Androgen deprivation therapy in men with prostate cancer is not associated with COVID‐2019 infection
et al., The Prostate, doi:10.1002/pros.24485, Jan 2023
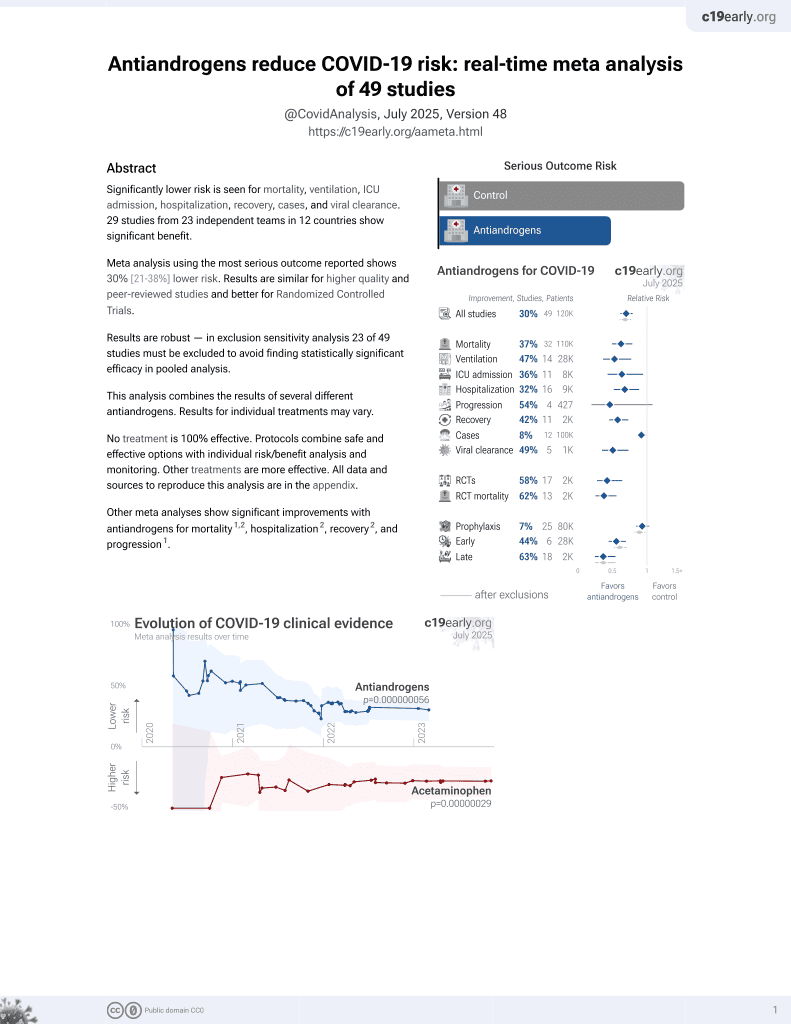
7th treatment shown to reduce risk in
September 2020, now with p = 0.000000056 from 49 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 655 prostate cancer patients in Sweden, showing no significant difference in seropositivity with ADT.
|
risk of IgG positive, 1.8% lower, RR 0.98, p = 0.95, treatment 30 of 224 (13.4%), control 45 of 431 (10.4%), adjusted per study, odds ratio converted to relative risk, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Davidsson et al., 19 Jan 2023, retrospective, Sweden, peer-reviewed, 10 authors.
Contact: sabina.davidsson@regionorebrolan.se.
