Hourly Analysis of Mechanical Ventilation Parameters in Critically Ill Adult Covid-19 Patients: Association with Mortality
et al., Journal of Intensive Care Medicine, doi:10.1177/08850666221105423, May 2022
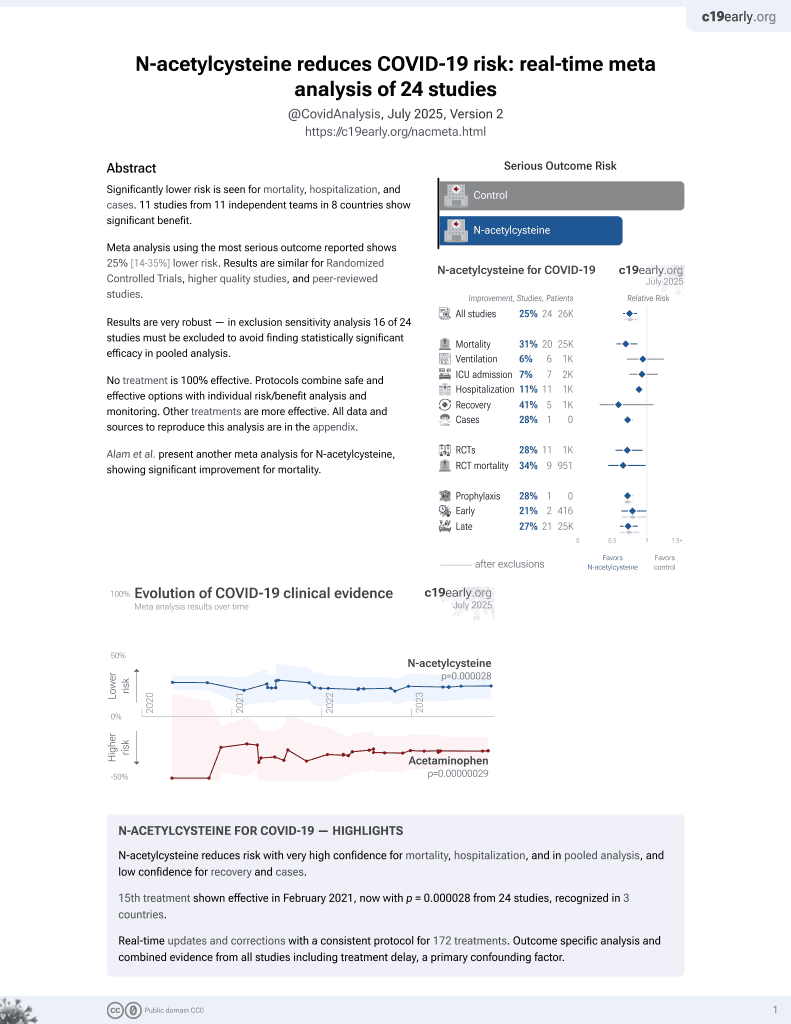
16th treatment shown to reduce risk in
February 2021, now with p = 0.0000032 from 25 studies, recognized in 3 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 140 mechanically ventilated patients in Spain, showing lower mortality with acetylcysteine treatment in unadjusted results, not reaching statistical significance.
Although the 39% lower mortality is not statistically significant, it is consistent with the significant 31% lower mortality [14‑44%] from meta-analysis of the 20 mortality results to date.
|
risk of death, 39.0% lower, RR 0.61, p = 0.08, treatment 10 of 38 (26.3%), control 44 of 102 (43.1%), NNT 5.9.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Fariña-González et al., 31 May 2022, retrospective, Spain, peer-reviewed, 8 authors, study period 5 March, 2020 - 30 April, 2020.
