Vitamin D in COVID-19
et al., International Journal of Clinical Biochemistry and Research, doi:10.18231/j.ijcbr.2023.007, Apr 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 88 PCR+ COVID-19 cases and 88 matched COVID-19 negative controls in India showing lower vitamin D levels and higher prevalence of vitamin D deficiency in COVID-19 patients.
This is the 175th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of case, 98.0% lower, OR 0.02, p = 0.007, high D levels (≥10ng/mL) 69 of 88 (78.4%) cases,
88 of 88 (100.0%) controls, NNT 1.8, case control OR.
|
|
risk of case, 88.4% lower, OR 0.12, p < 0.001, high D levels (≥20ng/mL) 54 of 88 (61.4%) cases,
82 of 88 (93.2%) controls, NNT 2.2, case control OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Devi et al., 15 Apr 2023, retrospective, India, peer-reviewed, mean age 47.0, 4 authors, study period August 2020 - August 2022.
Contact: vidyarajkumari@gmail.com.
Vitamin D in COVID-19
International Journal of Clinical Biochemistry and Research, doi:10.18231/j.ijcbr.2023.007
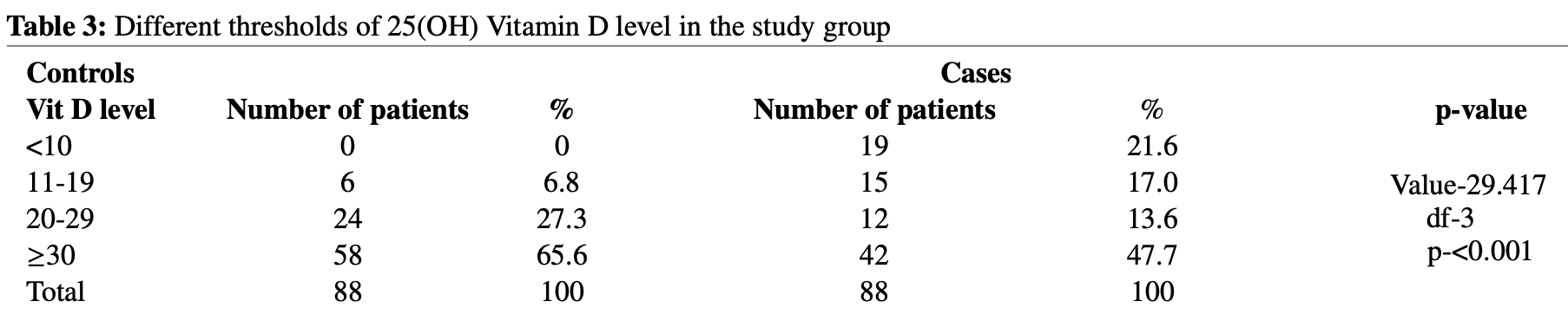
Background: Severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) causes coronavirus disease 2019 (COVID-19) with clinical outcome ranging from asymptomatic to severe disease, and even death to some. It posed a terrifying challenge to healthcare system worldwide. Several observational and clinical trials has reported that, Vitamin D deficiency has contributed to acute respiratory distress syndrome. Case fatality rate increases with age and comorbidities, both of which are associated with decreased Vitamin D level. Therefore, this study is done to study the prevalence of 25(OH)Vitamin D in RT-PCR positive COVID-19 cases and RT-PCR negative controls. Materials and Methods: This is a hospital based cross-sectional study conducted at Jawaharlal Nehru Institute of Medical Sciences, Manipur on 88 RT-PCR positive Covid-19 cases and 88 COVID-19 negative controls over a period of 2 years. Analysis of the sample was done by Liaison 25(OH) Vitamin D Total Chemiluminescence assay(CLIA). Result: In this study, statistically significant (p-0.018) lower plasma 25(OH)Vitamin D level is seen in COVID-19 positive cases (median 28±20.47) when compared to Covid-19 negative controls(median 33.50±10.66). The number of 25(OH) Vitamin D deficient is higher in Covid-19 positive cases when compared to Covid-19 negative controls -46(52.3%) and 30(34%) respectively with a high statistically significant value (p-0.015). Conclusion: COVID-19 positive cases have higher tendency to have suboptimal plasma 25(OH) Vitamin D level which may contribute to the high hospitalization risk in COVID-19 infection. This finding is important as it can identify population at risk, and contribute to interventions in reducing the risk of hospitalization associated with COVID-19 infection.
