)32497-3",
"article-title": "Dynamics of the double burden of malnutrition and the changing nutrition reality",
"author": "Popkin",
"doi-asserted-by": "crossref",
"first-page": "65",
"issue": "10217",
"journal-title": "Lancet",
"key": "10.1016/j.clnesp.2024.02.023_bib68",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.3389/fnut.2020.619850",
"article-title": "The burden of malnutrition and fatal COVID-19: a global burden of disease analysis",
"author": "Mertens",
"doi-asserted-by": "crossref",
"journal-title": "Front Nutr",
"key": "10.1016/j.clnesp.2024.02.023_bib69",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1002/jcsm.12383",
"article-title": "GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community",
"author": "Cederholm",
"doi-asserted-by": "crossref",
"first-page": "207",
"issue": "1",
"journal-title": "J Cachexia Sarcopenia Muscle",
"key": "10.1016/j.clnesp.2024.02.023_bib70",
"volume": "10",
"year": "2019"
}
],
"reference-count": 70,
"references-count": 70,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2405457724000469"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "High risk of malnutrition among hospitalised coronavirus disease 2019 (COVID-19) patients is associated with mortality and other clinical outcomes",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "61"
}
