Folate, B12 and Iron Levels in COVID 19 Patients Observational Case-Control Study
et al., Sağlık Akademisi Kastamonu, doi:10.25279/sak.1102076, Apr 2022
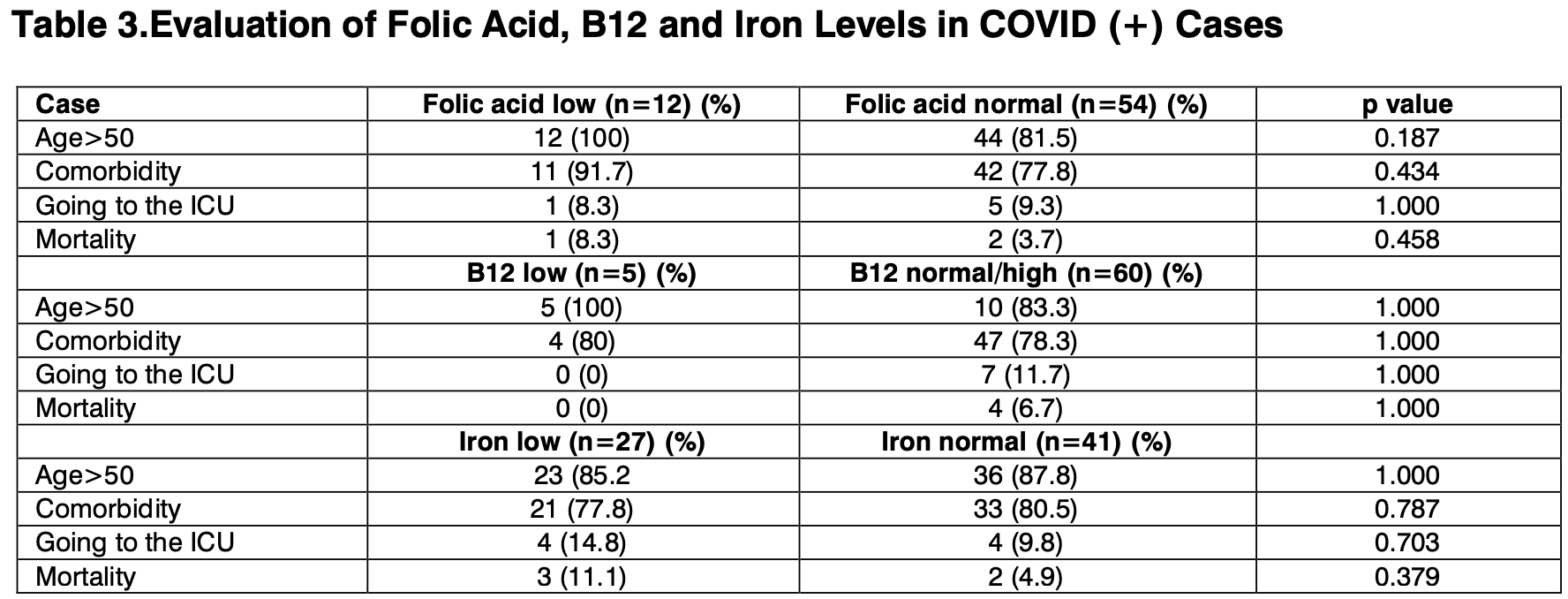
Retrospective 70 COVID-19 cases and 70 non-COVID-19 controls in Turkey, showing no significant differences based on folic acid levels.
|
risk of death, 55.6% lower, RR 0.44, p = 0.46, high vitamin B9 levels (≥4.6μg/L) 2 of 54 (3.7%), low vitamin B9 levels (<4.6μg/L) 1 of 12 (8.3%), NNT 22.
|
|
risk of ICU admission, 11.1% higher, RR 1.11, p = 1.00, high vitamin B9 levels (≥4.6μg/L) 5 of 54 (9.3%), low vitamin B9 levels (<4.6μg/L) 1 of 12 (8.3%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Doğan et al., 21 Apr 2022, retrospective, Turkey, peer-reviewed, 4 authors, study period 7 January, 2022 - 30 March, 2022.
