Vitamin D Serum Levels in Subjects Tested for SARS-CoV-2: What Are the Differences among Acute, Healed, and Negative COVID-19 Patients? A Multicenter Real-Practice Study
et al., Nutrients, doi:10.3390/nu13113932, Nov 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
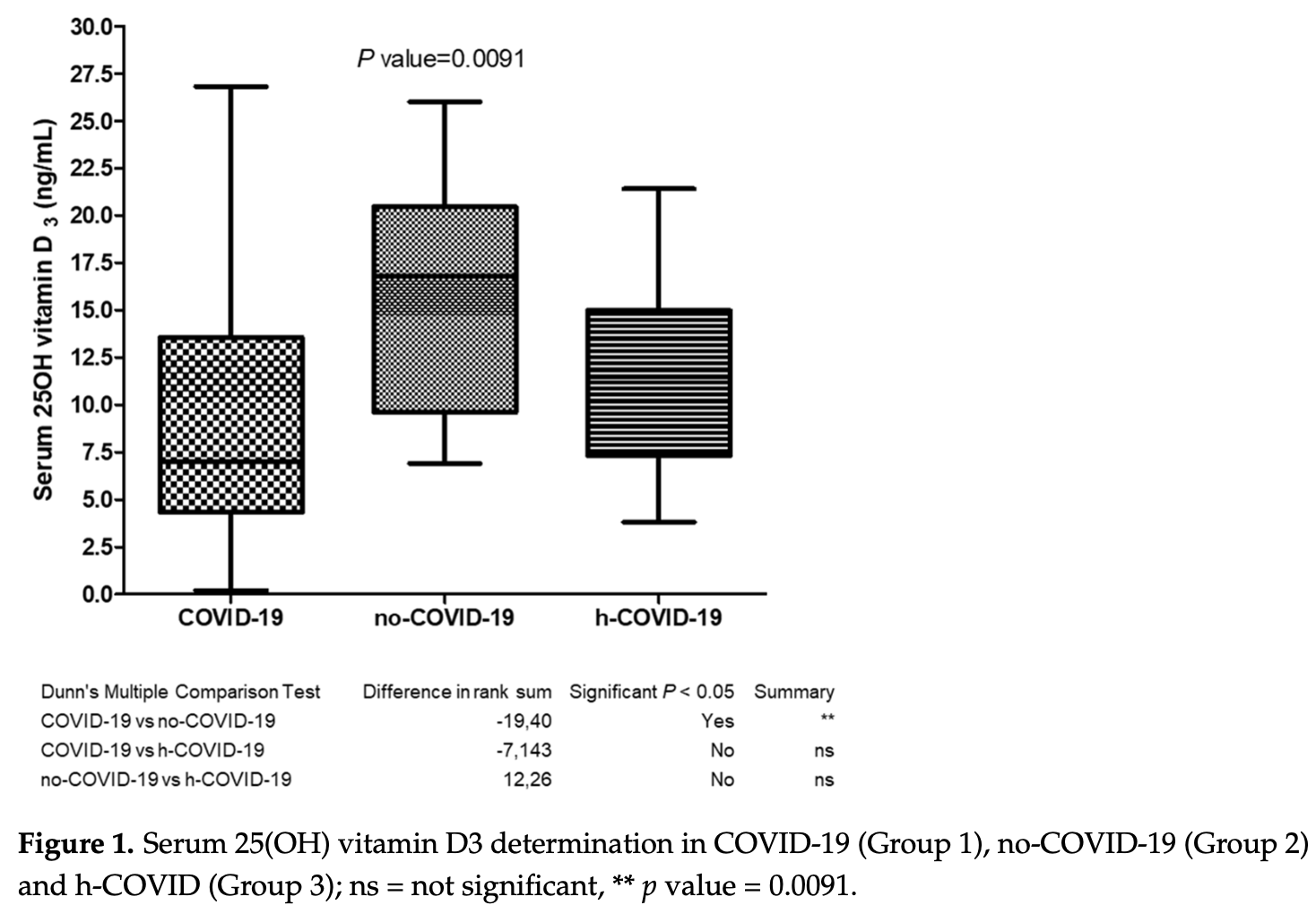
Analysis of 117 patients in Italy, showing COVID-19 patients had significantly lower vitamin D levels than control patients.