References
Alipio, Vitamin D Supplementation Could Possibly Improve Clinical Outcomes of Patients Infected with Coronavirus-2019 (COVID-2019, doi:10.2139/ssrn.3571484
Azrielant, Shoenfeld, Vitamin D and the Immune System, Isr Med Assoc J
Bassatne, Basbous, Chakhtoura, Zein, Rahme et al., The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis, Metabolism, doi:10.1016/j.metabol.2021.154753
Bianconi, Violi, Fallarino, Pignatelli, Sahebkar et al., Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19?, Drugs
Boucher, The problems of vitamin D insufficiency in older people, Aging Dis
Crane-Godreau, Clem, Payne, Fiering, Vitamin D deficiency and air pollution exacerbate COVID-19 through suppression of antiviral peptide LL37, Front Public Health
D'avolio, Avataneo, Manca, Cusato, Denicolò et al., 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2, Nutrients
Daniel, Sartory, Zahn, Radeke, Stein, Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitriol is associated with a change of a T helper (Th) 1/Th17 to a Th2 and regulatory T cell profile, J Pharmacol Exp Ther
Fabbri, Infante, Ricordi, Editorial -Vitamin D status: a key modulator of innate immunity and natural defense from acute viral respiratory infections, Eur Rev Med Pharmacol Sci
Ghavideldarestani, Honardoost, Khamseh, Role of vitamin D in pathogenesis and severity of COVID-19 infection, doi:10.20944/preprints202004.0355.v1
Hribar, Cobbold, Church, Potential role of vitamin D in the Elderly to resist COVID-19 and to slow progression of Parkinson's disease, Brain Sci, doi:10.3390/brainsci10050284
Jose, Manuel, COVID-19 cytokine storm: the interplay between inflammation and coagulation, Lancet Respir Med
Kara, Ekiz, Ricci, Kara, Chang et al., Scientific Strabismus' or two related pandemics: coronavirus disease and vitamin D deficiency, Br J Nutr
Laird, Rhodes, Kenny, Vitamin D and Inflammation -Potential Implications for Severity of Covid-19, Ir Med J
Mcgonagle, Sharif, 'regan, Bridgewood, The Role of Cytokines including Interleukin-6 in COVID-19 induced Pneumonia and Macrophage Activation Syndrome-Like Disease, Autoimmun Rev, doi:10.1016/j.autrev.2020.102537
Raharusun, Priambada, Budiarti, Agung, Budi, Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study
Rosenthal, Cao, Gundrum, Sianis, Safo, Risk factors associated with in-hospital mortality in a U.S. national sample of patients with COVID-19, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.29058
Ye, Tang, Liao, Shaw, Deng et al., Does serum vitamin D level affect COVID-19 infection and its severity? -A casecontrol study, J Am Coll Nutr
DOI record:
{
"DOI": "10.18231/j.ijcbr.2023.007",
"ISSN": [
"2394-6369",
"2394-6377"
],
"URL": "http://dx.doi.org/10.18231/j.ijcbr.2023.007",
"abstract": "<jats:p>Severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) causes coronavirus disease 2019 (COVID-19) with clinical outcome ranging from asymptomatic to severe disease, and even death to some. It posed a terrifying challenge to healthcare system worldwide. Several observational and clinical trials has reported that, Vitamin D deficiency has contributed to acute respiratory distress syndrome. Case fatality rate increases with age and comorbidities, both of which are associated with decreased Vitamin D level. Therefore, this study is done to study the prevalence of 25(OH)Vitamin D in RT-PCR positive COVID-19 cases and RT-PCR negative controls.</jats:p><jats:p>This is a hospital based cross-sectional study conducted at Jawaharlal Nehru Institute of Medical Sciences, Manipur on 88 RT-PCR positive Covid-19 cases and 88 COVID-19 negative controls over a period of 2 years. Analysis of the sample was done by Liaison 25(OH) Vitamin D Total Chemiluminescence assay(CLIA).