Hourly Analysis of Mechanical Ventilation Parameters in Critically Ill Adult Covid-19 Patients: Association with Mortality
Journal of Intensive Care Medicine, doi:10.1177/08850666221105423
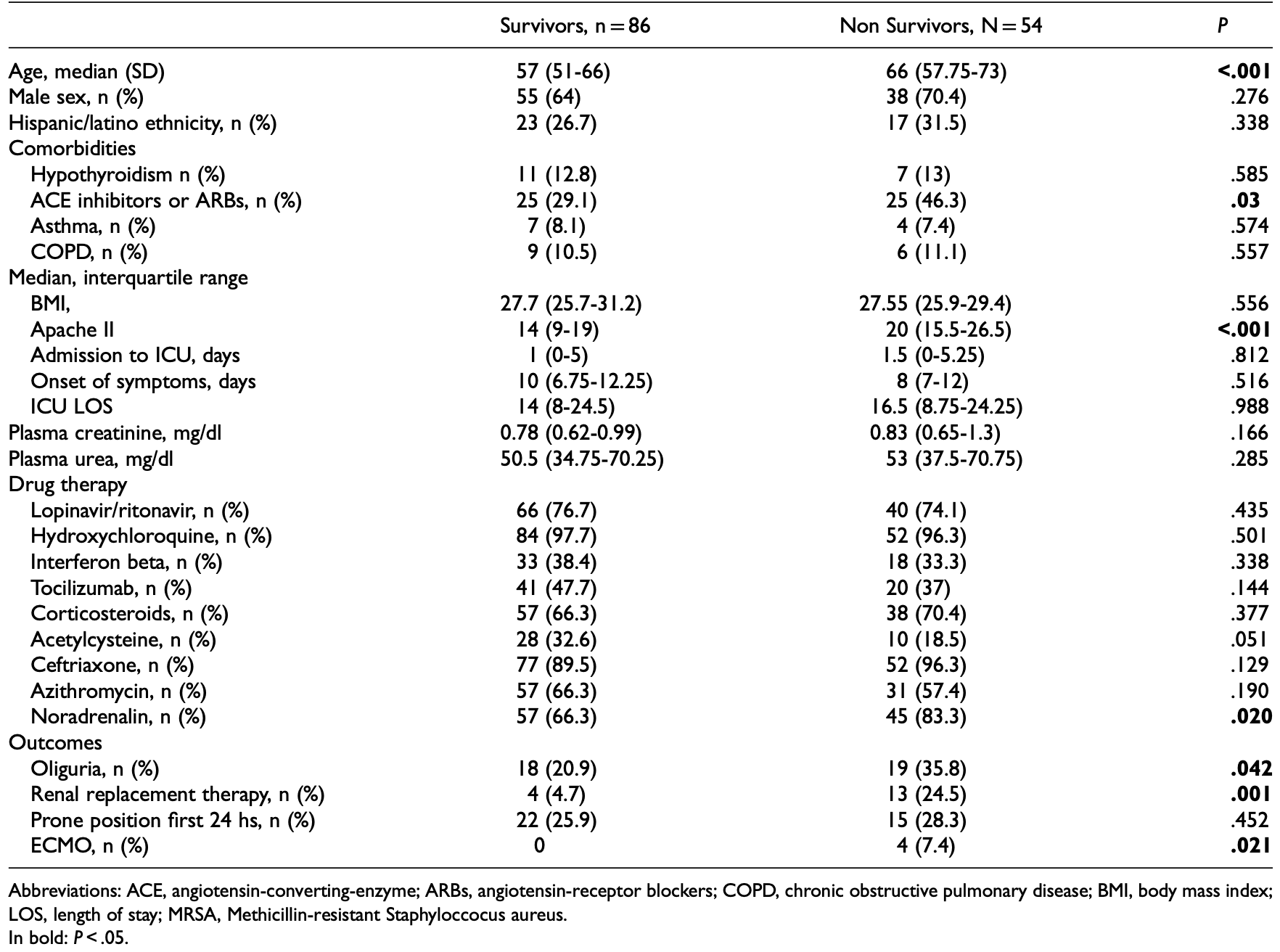
Objective: There exists controversy about the pathophysiology and lung mechanics of COVID-19 associated acute respiratory distress syndrome (ARDS), because some report severe hypoxemia with preserved respiratory system mechanics, contrasting with "classic" ARDS. We performed a detailed hourly analysis of the characteristics and time course of lung mechanics and biochemical analysis of patients requiring invasive mechanical ventilation (IMV) for COVID-19-associated ARDS, comparing survivors and nonsurvivors. Methods: Retrospective analysis of the data stored in the ICU information system of patients admitted in our hospital ICU that required IMV due to confirmed SARS-CoV-2 pneumonia between March 5th and April 30th, 2020. We compare respiratory system mechanics and gas exchange during the first ten days of IMV, discriminating volume and pressure controlled modes, between ICU survivors and non-survivors. Results: 140 patients were included, analyzing 11 138 respiratory mechanics recordings. Global mortality was 38.6%. Multivariate analysis showed that age (OR 1.092, 95% (CI 1.014-1.176)) and need of renal replacement therapies (OR 10.15, (95% CI 1.58-65.11)) were associated with higher mortality. Previous use of Angiotensin Converting Enzyme inhibitor (ACEI)/angiotensin-receptor blockers (ARBs) also seemed to show an increased mortality (OR 4.612, (95% CI 1.19-17.84)) although this significance was lost when stratifying by age. Respiratory variables start to diverge significantly between survivors and non-survivors after the 96 to 120 hours (hs) from mechanical ventilation initiation, particularly respiratory system compliance. In non survivors, mechanical power at 24 and 96 hs was higher regardless ventilatory mode. Conclusions: In patients admitted for SARS-CoV-2 pneumonia and requiring mechanical ventilation, non survivors have different respiratory system mechanics than survivors in the first 10 days of ICU admission. We propose a checkpoint at 96-120 hs to assess patients improvement or worsening in order to consider escalating to extracorporeal therapies.
Author Contributions TFG, ANR and MSG designed the study. TFF, ANR and JL extracted and analyzed the data. TFF, JL, MCR, VYZ and SDM drafted the article. MSG revised the article and supervised the project. All authors revised the manuscript.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval CEIC 21/170-E.
Supplemental Material Supplemental material for this article is available online.
ORCID iD Tomás F. Fariña-González https://orcid.org/0000-0002-4892-8153
References
Alhazzani, Moller, Arabi, Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19), Crit Care Med, doi:10.1097/CCM.0000000000004363