Gallelli et al., 3 Nov 2021, prospective, Italy, peer-reviewed, 17 authors.
Vitamin D Serum Levels in Subjects Tested for SARS-CoV-2: What Are the Differences among Acute, Healed, and Negative COVID-19 Patients? A Multicenter Real-Practice Study
Nutrients, doi:10.3390/nu13113932
Vitamin D might play a role in counteracting COVID-19, albeit strong evidence is still lacking in the literature. The present multicenter real-practice study aimed to evaluate the differences of 25(OH)D 3 serum levels in adults tested for SARS-CoV-2 (acute COVID-19 patients, subjects healed from COVID-19, and non-infected ones) recruited over a 6-month period (March-September 2021). In a sample of 117 subjects, a statistically significant difference was found, with acute COVID-19 patients demonstrating the lowest levels of serum 25(OH)D 3 (9.63 ± 8.70 ng/mL), significantly lower than values reported by no-COVID-19 patients (15.96 ± 5.99 ng/mL, p = 0.0091) and healed COVID-19 patients (11.52 ± 4.90 ng/mL, p > 0.05). Male gender across the three groups displayed unfluctuating 25(OH)D 3 levels, hinting at an inability to ensure adequate levels of the active vitamin D3 form (1α,25(OH)2D3). As a secondary endpoint, we assessed the correlation between serum 25(OH)D 3 levels and pro-inflammatory cytokine interleukin-6 (IL-6) in patients with extremely low serum 25(OH)D 3 levels (<1 ng/mL) and in a subset supplemented with 1α,25(OH) 2 D 3 . Although patients with severe hypovitaminosis-D showed no significant increase in IL-6 levels, acute COVID-19 patients manifested high circulating IL-6 at admission (females = 127.64 ± 22.24 pg/mL, males = 139.28 ± 48.95 ng/mL) which dropped drastically after the administration of 1α,25(OH) 2 D 3 (1.84 ± 0.77 pg/mL and 2.65 ± 0.92 ng/mL, respectively). Taken together, these findings suggest that an administration of 1α,25(OH) 2 D 3 might be helpful for treating male patients with an acute COVID-19 infection. Further studies on rapid correction of vitamin D deficiency with fast acting metabolites are warranted in COVID-19 patients.
References
Afzal, Bojesen, Nordestgaard, Low 25-Hydroxyvitamin D and risk of type 2 diabetes: A prospective cohort study and metaanalysis, Clin. Chem, doi:10.1373/clinchem.2012.193003
Bikle, Vitamin D metabolism, mechanism of action, and clinical applications, Chem. Biol, doi:10.1016/j.chembiol.2013.12.016
Bui, Zhu, Hawkins, Cortez-Resendiz, Bellon, Vitamin D regulation of the immune system and its implications for COVID-19: A mini review, SAGE Open Med, doi:10.1177/20503121211014073
Buitrago, Boland, Caveolae and caveolin-1 are implicated in 1alpha,25(OH)2-vitamin D3-dependent modulation of Src, MAPK cascades and VDR localization in skeletal muscle cells, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2010.03.002
Cannell, Vieth, Umhau, Holick, Grant et al., Epidemic influenza and vitamin D, Epidemiol. Infect, doi:10.1017/S0950268806007175
Chamekh, Casimir, Editorial: Sexual dimorphism of the immune inflammatory response in infectious and non-infectious diseases, Front. Immunol, doi:10.3389/fimmu.2019.00107
D'avolio, Avataneo, Manca, Cusato, De Nicolò et al., 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Ferraro, Calafiore, Dambruoso, Guidarini, De Sire, COVID-19 related fatigue: Which role for rehabilitation in post-COVID-19 patients? A case series, J. Med. Virol, doi:10.1002/jmv.26717
Fu, Cheng, Wu, Understanding SARS-CoV-2-mediated inflammatory responses: From mechanisms to potential therapeutic tools, Virol. Sin, doi:10.1007/s12250-020-00207-4
Gallelli, Escin: A review of its anti-edematous, anti-inflammatory, and venotonic properties, Drug Des. Dev. Ther, doi:10.2147/DDDT.S207720
Gallelli, Michniewicz, Cione, Squillace, Colosimo et al., 25-Hydroxy vitamin D detection using different analytic methods in patients with migraine, J. Clin. Med
Gimigliano, Moretti, De Sire, Calafiore, Iolascon, The combination of vitamin D deficiency and overweight affects muscle mass and function in older post-menopausal women, Aging Clin. Exp. Res, doi:10.1007/s40520-018-0921-1
Ginde, Mansbach, Camargo, Association between serum 25-Hydroxyvitamin D level and upper respiratory tract infection in the third national health and nutrition examination survey, Arch. Intern. Med, doi:10.1001/archinternmed.2008.560
Griffin, Hewison, Hopkin, Kenny, Quinton et al., Preventing vitamin D deficiency during the COVID-19 pandemic: UK definitions of vitamin D sufficiency and recommended supplement dose are set too low, Clin. Med, doi:10.7861/clinmed.2020-0858