Androgen deprivation therapy in men with prostate cancer is not associated with COVID‐19 infection
The Prostate, doi:10.1002/pros.24485
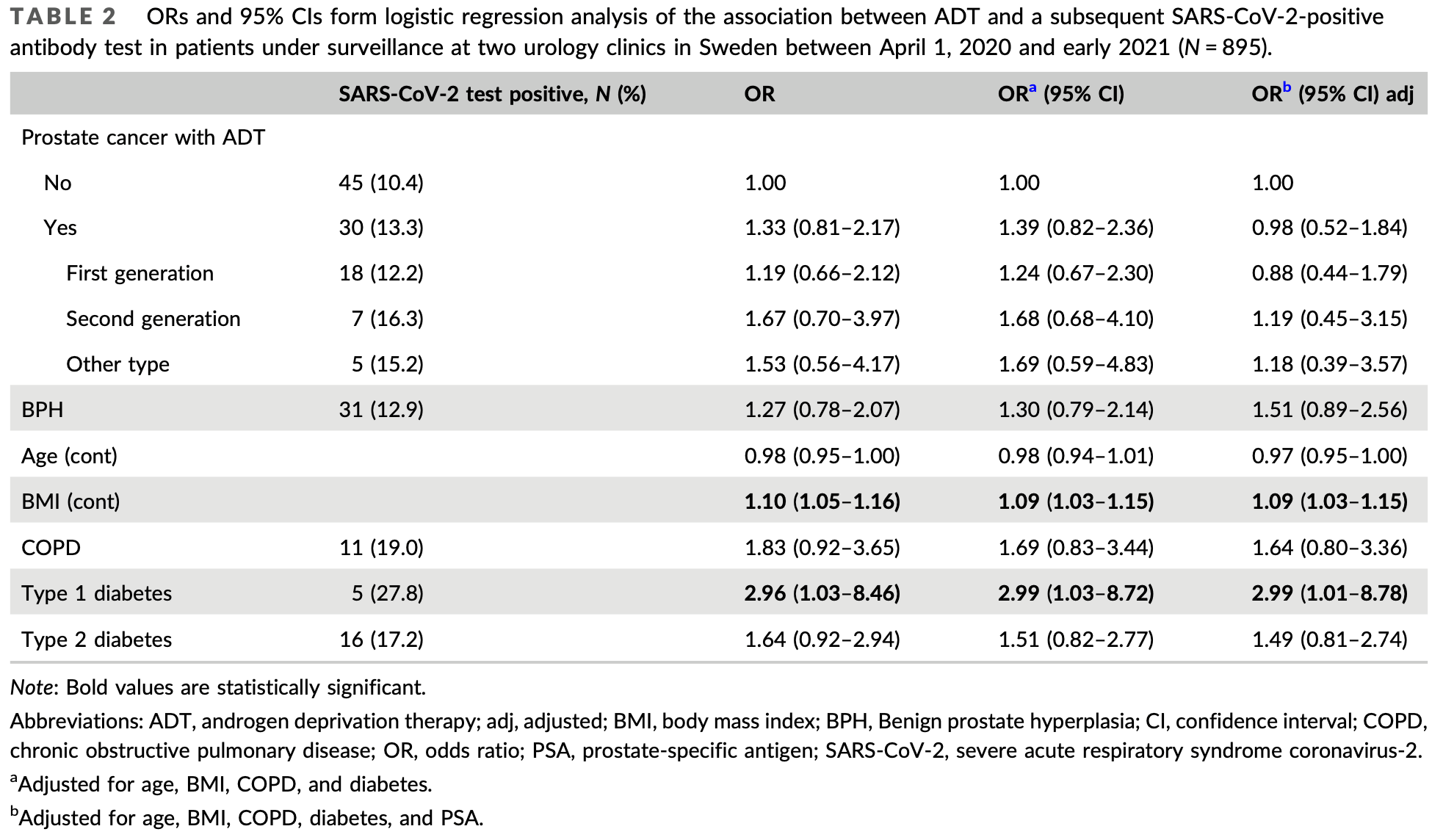
Background: Androgens may play a role in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection and host responses as the virus is dependent on the androgen-regulated protein transmembrane serine protease 2 for cell entry. Studies have indicated that prostate cancer patients receiving androgen deprivation therapy (ADT) are at reduced risk of SARS-CoV-2 infection and serious complications compared with patients without ADT, but data are inconsistent. Methods: A total of 655 prostate cancer patients who were under surveillance at two urology departments in Sweden on April 1, 2020 were included in the study as well as 240 patients with benign prostatic hyperplasia (BPH). At follow-up early in 2021, the participants completed a questionnaire containing information about symptoms compatible with coronavirus disease 2019 (COVID-19). Blood samples were also collected for the assessment of SARS-CoV-2 IgG antibodies (SARS-CoV-2 Total; Siemens). We used multivariable logistic regression models to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for the association between ADT and the risk of SARS-CoV-2 infection.