</jats:p><jats:p>In this study, statistically significant (p-0.018) lower plasma 25(OH)Vitamin D level is seen in COVID-19 positive cases (median 28±20.47) when compared to Covid-19 negative controls(median 33.50±10.66). The number of 25(OH) Vitamin D deficient is higher in Covid-19 positive cases when compared to Covid-19 negative controls -46(52.3%) and 30(34%) respectively with a high statistically significant value (p-0.015).</jats:p><jats:p>COVID-19 positive cases have higher tendency to have suboptimal plasma 25(OH) Vitamin D level which may contribute to the high hospitalization risk in COVID-19 infection. This finding is important as it can identify population at risk, and contribute to interventions in reducing the risk of hospitalization associated with COVID-19 infection.</jats:p>",
"assertion": [
{
"label": "Peer Reviewed",
"name": "peer_reviewed",
"value": "Yes"
},
{
"label": "Content Type",
"name": "content_type",
"value": "Original Article"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "18-02-2023"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "02-03-2023"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "05-04-2023"
},
{
"explanation": {
"URL": "https://creativecommons.org/licenses/by/4.0/"
},
"group": {
"label": "Rights",
"name": "rights"
},
"label": "License",
"name": "license",
"value": "Creative Commons Attribution"
}
],
"author": [
{
"affiliation": [],
"family": "Devi",
"given": "R K Vidyabati",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-8491-4971",
"affiliation": [],
"authenticated-orcid": true,
"family": "Lian",
"given": "Niangngaih",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Singh",
"given": "Thokchom Opendro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Devi",
"given": "Chungkham Rebika",
"sequence": "additional"
}
],
"container-title": "International Journal of Clinical Biochemistry and Research",
"container-title-short": "IJCBR",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"ijcbr.in",
"ipinnovative.com"
]
},
"created": {
"date-parts": [
[
2023,
4,
5
]
],
"date-time": "2023-04-05T09:05:26Z",
"timestamp": 1680685526000
},
"deposited": {
"date-parts": [
[
2023,
4,
5
]
],
"date-time": "2023-04-05T09:09:23Z",
"timestamp": 1680685763000
},
"indexed": {
"date-parts": [
[
2023,
4,
6
]
],
"date-time": "2023-04-06T05:00:53Z",
"timestamp": 1680757253783
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2023,
4,
15
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2023,
4,
15
]
]
},
"published-print": {
"date-parts": [
[
2023,
4,
28
]
]
}
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-sa/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
5
]
],
"date-time": "2023-04-05T00:00:00Z",
"timestamp": 1680652800000
}
}
],
"link": [
{
"URL": "https://ijcbr.in/media/journals/xml/IntJClinBiochemRes-10-1-50-54.xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://ijcbr.in/journal-article-file/18593",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "9296",
"original-title": [],
"page": "50-54",
"prefix": "10.18231",
"published": {
"date-parts": [
[
2023,
4,
15
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
15
]
]
},
"published-print": {
"date-parts": [
[
2023,
4,
28
]
]
},
"publisher": "IP Innovative Publication Pvt Ltd",
"reference": [
{
"DOI": "10.1007/s40265-020-01365-1",
"doi-asserted-by": "crossref",
"key": "ref1",