Auld, Caridi-Scheible, Blum, ICU and ventilator mortality among critically ill adults with coronavirus disease 2019, Crit Care Med, doi:10.1097/CCM.0000000000004457
Barbaro, Maclaren, Boonstra, Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the Extracorporeal Life Support Organization registry, Lancet, doi:10.1016/S0140-6736(20)32008-0
Becher, Van Der Staay, Schadler, Frerichs, Weiler, Calculation of mechanical power for pressure-controlled ventilation, Intensive Care Med, doi:10.1007/s00134-019-05636-8
Bellani, Laffey, Pham, Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries, JAMA, doi:10.1001/jama.2016.0291
Chiumello, Gotti, Guanziroli, Bedside calculation of mechanical power during volume-and pressure-controlled mechanical ventilation, Crit Care, doi:10.1186/s13054-020-03116-w
Cressoni, Chiurazzi, Gotti, Lung inhomogeneities and time course of ventilator-induced mechanical injuries, Anesthesiology, doi:10.1097/ALN.0000000000000727
Drent, Cobben, Henderson, Wouters, Van Dieijen-Visser, Usefulness of lactate dehydrogenase and its isoenzymes as indicators of lung damage or inflammation, Eur Respir J, doi:10.1183/09031936.96.09081736
Gattinoni, Chiumello, Caironi, COVID-19 pneumonia: different respiratory treatments for different phenotypes?, Intensive Care Med, doi:10.1007/s00134-020-06033-2
Gattinoni, Coppola, Cressoni, Busana, Rossi et al., COVID-19 does not lead to a "typical" acute respiratory distress syndrome, Am J Respir Crit Care Med, doi:10.1164/rccm.202003-0817LE
Gattinoni, Tonetti, Cressoni, Ventilator-related causes of lung injury: the mechanical power, Intensive Care Med, doi:10.1007/s00134-016-4505-2
Grasselli, Pesenti, Cecconi, Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response, JAMA, doi:10.1001/jama.2020.4031
Hagadorn, Bloor, Yang, Elevated plasma activity of lactate dehydrogenase isoenzyme-3 (LDH 3) in experimentally induced immunologic lung injury, Am J Pathol
Hirsch, Ng, Ross, Acute kidney injury in patients hospitalized with COVID-19, Kidney Int, doi:10.1016/j.kint.2020.05.006
Kon, Smith, Chang, Extracorporeal membrane oxygenation support in severe COVID-19, Ann Thorac Surg, doi:10.1016/j.athoracsur.2020.07.002
Mancia, Rea, Ludergnani, Apolone, Corrao, Renin-angiotensin-aldosterone system blockers and the risk of COVID-19, N Engl J Med, doi:10.1056/NEJMoa2006923
Mustafa, Alexander, Joshi, Extracorporeal membrane oxygenation for patients with COVID-19 in severe respiratory failure, JAMA Surg, doi:10.1001/jamasurg.2020.3950
Shekar, Badulak, Peek, Extracorporeal life support organization coronavirus disease 2019 interim guidelines: a consensus document from an international group of interdisciplinary extracorporeal membrane oxygenation providers, ASAIO J, doi:10.1097/MAT.0000000000001193
Sinha, Fauvel, Singh, Soni, Ventilatory ratio: a simple bedside measure of ventilation, Br J Anaesth, doi:10.1093/bja/aep054
Su, Yang, Wan, Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China, Kidney Int, doi:10.1016/j.kint.2020.04.003