Results: The cumulative incidence of SARS-CoV-2 seropositivity was 13.4% among patients receiving ADT and 10.4% among patients without ADT. After adjusting for potential confounders, we observed no differences in symptoms or risk of SARS-CoV-2 infection between patients with and without ADT (OR: 0.98; 95% CI: 0.52-1.85). Higher body mass index, Type 1 diabetes, and prostate cancer severity, defined by high Gleason score (8-10; OR: 2.06; 95% CI: 1.04-4.09) or elevated levels of prostate-specific antigen (>20 µg/l; OR: 2.15; 95% CI: 1.13-4.07) were associated with increased risk of SARS-CoV-2 infection. Overall, the risk of SARS-CoV-2 infection was not higher among men with prostate cancer than among men with BPH. Conclusions: Our results do not support the hypothesis that ADT use in prostate cancer patients reduces the risk or symptom severity of SARS-CoV-2 infection or
CONFLICT OF INTEREST The authors declare no conflict of interest.
References
Bonelli, Sarasini, Zierold, Clinical and analytical performance of an automated serological test that identifies S1/ S2-neutralizing IgG in COVID-19 patients semiquantitatively, J Clin Microbiol
Borges Do Nascimento, Cacic, Abdulazeem, Novel coronavirus infection (COVID-19) in humans: a scoping review and meta-analysis, J Clin Med
Caffo, Gasparro, Lorenzo, Incidence and outcomes of severe acute respiratory syndrome coronavirus 2 infection in patients with metastatic castration-resistant prostate cancer, Eur J Cancer
Duarte, Leal, Argenton, Carvalheira, Impact of androgen deprivation therapy on mortality of prostate cancer patients with COVID-19: a propensity score-based analysis, Infect Agent Cancer
Gedeborg, Lindhagen, Loeb, Styrke, Garmo et al., Androgen deprivation therapy, comorbidity, cancer stage and mortality from COVID-19 in men with prostate cancer, Scand J Urol
Gooden, De Bock, Leffers, Daemen, Nijman, The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis, Br J Cancer
Hadrup, Donia, Thor Straten, Effector CD4 and CD8 T cells and their role in the tumor microenvironment, Cancer Microenviron
Hua, Xia, Zheng, The association between immune infiltration and clinical phenotypes and prognosis of prostate cancer, Iran J Biotechnol
Idorn, Køllgaard, Kongsted, Sengeløv, Thor Straten, Correlation between frequencies of blood monocytic myeloidderived suppressor cells, regulatory T cells and negative prognostic markers in patients with castration-resistant metastatic prostate cancer, Cancer Immunol Immunother
Jiang, Markovic, Patel, Radiation therapy dose and androgen deprivation therapy in localized prostate cancer: a metaregression of 5-year outcomes in phase III randomized controlled trials, Prostate Cancer Prostatic Dis
Jiménez-Alcaide, García-Fuentes, Hernández, Influence of androgen deprivation therapy on the severity of COVID-19 in prostate cancer patients, Prostate
Kheshtchin, Bakhshi, Arab, Nourizadeh, Immunoediting in SARS-CoV-2: mutual relationship between the virus and the host, Int Immunopharmacol
Klein, Li, Milinovich, Androgen deprivation therapy in men with prostate cancer does not affect risk of infection with SARS-CoV-2, J Urol
Koskinen, Carpen, Honkanen, Androgen deprivation and SARS-CoV-2 in men with prostate cancer, Ann Oncol
Kwon, Vashisht, Borno, Androgen-deprivation therapy and SARS-CoV-2 in men with prostate cancer: findings from the University of California Health System registry, Ann Oncol
Lanciotti, Masieri, Raspollini, The role of M1 and M2 macrophages in prostate cancer in relation to extracapsular tumor extension and biochemical recurrence after radical prostatectomy, BioMed Res Int
Lawton, Men hit harder by covid-19, New Sci
Li, Han, Dai, Distinct mechanisms for TMPRSS2 expression explain organ-specific inhibition of SARS-CoV-2 infection by enzalutamide, Nat Commun
Meng, Zhou, Lu, Immune response drives outcomes in prostate cancer: implications for immunotherapy, Mol Oncol
Montopoli, Zumerle, Vettor, Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532), Ann Oncol