Contact: uzdrahmetdogan@gmail.com, ismail.anac3@saglik.gov.tr, dryakupgezer@gmail.com, drburccu@gmail.com.
Folate, B12 and Iron Levels in COVID 19 Patients Observational Case-Control Study
Sağlık Akademisi Kastamonu, doi:10.25279/sak.1102076
Introduction: Folic acid, B12 and Iron play an important role in the pathogenesis of viral infections. Aim: The aim of the study is to determine the blood levels of Folate, B12 and Iron and to examine their relationship with prognosis in cases followed up by the COVID-19 pandemic service. Materials and Methods: The study was planned as a retrospective observational case-control study. In a period of approximately 3 months, 140 patients were screened retrospectively, 70 of whom were COVID-19 and 70 control cases. Cases <18 years of age, followed up in the Intensive Care Unit or withdrawn from the Intensive Care Unit to the service, and patients taking drugs or supportive treatment that could affect blood Folate, B12, Iron levels were excluded from the study. p<0.05 was accepted as statistical significance level. Results: 48.6% (68) of the cases were male, 51.4% (72) were female. The mean age (Mean±SD) of all cases was 67.3±15.8. No significant difference was observed between the case and control groups in terms of age, gender, presence of comorbid disease, prognosis, Folate and B12 levels. However, the iron level was significantly higher in the case group. Conclusion: As a result, Folic acid and B12 supplementation is needed in the majority of COVID-19 cases. Before supplementing with iron, the iron level should be checked.
Declarations: This article was not produced from the thesis study. It was sent to the 10th Turkey EKMUD Scientific Congress to be held on 25-29 May 2022 as a verbal presentation. No kind of support has been received from anyinstitution / organization / person. The authors declared that there is no conflict of interest. Necessary permissions were obtained from Ordu University and Medical Research Ethics Committee to conduct the study (Decision no: 2022/116). All directives of the Helsinki Declaration have been followed.We would like to thank all Fatsa State Hospital Biochemistry laboratory and service staff who contributed to the study. Author contributions: İdea: AD, İA. Design: AD, İA, YG, BT. İnspection: AD, İA, YG, BT. Resources: AD, İA, YG, BT. Materials: AD, İA. Data collection and/or processing: AD, İA, YG. Analysis and/or interpretation: AD, İA, YG, BT. Literature research: AD, İA. Writing: AD, YG. Critical review: AD, İA, YG, BT
References
Acosta-Elias, Espinosa-Tanguma, The folate concentration and/or folic acid metabolites in plasma as factor for COVID-19 infection, Front Pharmacol, doi:10.3389/fphar.2020.01062
Andreini, Putignano, Rosato, Banci, The human ironproteome, Metallomics
Atıf, Doğan, Anaç, Gezer, Timur, Folate, B12 and Iron Levels in COVID-19 Patients: Observational Case-Control Study, Health Academy Kastamonu (HAK)
Atıf, Doğan, Anaç, Gezer, Timur, Folate, B12 and Iron Levels in COVID-19 Patients: Observational Case-Control Study, Health Academy Kastamonu (HAK)
Atıf, Doğan, Anaç, Gezer, Timur, Folate, B12 and Iron Levels in COVID-19 Patients: Observational Case-Control Study, Health Academy Kastamonu (HAK)
Batista, Cintra, Lucena, Manhães-De-Castro, Toscano et al., The role of vitamin B12 in viral infections: a comprehensive review of its relationship with the muscle-gut-brain axis and implications for SARS-CoV-2 infection, Nutr Rev, doi:10.1093/nutrit/nuab092
Bhaskaram, Micronutrient malnutrition, infection, and immunity: an overview, Nutr Rev, doi:10.1301/00296640260130722
Calder, Carr, Gombart, Eggersdorfer, Optimal nutritional status for a well-functioning ımmune system ıs an ımportant factor to protect against viral ınfections, Nutrients, doi:10.3390/nu12041181