Griffin, Hewison, Hopkin, Kenny, Quinton et al., Vitamin D and COVID-19: Evidence and recommendations for supplementation, R. Soc. Open Sci, doi:10.1098/rsos.201912
Hewison, Vitamin D and the immune system: New perspectives on an old theme, Rheum. Dis. Clin. N. Am, doi:10.1016/j.rdc.2012.03.012
Holick, High prevalence of vitamin D inadequacy and implications for health, Mayo Clin. Proc. Marzo, doi:10.4065/81.3.353
Iolascon, Mauro, Fiore, Cisari, Benedetti et al., Can vitamin D deficiency influence muscle performance in postmenopausal women? A multicenter retrospective study, Eur. J. Phys. Rehabil. Med, doi:10.23736/S1973-9087.17.04533-6
Iorio, Ammendolia, Marotta, Ricardi, De Sire, A bond between rheumatic diseases and cancer in the elderly: The interleukin-6 pathway, Int. J. Rheum Dis, doi:10.1111/1756-185X.14194
Jin, He, Wu, Liu, Han et al., Gender differences in patients with COVID-19: Focus on severity and mortality, Front. Public Health, doi:10.3389/fpubh.2020.00152
Keller, Varela, Vazquez, Dangol, Damm et al., The role of vitamin D in the development of diabetes post gestational diabetes mellitus: A systematic literature review, Nutrients, doi:10.3390/nu12061733
Koenig, Buskiewicz, Huber, Age-Associated changes in estrogen receptor ratios correlate with increased female susceptibility to Coxsackievirus B3-Induced myocarditis, Front. Immunol, doi:10.3389/fimmu.2017.01585
Labudzynskyi, Shymanskyy, Veliky, Role of vitamin D3 in regulation of interleukin-6 and osteopontin expression in liver of diabetic mice, Eur. Rev. Med. Pharmacol. Sci
Lee, Li, Chan, Hollis, Lee et al., Circulating levels of vitamin D and colon and rectal cancer: The physicians' health study and a meta-analysis of prospective studies, Cancer Prev. Res, doi:10.1158/1940-6207.CAPR-10-0289
Liu, Li, Zhou, Guan, Xiang, Can we use interleukin-6 (IL-6) blockade for coronavirus disease 2019 (COVID-19)-induced cytokine release syndrome (CRS)?, J. Autoimmun, doi:10.1016/j.jaut.2020.102452
Liu, Zhou, Yang, The cytokine storm of severe influenza and development of immunomodulatory therapy, Cell Mol. Immunol, doi:10.1038/cmi.2015.74
Lu, Zhang, Ma, Yue, Zou et al., Link between community-acquired pneumonia and vitamin D levels in older patients, J. Gerontol. Geriatr, doi:10.1007/s00391-017-1237-z
Ma, Zhou, Heianza, Qi, Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: A prospective study in UK Biobank, Am. J. Clin. Nutr, doi:10.1093/ajcn/nqaa381
Manion, Hullsiek, Wilson, Rhame, Kojic et al., Vitamin D deficiency is associated with IL-6 levels and monocyte activation in HIV-infected persons, PLoS ONE
Martín Giménez, Inserra, Tajer, Mariani, Ferder et al., Lungs as target of COVID-19 infection: Protective common molecular mechanisms of vitamin D and melatonin as a new potential synergistic treatment, Life Sci, doi:10.1016/j.lfs.2020.117808
Mauvais-Jarvis, Klein, Levin, Estradiol, progesterone, immunomodulation, and COVID-19 outcomes, Endocrinology, doi:10.1210/endocr/bqaa127
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., HLH across speciality collaboration, UK. COVID-19: Consider cytokine storm syndromes and immunosuppression, Lancet, doi:10.1016/S0140-6736(20)30628-0
Negrini, De Sire, Andrenelli, Lazzarini, Patrini et al., International multiprofessional steering committee of cochrane rehabilitation REH-COVER action. rehabilitation and COVID-19: The cochrane rehabilitation 2020 rapid living systematic review. update as of July 31st, Eur. J. Phys. Rehabil. Med, doi:10.23736/S1973-9087.20.06539-9
Osorio Landa, Pérez Díaz, Laguna Bárcenas, López Navarro, Abella Roa et al., Association of serum vitamin D levels with chronic disease and mortality, Nutr. Hosp
Perri, Pingitore, Cione, Vilardi, Perrone et al., Proliferative and anti-proliferative effects of retinoic acid at doses similar to endogenous levels in Leydig MLTC-1/R2C/TM-3 cells, Biochim. Biophys. Acta, doi:10.1016/j.bbagen.2010.06.006
Quesada-Gomez, Entrenas-Castillo, Bouillon, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105719
Sanders, Monogue, Jodlowski, Cutrell, Pharmacologic treatments for Coronavirus disease 2019 (COVID-19): A Review, JAMA, doi:10.1001/jama.2020.6019
Siniscalchi, Lochner, Anticoli, Chirchiglia, De Sarro et al., What is the current role for vitamin D and the risk of stroke?, Curr. Neurovasc. Res, doi:10.2174/1567202616666190412152948
Torkildsen, Knappskog, Nyland, Myhr, Vitamin D-dependent rickets as a possible risk factor for multiple sclerosis, Arch. Neurol, doi:10.1001/archneur.65.6.809