Wang, Hu, Hu, Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585
White, Anderson, Outcomes in patients with COVID-19 infection taking ACEI/ARB, Curr Cardiol Rep, doi:10.1007/s11886-020-01291-4
Wu, Chen, Cai, Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China, JAMA Intern Med, doi:10.1001/jamainternmed.2020.0994
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
Zhu, Zhang, Wang, A novel coronavirus from patients with pneumonia in China, 2019, N Engl J Med, doi:10.1056/NEJMoa2001017
DOI record:
{
"DOI": "10.1177/08850666221105423",
"ISSN": [
"0885-0666",
"1525-1489"
],
"URL": "http://dx.doi.org/10.1177/08850666221105423",
"abstract": "<jats:p> Objective: There exists controversy about the pathophysiology and lung mechanics of COVID-19 associated acute respiratory distress syndrome (ARDS), because some report severe hypoxemia with preserved respiratory system mechanics, contrasting with “classic” ARDS. We performed a detailed hourly analysis of the characteristics and time course of lung mechanics and biochemical analysis of patients requiring invasive mechanical ventilation (IMV) for COVID-19-associated ARDS, comparing survivors and non-survivors. Methods: Retrospective analysis of the data stored in the ICU information system of patients admitted in our hospital ICU that required IMV due to confirmed SARS-CoV-2 pneumonia between March 5th and April 30th, 2020. We compare respiratory system mechanics and gas exchange during the first ten days of IMV, discriminating volume and pressure controlled modes, between ICU survivors and non-survivors. Results: 140 patients were included, analyzing 11 138 respiratory mechanics recordings. Global mortality was 38.6%. Multivariate analysis showed that age (OR 1.092, 95% (CI 1.014-1.176)) and need of renal replacement therapies (OR 10.15, (95% CI 1.58-65.11)) were associated with higher mortality. Previous use of Angiotensin Converting Enzyme inhibitor (ACEI)/angiotensin-receptor blockers (ARBs) also seemed to show an increased mortality (OR 4.612, (95% CI 1.19-17.84)) although this significance was lost when stratifying by age. Respiratory variables start to diverge significantly between survivors and non-survivors after the 96 to 120 hours (hs) from mechanical ventilation initiation, particularly respiratory system compliance. In non survivors, mechanical power at 24 and 96 hs was higher regardless ventilatory mode. Conclusions: In patients admitted for SARS-CoV-2 pneumonia and requiring mechanical ventilation, non survivors have different respiratory system mechanics than survivors in the first 10 days of ICU admission. We propose a checkpoint at 96–120 hs to assess patients improvement or worsening in order to consider escalating to extracorporeal therapies. </jats:p>",
"alternative-id": [
"10.1177/08850666221105423"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4892-8153",
"affiliation": [
{
"name": "Critical Care Deparment, Hospital Universitario Clínico San Carlos, Madrid, Spain"