Calder, Nutrition, immunity and COVID-19, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000085
Drakesmith, Prentice, Viral infection and iron metabolism, Nat Rev Microbiol, doi:10.1038/nrmicro1930
Ducker, Rabinowitz, One-carbon metabolism in health and disease, Cell Metab, doi:10.1016/j.cmet.2016.08.009
Elmadfa, Meyer, The role of the status of selected micronutrients in shaping the ımmune function, Endocr Metab Immune Disord Drug Targets, doi:10.2174/1871530319666190529101816
Gombart, Pierre, Maggini, Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients, doi:10.3390/nu12010236
Gropper, Smith, Advanced Nutrition and Human Metabolism
Hiraoka, Kagawa, Genetic polymorphisms and folate status, Congenit Anom, doi:10.1111/cga.12232
Itelman, Wasserstrum, Segev, Avaky, Negru et al., Clinical Characterization of 162 COVID-19 patients in Israel: Preliminary Report from a Large Tertiary Center, Isr Med Assoc J
Jacobson, Wreghitt, Saich, Nagington, Serum folate in viral and mycoplasmal infections, J Infect, doi:10.1016/s0163-4453
Keusch, The history of nutrition: malnutrition, infection and immunity, J Nutr, doi:10.1093/jn/133.1.336S
Meisel, Efros, Bleier, Beit Halevi, Segal et al., Folate levels in patients hospitalized with coronavirus disease, Nutrients, doi:10.3390/nu13030812
Muscogiuri, Barrea, Savastano, Colao, Nutritional recommendations for CoVID-19 quarantine, Eur J Clin Nutr, doi:10.1038/s41430-020
Renzo, Gualtieri, Pivari, Soldati, Attina et al., Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey, J Transl Med, doi:10.1186/s12967-020-02399-5
Rodriguez, Corwin, Gettinger, Corwin, Gubler et al., Nutritional deficiencies and blunted erythropoietin response as causes of the anemia of critical illness, J Crit Care, doi:10.1053/jcrc.2001.21795
Scaglione, Panzavolta, Folate, folic acid and 5-methyltetrahydrofolate are not the same thing, Xenobiotica, doi:10.3109/00498254.2013.845705
Strand, Taneja, Bhandari, Refsum, Ueland et al., Folate, but not vitamin B-12 status, predicts respiratory morbidity in north Indian children, Am J Clin Nutr, doi:10.1093/ajcn/86.1.139
Ward, Crichton, Taylor, Della Corte, Srai et al., Iron and the immune system, J Neural Transm, doi:10.1007/s00702-010-0479-3
Wee, COVID-19's toll on the elderly and those with diabetes mellitus -is vitamin B12 deficiency an accomplice?, Med Hypotheses, doi:10.1016/j.mehy
Weiss, Ganz, Goodnough, Anemia of inflammation, Blood, doi:10.1182/blood-2018-06-856500
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using, Open SAFELY
DOI record:
{
"DOI": "10.25279/sak.1102076",
"ISSN": [
"2548-1010"
],
"URL": "http://dx.doi.org/10.25279/sak.1102076",
"author": [
{
"affiliation": [],
"family": "DOĞAN",
"given": "Ahmet",
"sequence": "first"
},
{
"affiliation": [],
"family": "ANAÇ",
"given": "İsmail",
"sequence": "additional"
},
{
"affiliation": [],
"family": "GEZER",
"given": "Yakup",
"sequence": "additional"
},
{
"affiliation": [],
"family": "TİMUR",
"given": "Burcu",
"sequence": "additional"
}
],
"container-title": "Sağlık Akademisi Kastamonu",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
4,
21
]
],
"date-time": "2022-04-21T21:34:47Z",
"timestamp": 1650576887000
},
"deposited": {
"date-parts": [
[
2022,
4,
21
]
],
"date-time": "2022-04-21T21:34:55Z",
"timestamp": 1650576895000
},
"indexed": {
"date-parts": [
[
2022,
4,
22
]
],
"date-time": "2022-04-22T12:43:09Z",
"timestamp": 1650631389678
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
4,
21
]
]
},
"member": "10911",
"original-title": [],
"prefix": "10.25279",
"published": {
"date-parts": [
[
2022,
4,
21
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
21
]
]
},
"publisher": "Saglik Akademisi Kastamonu",
"reference": [
{
"DOI": "10.1186/s12967-020-02399-5",
"doi-asserted-by": "crossref",
"key": "ref1",
"unstructured": "1.\tDi Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med 2020;18:229."