Motlagh, Abufaraj, Karakiewicz, Association between SARS-CoV-2 infection and disease severity among prostate cancer patients on androgen deprivation therapy: a systematic review and meta-analysis, World J Urol
Patel, Zhong, Liaw, Does androgen deprivation therapy protect against severe complications from COVID-19?, Ann Oncol
Royston, Sauerbrei, Building multivariable regression models with continuous covariates in clinical epidemiology-with an emphasis on fractional polynomials, Methods Inf Med
Shah, Patel, Zhong, The impact of androgen deprivation therapy on COVID-19 illness in men with prostate cancer, JNCI Cancer Spectr
Stopsack, Mucci, Antonarakis, Nelson, Kantoff, TMPRSS2 and COVID-19: serendipity or opportunity for intervention?, Cancer Discov
Wambier, Goren, Vaño-Galván, Androgen sensitivity gateway to COVID-19 disease severity, Drug Dev Res
Welén, Rosendal, Gisslén, A phase 2 trial of the effect of antiandrogen therapy on COVID-19 outcome: no evidence of benefit, supported by epidemiology and in vitro data, Eur Urol
Yazdanpanah, Hamblin, Rezaei, Udumyan, Androgen deprivation therapy in men with prostate cancer is not associated with COVID-2019 infection, The Prostate
DOI record:
{
"DOI": "10.1002/pros.24485",
"ISSN": [
"0270-4137",
"1097-0045"
],
"URL": "http://dx.doi.org/10.1002/pros.24485",
"alternative-id": [
"10.1002/pros.24485"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2022-09-19"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2022-12-28"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2023-01-19"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-2850-6009",
"affiliation": [
{
"name": "Department of Urology, Faculty of Medicine and Health, Örebro University Hospital Örebro University Örebro Sweden"
}
],
"authenticated-orcid": false,
"family": "Davidsson",
"given": "Sabina",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Urology, Faculty of Medicine and Health, Örebro University Hospital Örebro University Örebro Sweden"
}
],
"family": "Messing Eriksson",
"given": "Anna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "School of Medical Sciences, Faculty of Medicine and Health Örebro University Örebro Sweden"
}
],
"family": "Udumyan",
"given": "Ruzan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Urology Karlstad Central Hospital Karlstad Sweden"
}
],
"family": "Swanholm",
"given": "Per",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Urology Karlstad Central Hospital Karlstad Sweden"
}
],
"family": "Lewin Lundh",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Urology, Faculty of Medicine and Health, Örebro University Hospital Örebro University Örebro Sweden"
}
],
"family": "Widing",
"given": "Carolina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Urology, Faculty of Medicine and Health, Örebro University Hospital Örebro University Örebro Sweden"
}
],
"family": "Lindlöf",
"given": "Christina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Urology, Faculty of Medicine and Health, Örebro University Hospital Örebro University Örebro Sweden"
}
],
"family": "Fridfeldt",
"given": "Jonna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Urology, Faculty of Medicine and Health, Örebro University Hospital Örebro University Örebro Sweden"
}
],
"family": "Andersson",
"given": "Sven‐Olof",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "School of Medical Sciences, Faculty of Medicine and Health Örebro University Örebro Sweden"
}
],
"family": "Fall",
"given": "Katja",
"sequence": "additional"
}
],
"container-title": "The Prostate",
"container-title-short": "The Prostate",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2023,
1,
20
]
],
"date-time": "2023-01-20T05:40:11Z",
"timestamp": 1674193211000
},
"deposited": {
"date-parts": [
[
2023,
3,
23
]
],
"date-time": "2023-03-23T11:12:35Z",
"timestamp": 1679569955000
},
"indexed": {
"date-parts": [
[
2023,
3,
24
]
],
"date-time": "2023-03-24T04:35:02Z",
"timestamp": 1679632502190
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2023,
1,
19
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2023,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
1,
19
]
],