"unstructured": "Bianconi V, Violi F, Fallarino F, Pignatelli P, Sahebkar A, Pirro M, Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19?.Drugs 2020;80(14):1383-96"
},
{
"DOI": "10.1001/jamanetworkopen.2020.29058",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1016/j.autrev.2020.102537",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1016/S2213-2600(20)30216-2",
"doi-asserted-by": "crossref",
"key": "ref4",
"unstructured": "Jose RJ, Manuel A, COVID-19 cytokine storm: the interplay between inflammation and coagulation.Lancet Respir Med 2020;8(6):46-7"
},
{
"key": "ref5",
"unstructured": "Azrielant S, Shoenfeld Y, Vitamin D and the Immune System.Isr Med Assoc J 2017;19(8):510-1"
},
{
"DOI": "10.1124/jpet.107.127209",
"doi-asserted-by": "crossref",
"key": "ref6",
"unstructured": "Daniel C, Sartory NA, Zahn N, Radeke HH, Stein JM, Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitriol is associated with a change of a T helper (Th) 1/Th17 to a Th2 and regulatory T cell profile.J Pharmacol Exp Ther 2008;324(1):23-33"
},
{
"DOI": "10.1017/S0007114520001749",
"doi-asserted-by": "crossref",
"key": "ref7",
"unstructured": "Kara M, Ekiz T, Ricci V, Kara Ö, Chang KV, Özçakar L, Scientific Strabismus’ or two related pandemics: coronavirus disease and vitamin D deficiency.Br J Nutr 2020;124(7):736-41"
},
{
"key": "ref8",
"unstructured": "Does serum vitamin D level affect COVID-19 infection and its severity? -A case-control study.."
},
{
"DOI": "10.2139/ssrn.3571484",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"key": "ref10",
"unstructured": "Raharusun P, Priambada S, Budiarti C, Agung E, Budi C, Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study.Emerginnova."
},
{
"key": "ref11",
"unstructured": "Laird E, Rhodes J, Kenny RA, Vitamin D and Inflammation - Potential Implications for Severity of Covid-19.Ir Med J 2020;113(5):81"
},
{
"DOI": "10.3390/brainsci10050284",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"key": "ref13",
"unstructured": "Fabbri A, Infante M, Ricordi C, Editorial - Vitamin D status: a key modulator of innate immunity and natural defense from acute viral respiratory infections.Eur Rev Med Pharmacol Sci 2020;24(7):4048-52"
},
{
"key": "ref14",
"unstructured": "Boucher BJ, The problems of vitamin D insufficiency in older people.Aging Dis 2012;3(4):313-29"
},
{
"DOI": "10.3389/fpubh.2020.00232",
"doi-asserted-by": "crossref",
"key": "ref15",
"unstructured": "Crane-Godreau MA, Clem KJ, Payne P, Fiering S, Vitamin D deficiency and air pollution exacerbate COVID-19 through suppression of antiviral peptide LL37.Front Public Health 2020;8:232"
},
{
"DOI": "10.20944/preprints202004. 0355.v1",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.3390/nu12051359",
"doi-asserted-by": "crossref",
"key": "ref17",
"unstructured": "D'Avolio A, Avataneo V, Manca A, Cusato J, DeNicolò A, Lucchini R, 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2.Nutrients 2020;12(5):1359"
},
{
"DOI": "10.1080/07315724.2020.1826005",
"doi-asserted-by": "crossref",
"key": "ref18",
"unstructured": "Ye K, Tang F, Liao X, Shaw BA, Deng M, Huang G, Does serum vitamin D level affect COVID-19 infection and its severity? -A case-control study.J Am Coll Nutr 2020;13:1-8"
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"doi-asserted-by": "publisher",
"key": "ref19"
}
],
"reference-count": 19,
"references-count": 19,
"relation": {},
"resource": {
"primary": {
"URL": "https://ijcbr.in/article-details/18593"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Vitamin D in COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.18231/ip-innovative-publication-crossmark-policy",
"volume": "10"
}