},
{
"DOI": "10.1038/s41430-020-0635-2",
"doi-asserted-by": "crossref",
"key": "ref2",
"unstructured": "2.\tMuscogiuri G, Barrea L, Savastano S, Colao A. Nutritional recommendations for CoVID-19 quarantine. Eur J Clin Nutr 2020;74:850–1."
},
{
"DOI": "10.1093/jn/133.1.336S",
"doi-asserted-by": "crossref",
"key": "ref3",
"unstructured": "3.\tKeusch GT. The history of nutrition: malnutrition, infection and immunity. J Nutr 2003;133:336S–40S."
},
{
"DOI": "10.1301/00296640260130722",
"doi-asserted-by": "crossref",
"key": "ref4",
"unstructured": "4.\tBhaskaram P. Micronutrient malnutrition, infection and immunity: an overview. Nutr Rev 2002;60:S40–5."
},
{
"DOI": "10.1111/cga.12232",
"doi-asserted-by": "crossref",
"key": "ref5",
"unstructured": "5.\tHiraoka M, Kagawa Y. Genetic polymorphisms and folate status. Congenital Anomalies 2017; 57, 142–149."
},
{
"key": "ref6",
"unstructured": "6.\tGropper, S.S, Smith, J.L. Advanced Nutrition and Human Metabolism, 7th ed.; Cengage Learning: Belmont, CA, USA, 2017; ISBN 1305627857."
},
{
"DOI": "10.3109/00498254.2013.845705",
"doi-asserted-by": "crossref",
"key": "ref7",
"unstructured": "7.\tScaglione, F. Panzavolta, G. Folate, folic acid and 5-methyltetrahydrofolate are not the same thing. Xenobiotica 2014, 44, 480–488."
},
{
"DOI": "10.1016/j.cmet.2016.08.009",
"doi-asserted-by": "crossref",
"key": "ref8",
"unstructured": "8.\tDucker, G.S. Rabinowitz, J.D. One-Carbon Metabolism in Health and Disease. Cell Metab. 2017, 25, 27–42."
},
{
"DOI": "10.1016/S0163-4453(87)91827-5",
"doi-asserted-by": "crossref",
"key": "ref9",
"unstructured": "9.\tJacobson, W., Wreghitt, T.G., Saich, T., Nagington, J. Serum folate in viral and mycoplasmal infections. J. Infect. 1987, 14, 103–111."
},
{
"DOI": "10.1093/ajcn/86.1.139",
"doi-asserted-by": "crossref",
"key": "ref10",
"unstructured": "10.\t Strand, T.A., Taneja, S., Bhandari, N., et al. Folate, but not vitamin B-12 status, predicts respiratory morbidity in north Indian children. Am. J. Clin. Nutr. 2007, 86, 139–144."
},
{
"DOI": "10.3390/nu12041181",
"doi-asserted-by": "crossref",
"key": "ref11",
"unstructured": "11.\t Calder, P., Carr, A., Gombart, A., Eggersdorfer, M. Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients 2020, 12, 1181."
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"doi-asserted-by": "crossref",
"key": "ref12",
"unstructured": "12.\t Calder, P.C. Nutrition, immunity and COVID-19. BMJ Nutr. Prev. Health 2020, 3, 74–92."
},
{
"DOI": "10.3390/nu12010236",
"doi-asserted-by": "crossref",
"key": "ref13",
"unstructured": "13.\t Gombart, A.F., Pierre, A., Maggini, S. A Review of Micronutrients and the Immune System–Working in Harmony to Reduce the Risk of Infection. Nutrients 2020, 12, 236."