"date-time": "2023-01-19T00:00:00Z",
"timestamp": 1674086400000
}
},
{
"URL": "http://doi.wiley.com/10.1002/tdm_license_1.1",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
1,
19
]
],
"date-time": "2023-01-19T00:00:00Z",
"timestamp": 1674086400000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/pros.24485",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/full-xml/10.1002/pros.24485",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/pros.24485",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"page": "555-562",
"prefix": "10.1002",
"published": {
"date-parts": [
[
2023,
1,
19
]
]
},
"published-online": {
"date-parts": [
[
2023,
1,
19
]
]
},
"published-print": {
"date-parts": [
[
2023,
5
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1016/S0262-4079(20)30786-7",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_2_1"
},
{
"DOI": "10.3390/jcm9040941",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_3_1"
},
{
"DOI": "10.1002/ddr.21688",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_4_1"
},
{
"DOI": "10.1158/2159-8290.CD-20-0451",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_5_1"
},
{
"DOI": "10.1016/j.annonc.2020.04.479",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_6_1"
},
{
"DOI": "10.1016/j.annonc.2020.06.023",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_7_1"
},
{
"DOI": "10.1016/j.annonc.2020.06.015",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_8_1"
},
{
"DOI": "10.1016/j.ejca.2020.09.018",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_9_1"
},
{
"DOI": "10.1097/JU.0000000000001338",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_10_1"
},
{
"DOI": "10.1016/j.annonc.2021.01.067",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_11_1"
},
{
"DOI": "10.1128/JCM.01224-20",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_12_1"
},
{
"DOI": "10.1055/s-0038-1634008",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_13_1"
},
{
"DOI": "10.1038/s41391-021-00432-2",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_14_1"
},
{
"DOI": "10.1016/j.eururo.2021.12.013",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_15_1"
},
{
"DOI": "10.1080/21681805.2021.2019304",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_16_1"
},
{
"DOI": "10.1186/s13027-021-00406-y",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_17_1"
},
{
"DOI": "10.1002/pros.24232",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_18_1"
},
{
"DOI": "10.1093/jncics/pkac035",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_19_1"
},
{
"DOI": "10.1007/s00345-021-03810-6",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_20_1"
},
{
"DOI": "10.1038/s41467-021-21171-x",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_21_1"
},
{
"DOI": "10.1038/bjc.2011.189",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_22_1"
},
{
"DOI": "10.1007/s12307-012-0127-6",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_23_1"
},
{
"article-title": "The association between immune infiltration and clinical phenotypes and prognosis of prostate cancer",
"author": "Hua L",
"first-page": "2538",
"journal-title": "Iran J Biotechnol",
"key": "e_1_2_9_24_1",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1002/1878-0261.12887",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_25_1"
},
{
"DOI": "10.1155/2014/486798",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_26_1"
},
{
"DOI": "10.1007/s00262-014-1591-2",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_27_1"
},
{
"DOI": "10.1016/j.intimp.2022.108531",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_28_1"
},
{
"DOI": "10.1016/j.lfs.2020.117900",
"doi-asserted-by": "publisher",
"key": "e_1_2_9_29_1"
}
],
"reference-count": 28,
"references-count": 28,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/pros.24485"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Urology",
"Oncology"
],
"subtitle": [],
"title": "Androgen deprivation therapy in men with prostate cancer is not associated with COVID‐2019 infection",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy",
"volume": "83"
}