Shadowing SARS-CoV-2 Through Mucus and Cilia
, S., DDN, Jan 2023
Discussion of Wu et al. on how SARS-CoV-2 invades and spreads through nasal epithelial cells.
Demarco et al., 31 Jan 2023, preprint, 1 author.
Abstract: infectious disease
Shadowing SARS-CoV-2 Through Mucus and Cilia
Researchers discovered how SARS-CoV-2 invades and spreads through nasal epithelial cells, identifying
potential new drug targets to prevent transmission.
W
BY STEPHANIE DEMARCO, PHD
Microvilli escape routes
After figuring out how SARS-CoV-2 enters
the cells, the researchers wanted to know
images of the month
CREDIT: CHIEN-TING WU
Mucin barriers and cilia ladders
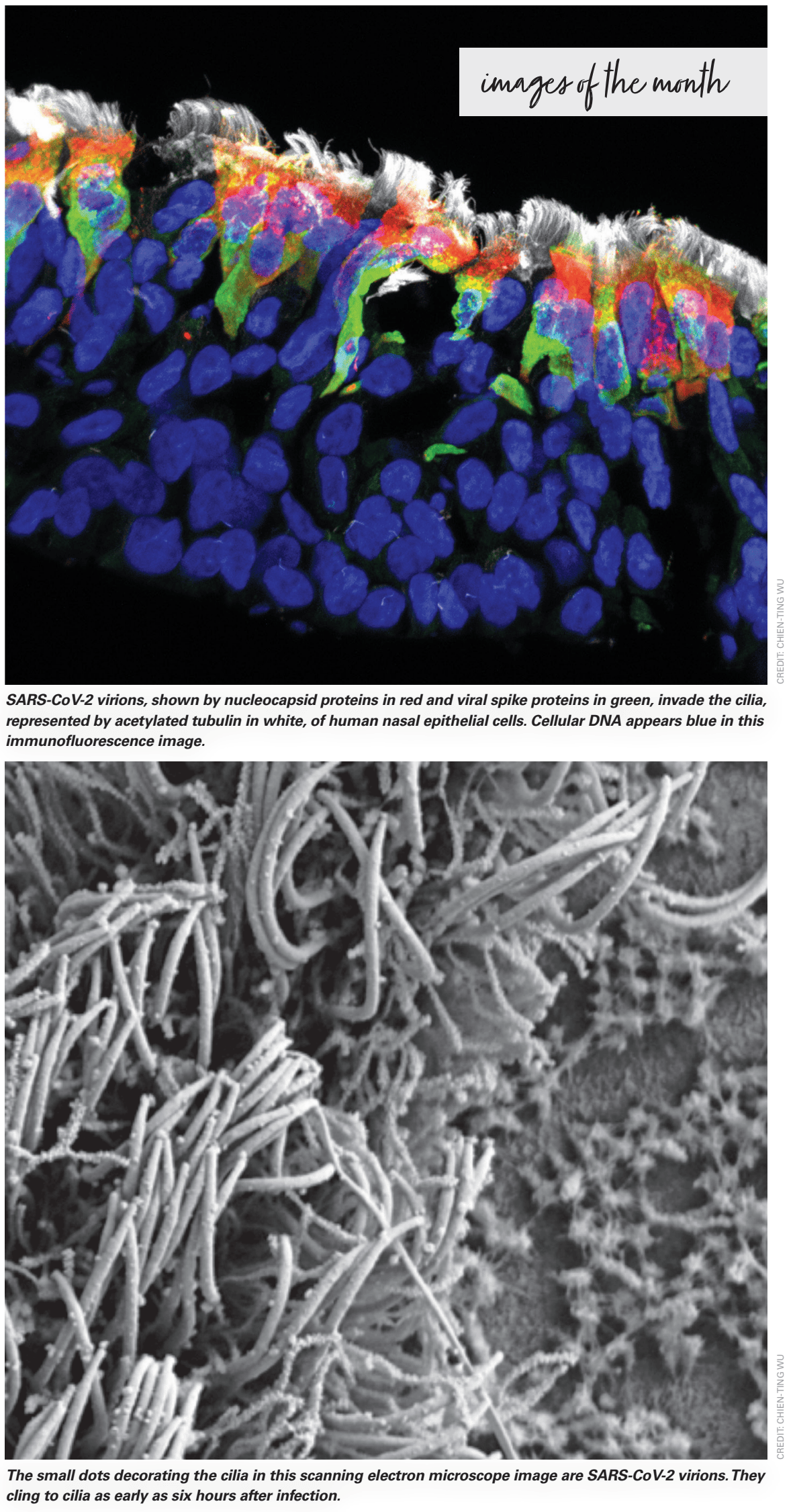
To refine their idea of how quickly SARSCoV-2 binds to cilia after infection, the team
relied on the lead author, Chien-Ting Wu’s
expertise in electron microscopy (EM) to
take scanning EM images of the organoids
soon after SARS-CoV-2 infection. Wu, who
is now a virologist at UT Southwestern,
observed virions dotted all over the cilia as
soon as six hours after infection.
The researchers wondered why the virus
took 24 to 48 hours to infect the cells if
they reached the cilia in only six hours. In
cell culture experiments, Jackson said, “the
virus gets into the cell in about 10 minutes.”
They hypothesized that the mucus layer,
which was absent in cell culture experiments, slowed the virus down.
To crack this mystery, the researchers
treated the organoids with mucinase, an
enzyme that digests the main component
of mucus called mucins, and infected the
organoids with SARS-CoV-2. The virus
invaded the cells much faster than before.
“When you accept that the mucins
are the barrier, what does the cilia
do?” Jackson asked.
The team then knocked down cilia in
the organoids and found that SARS-CoV-2
couldn’t enter the cells at all. They even
showed that other respiratory viruses
including respiratory syncytial virus (RSV)
and parainfluenza virus (PIV) also couldn’t
infect the nasal epithelial cells without cilia.
“That confirmed the model that the virus
needed these little portals or ladders to
crawl through the mucous,” said Jackson.
“The cilia are kind of like the ladders that
the army in Game of Thrones uses to climb
up the walls of the castle and attack.”
how the virus climbs back out and spreads
to other nasal epithelial cells.
To find out, the researchers used transmission EM to visualize the nasal epithelial
cells after infection and noticed that emerging SARS-CoV-2 virions clustered around
what looked like brand new structures.
Normally, cells can form extensions called
microvilli that look similar to cilia but are
nonmotile and typically shorter. But the
researchers saw that the SARS-CoV-2 infected nasal epithelial cells formed extremely
long and more branched microvilli than
they had ever seen before. The uninfected
cells did not form these structures.
SARS-CoV-2 virions, shown by nucleocapsid proteins in red and viral spike proteins in green, invade the cilia,
represented by acetylated tubulin in white, of human nasal epithelial cells. Cellular DNA appears blue in this
immunofluorescence image.
Using transmission EM, the researchers observed SARS-CoV-2 virions — the circular structures — exiting
abnormally branched and extended microvilli.
“When you infect
with the virus, the
microvilli, they branch,
and that’s just crazy. I
don’t think anyone had
ever observed that.”
– Peter Jackson,
Stanford University
“If you look at some of the EM pictures,
they’re really kind of amazing,” said Jackson.
“When you infect with the virus, the microvilli, they branch, and that’s just crazy. I
don’t think anyone had ever observed that.”
The small dots decorating the cilia in this scanning electron microscope image are..