},
{
"key": "ref14",
"unstructured": "14.\t Batista K.S, Cintra V.M, Lucena P.A.F. The role of vitamin B12 in viral infections: a comprehensive review of its relationship with the muscle–gut–brain axis and implications for SARS-CoV-2 infection. Nutrition ReviewsVR Vol. 00(0):1–18."
},
{
"DOI": "10.1039/c8mt00146d",
"doi-asserted-by": "crossref",
"key": "ref15",
"unstructured": "15.\t Andreini C, Putignano V, Rosato A, Banci L. The human ironproteome. Metallomics 2018;10:1223–31."
},
{
"DOI": "10.1038/nrmicro1930",
"doi-asserted-by": "crossref",
"key": "ref16",
"unstructured": "16.\t Drakesmith H, Prentice A. Viral infection and iron metabolism. Nat Rev Microbiol 2008;6:541–52."
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "crossref",
"key": "ref17",
"unstructured": "17.\t Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020;584:430–6."
},
{
"DOI": "10.3390/nu13030812",
"doi-asserted-by": "crossref",
"key": "ref18",
"unstructured": "18.\t Meisel E, Efros O, Bleier J, Beit Halevi T, Segal G, Rahav G, Leibowitz A, Grossman E. Folate Levels in Patients Hospitalized with Coronavirus Disease 2019. Nutrients. 2021 Mar 2;13(3):812."
},
{
"key": "ref19",
"unstructured": "19.\t Itelman E, Wasserstrum Y, Segev A, Avaky C, Negru L, Cohen D, et al. Clinical Characterization of 162 COVID-19 patients in Israel: Preliminary Report from a Large Tertiary Center. Isr Med Assoc J. 2020 May;22(5):271-274."
},
{
"DOI": "10.3389/fphar.2020.01062",
"doi-asserted-by": "crossref",
"key": "ref20",
"unstructured": "20.\t Acosta-Elias J and Espinosa-Tanguma R (2020). The Folate Concentration and/or Folic Acid Metabolites in Plasma as Factor for COVID-19 Infection. Front. Pharmacol. 11:1062."
},
{
"DOI": "10.2174/1871530319666190529101816",
"doi-asserted-by": "crossref",
"key": "ref21",
"unstructured": "21.\t Elmadfa I, Meyer AL. The Role of the Status of Selected Micronutrients in Shaping the Immune Function. Endocr Metab Immune Disord Drug Targets. 2019;19(8):1100-1115."
},
{
"DOI": "10.1016/j.mehy.2020.110374",
"doi-asserted-by": "crossref",
"key": "ref22",
"unstructured": "22.\t Andrew Kien HanWee. COVID-19’s toll on the elderly and those with diabetes mellitus – Is vitamin B12 deficiency an accomplice? Medical Hypotheses 146 (2021) 110374."
},
{
"DOI": "10.1053/jcrc.2001.21795",
"doi-asserted-by": "crossref",
"key": "ref23",
"unstructured": "23.\t Rodriguez RM, Corwin HL, Gettinger A, Corwin MJ, Gubler D, Pearl RG. Nutritional deficiencies and blunted erythropoietin response as causes of the anemia of critical illness. J Crit Care 2001;16:36e41."
},
{
"DOI": "10.1182/blood-2018-06-856500",
"doi-asserted-by": "crossref",
"key": "ref24",
"unstructured": "24.\t Weiss, G.; Ganz, T.; Goodnough, L.T. Anemia of inflammation. Blood, 2019, 133(1), 40-50."
},
{
"DOI": "10.1007/s00702-010-0479-3",
"doi-asserted-by": "crossref",
"key": "ref25",
"unstructured": "25.\t Ward, R.J.; Crichton, R.R.; Taylor, D.L.; Della Corte, L.; Srai, S.K.; Dexter, D.T. Iron and the immune system. J. Neural Transm. (Vienna), 2011, 118(3), 315-328."
}
],
"reference-count": 25,
"references-count": 25,
"relation": {},
"resource": {
"primary": {
"URL": "https://dergipark.org.tr/en/doi/10.25279/sak.1102076"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"title": "Folate, B12 and Iron Levels in COVID 19 Patients Observational Case-Control Study",
"type": "journal-article"
}