Umar, Sastry, Chouchane, Role of Vitamin D beyond the skeletal function: A Review of the molecular and clinical studies, Int. J. Mol. Sci, doi:10.3390/ijms19061618
White, Vitamin, Signaling, Infectious Diseases, and Regulation of Innate Immunity, Infect. Immun
Yan, Zhang, Cheng, Wang, Qin, Gender differences in vitamin D status in China, Med. Sci. Monit. Int. Med. J. Exp. Clin. Res, doi:10.12659/MSM.916326
DOI record:
{
"DOI": "10.3390/nu13113932",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu13113932",
"abstract": "<jats:p>Vitamin D might play a role in counteracting COVID-19, albeit strong evidence is still lacking in the literature. The present multicenter real-practice study aimed to evaluate the differences of 25(OH)D3 serum levels in adults tested for SARS-CoV-2 (acute COVID-19 patients, subjects healed from COVID-19, and non-infected ones) recruited over a 6-month period (March–September 2021). In a sample of 117 subjects, a statistically significant difference was found, with acute COVID-19 patients demonstrating the lowest levels of serum 25(OH)D3 (9.63 ± 8.70 ng/mL), significantly lower than values reported by no-COVID-19 patients (15.96 ± 5.99 ng/mL, p = 0.0091) and healed COVID-19 patients (11.52 ± 4.90 ng/mL, p > 0.05). Male gender across the three groups displayed unfluctuating 25(OH)D3 levels, hinting at an inability to ensure adequate levels of the active vitamin D3 form (1α,25(OH)2D3). As a secondary endpoint, we assessed the correlation between serum 25(OH)D3 levels and pro-inflammatory cytokine interleukin-6 (IL-6) in patients with extremely low serum 25(OH)D3 levels (<1 ng/mL) and in a subset supplemented with 1α,25(OH)2D3. Although patients with severe hypovitaminosis-D showed no significant increase in IL-6 levels, acute COVID-19 patients manifested high circulating IL-6 at admission (females = 127.64 ± 22.24 pg/mL, males = 139.28 ± 48.95 ng/mL) which dropped drastically after the administration of 1α,25(OH)2D3 (1.84 ± 0.77 pg/mL and 2.65 ± 0.92 ng/mL, respectively). Taken together, these findings suggest that an administration of 1α,25(OH)2D3 might be helpful for treating male patients with an acute COVID-19 infection. Further studies on rapid correction of vitamin D deficiency with fast acting metabolites are warranted in COVID-19 patients.</jats:p>",
"alternative-id": [
"nu13113932"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0858-7902",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gallelli",
"given": "Luca",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-6341-4572",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mannino",
"given": "Gaia Chiara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Luciani",
"given": "Filippo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5541-8346",
"affiliation": [],
"authenticated-orcid": false,
"family": "de Sire",
"given": "Alessandro",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0562-9196",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mancuso",
"given": "Elettra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gangemi",
"given": "Pietro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cosco",
"given": "Lucio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0647-5846",
"affiliation": [],
"authenticated-orcid": false,
"family": "Monea",
"given": "Giuseppe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Averta",
"given": "Carolina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Minchella",
"given": "Pasquale",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Colosimo",
"given": "Manuela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Muraca",
"given": "Lucia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Longhini",
"given": "Federico",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2828-2455",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ammendolia",
"given": "Antonio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9375-1513",
"affiliation": [],
"authenticated-orcid": false,
"family": "Andreozzi",
"given": "Francesco",
"sequence": "additional"
},
{
"affiliation": [],
"family": "De Sarro",
"given": "Giovambattista",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0562-0597",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cione",
"given": "Erika",
"sequence": "additional"
},
{
"affiliation": [],
"name": "G&P Working Group",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
11,
4
]
],
"date-time": "2021-11-04T01:57:49Z",
"timestamp": 1635991069000
},
"deposited": {
"date-parts": [
[
2021,
11,
4
]
],
"date-time": "2021-11-04T02:20:14Z",
"timestamp": 1635992414000