}
],
"authenticated-orcid": false,
"family": "Fariña-González",
"given": "Tomás F.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Critical Care Deparment, Hospital Universitario Clínico San Carlos, Madrid, Spain"
}
],
"family": "Núñez-Reiz",
"given": "Antonio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Critical Care Deparment, Hospital Universitario Clínico San Carlos, Madrid, Spain"
}
],
"family": "Yordanov-Zlatkov",
"given": "Viktor",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Anesthesiology Department, Hospital Universitario La Paz, Madrid, Spain"
}
],
"family": "Latorre",
"given": "Julieta",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Critical Care Deparment, Hospital Universitario Clínico San Carlos, Madrid, Spain"
}
],
"family": "Calle-Romero",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Critical Care Deparment, Hospital Universitario Clínico San Carlos, Madrid, Spain"
}
],
"family": "Alonso-Martinez",
"given": "Patricia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Critical Care Deparment, Hospital Universitario Clínico San Carlos, Madrid, Spain"
}
],
"family": "Domingo-Marín",
"given": "Sara",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Critical Care Deparment, Hospital Universitario Clínico San Carlos, Madrid, Spain"
}
],
"family": "Sánchez-García",
"given": "Miguel",
"sequence": "additional"
}
],
"container-title": "Journal of Intensive Care Medicine",
"container-title-short": "J Intensive Care Med",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"journals.sagepub.com"
]
},
"created": {
"date-parts": [
[
2022,
6,
1
]
],
"date-time": "2022-06-01T05:56:40Z",
"timestamp": 1654063000000
},
"deposited": {
"date-parts": [
[
2022,
6,
1
]
],
"date-time": "2022-06-01T05:56:43Z",
"timestamp": 1654063003000
},
"indexed": {
"date-parts": [
[
2022,
6,
1
]
],
"date-time": "2022-06-01T06:15:02Z",
"timestamp": 1654064102832
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
5,
31
]
]
},
"language": "en",
"license": [
{
"URL": "http://journals.sagepub.com/page/policies/text-and-data-mining-license",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
31
]
],
"date-time": "2022-05-31T00:00:00Z",
"timestamp": 1653955200000
}
}
],
"link": [
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/08850666221105423",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/full-xml/10.1177/08850666221105423",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/08850666221105423",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "179",
"original-title": [],
"page": "088506662211054",
"prefix": "10.1177",
"published": {
"date-parts": [
[
2022,
5,
31
]
]
},
"published-online": {
"date-parts": [
[
2022,
5,
31
]
]
},
"publisher": "SAGE Publications",
"reference": [
{
"DOI": "10.1056/NEJMoa2001017",
"doi-asserted-by": "publisher",
"key": "bibr1-08850666221105423"
},
{
"DOI": "10.1001/jama.2020.1585",
"doi-asserted-by": "publisher",
"key": "bibr2-08850666221105423"
},
{
"DOI": "10.1001/jama.2020.4031",