},
"indexed": {
"date-parts": [
[
2024,
5,
9
]
],
"date-time": "2024-05-09T19:53:37Z",
"timestamp": 1715284417504
},
"is-referenced-by-count": 22,
"issue": "11",
"issued": {
"date-parts": [
[
2021,
11,
3
]
]
},
"journal-issue": {
"issue": "11",
"published-online": {
"date-parts": [
[
2021,
11
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
11,
3
]
],
"date-time": "2021-11-03T00:00:00Z",
"timestamp": 1635897600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/13/11/3932/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3932",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
11,
3
]
]
},
"published-online": {
"date-parts": [
[
2021,
11,
3
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.lfs.2020.117808",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.2147/DDDT.S207720",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1001/jama.2020.6019",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1016/j.jsbmb.2020.105719",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1007/s12250-020-00207-4",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/j.chembiol.2013.12.016",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/j.bbagen.2010.06.006",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1016/j.jsbmb.2010.03.002",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.23736/S1973-9087.17.04533-6",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.3390/ijms19061618",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1007/s40520-018-0921-1",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1093/ajcn/nqaa381",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1016/j.rdc.2012.03.012",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1177/20503121211014073",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1016/j.jaut.2020.102452",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1111/1756-185X.14194",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1128/IAI.00353-08",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.4065/81.3.353",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1017/S0950268806007175",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1001/archinternmed.2008.560",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1007/s00391-017-1237-z",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.3390/nu12051359",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.3390/jcm8060895",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1001/archneur.65.6.809",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1373/clinchem.2012.193003",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1158/1940-6207.CAPR-10-0289",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.3390/nu12061733",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"article-title": "Association of serum vitamin D levels with chronic disease and mortality",
"author": "Osorio Landa",
"first-page": "335",
"journal-title": "Nutr. Hosp.",
"key": "ref28",
"volume": "37",
"year": "2020"
},
{
"DOI": "10.2174/1567202616666190412152948",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.3389/fimmu.2019.00107",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.3389/fpubh.2020.00152",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.3389/fimmu.2017.01585",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1210/endocr/bqaa127",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.12659/MSM.916326",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1371/journal.pone.0175517",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1038/cmi.2015.74",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"article-title": "Role of vitamin D3 in regulation of interleukin-6 and osteopontin expression in liver of diabetic mice",
"author": "Labudzynskyi",
"first-page": "2916",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "ref37",
"volume": "20",
"year": "2016"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.23736/S1973-9087.20.06539-9",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1002/jmv.26717",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1098/rsos.201912",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.7861/clinmed.2020-0858",
"doi-asserted-by": "publisher",
"key": "ref42"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/13/11/3932"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Vitamin D Serum Levels in Subjects Tested for SARS-CoV-2: What Are the Differences among Acute, Healed, and Negative COVID-19 Patients? A Multicenter Real-Practice Study",
"type": "journal-article",
"volume": "13"
}