"doi-asserted-by": "publisher",
"key": "bibr3-08850666221105423"
},
{
"DOI": "10.1164/rccm.202003-0817LE",
"doi-asserted-by": "publisher",
"key": "bibr4-08850666221105423"
},
{
"DOI": "10.1007/s00134-020-06033-2",
"doi-asserted-by": "publisher",
"key": "bibr5-08850666221105423"
},
{
"DOI": "10.1186/s13054-020-03116-w",
"doi-asserted-by": "publisher",
"key": "bibr6-08850666221105423"
},
{
"DOI": "10.1007/s00134-016-4505-2",
"doi-asserted-by": "publisher",
"key": "bibr7-08850666221105423"
},
{
"DOI": "10.1007/s00134-019-05636-8",
"doi-asserted-by": "publisher",
"key": "bibr8-08850666221105423"
},
{
"DOI": "10.1093/bja/aep054",
"doi-asserted-by": "publisher",
"key": "bibr9-08850666221105423"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"doi-asserted-by": "publisher",
"key": "bibr10-08850666221105423"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "bibr11-08850666221105423"
},
{
"DOI": "10.1097/CCM.0000000000004457",
"doi-asserted-by": "publisher",
"key": "bibr12-08850666221105423"
},
{
"DOI": "10.1001/jama.2016.0291",
"doi-asserted-by": "publisher",
"key": "bibr13-08850666221105423"
},
{
"DOI": "10.1056/NEJMoa2006923",
"doi-asserted-by": "publisher",
"key": "bibr14-08850666221105423"
},
{
"DOI": "10.1007/s11886-020-01291-4",
"doi-asserted-by": "publisher",
"key": "bibr15-08850666221105423"
},
{
"DOI": "10.1016/j.kint.2020.04.003",
"doi-asserted-by": "publisher",
"key": "bibr16-08850666221105423"
},
{
"DOI": "10.1016/j.kint.2020.05.006",
"doi-asserted-by": "publisher",
"key": "bibr17-08850666221105423"
},
{
"author": "Hagadorn JE",
"first-page": "575",
"issue": "3",
"journal-title": "Am J Pathol",
"key": "bibr18-08850666221105423",
"volume": "64",
"year": "1971"
},
{
"DOI": "10.1183/09031936.96.09081736",
"doi-asserted-by": "publisher",
"key": "bibr19-08850666221105423"
},
{
"DOI": "10.1097/CCM.0000000000004363",
"doi-asserted-by": "publisher",
"key": "bibr20-08850666221105423"
},
{
"DOI": "10.1097/ALN.0000000000000727",
"doi-asserted-by": "publisher",
"key": "bibr21-08850666221105423"
},
{
"DOI": "10.1097/MAT.0000000000001193",
"doi-asserted-by": "publisher",
"key": "bibr22-08850666221105423"
},
{
"DOI": "10.1016/S0140-6736(20)32008-0",
"doi-asserted-by": "publisher",
"key": "bibr23-08850666221105423"
},
{
"DOI": "10.1001/jamasurg.2020.3950",
"doi-asserted-by": "publisher",
"key": "bibr24-08850666221105423"
},
{
"DOI": "10.1016/j.athoracsur.2020.07.002",
"doi-asserted-by": "publisher",
"key": "bibr25-08850666221105423"
}
],
"reference-count": 25,
"references-count": 25,
"relation": {},
"resource": {
"primary": {
"URL": "http://journals.sagepub.com/doi/10.1177/08850666221105423"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Critical Care and Intensive Care Medicine"
],
"subtitle": [],
"title": "Hourly Analysis of Mechanical Ventilation Parameters in Critically Ill Adult Covid-19 Patients: Association with Mortality",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1177/sage-journals-update-policy"
}