Distinct temporal trajectories and risk factors for Post-acute sequelae of SARS-CoV-2 infection
et al., Frontiers in Medicine, doi:10.3389/fmed.2023.1227883, Oct 2023
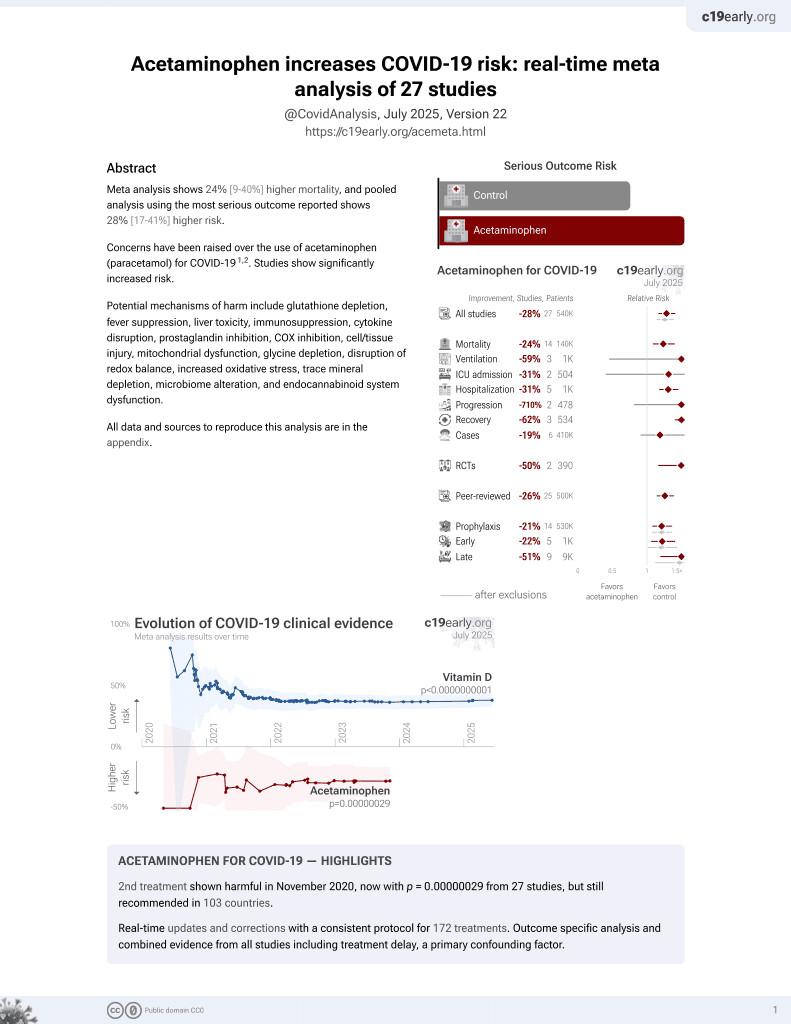
2nd treatment shown to increase risk in
November 2020, now with p = 0.00000029 from 27 studies, but still recommended in 103 countries.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 494 COVID-19 patients showing higher risk of PASC with acetaminophen use in unadjusted results, without reaching statistical significance (p=0.07). Higher risk is also seen for dexamethasone and remdesivir (statistically significant for dexamethasone), however confounding by indication may be significant for these treatments, with increased use for more severe patients. While details of treatment timing and dose are not available, the result for acetaminophen can be compared with ibuprofen, with comparable indication for use. Notably there is no increased risk with ibuprofen, suggesting higher risk with acetaminophen, consistent with the higher risk seen in meta analysis1.
Acetaminophen is also known as paracetamol, Tylenol, Panadol, Calpol, Tempra, Calprofen, Doliprane, Efferalgan, Grippostad C, Dolo, Acamol, Fevadol, Crocin, and Perfalgan.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments2.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of long COVID, 32.1% higher, RR 1.32, p = 0.07, treatment 98 of 232 (42.2%), control 39 of 122 (32.0%).
|
|
risk of long COVID, 0.9% higher, RR 1.01, p = 1.00, treatment 16 of 41 (39.0%), control 121 of 313 (38.7%), ibuprofen.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Chen et al., 16 Oct 2023, prospective, USA, peer-reviewed, 17 authors, study period May 2020 - June 2021.
Contact: jakris@uic.edu, charliekim@verily.com.
Distinct temporal trajectories and risk factors for Post-acute sequelae of SARS-CoV-2 infection
Frontiers in Medicine, doi:10.3389/fmed.2023.1227883
Background: The understanding of Post-acute sequelae of SARS-CoV-2 infection (PASC) can be improved by longitudinal assessment of symptoms encompassing the acute illness period. To gain insight into the various disease trajectories of PASC, we assessed symptom evolution and clinical factors associated with the development of PASC over 3 months, starting with the acute illness period.
Methods: We conducted a prospective cohort study to identify parameters associated with PASC. We performed cluster and case control analyses of clinical data, including symptomatology collected over 3 months following infection. Results: We identified three phenotypic clusters associated with PASC that could be characterized as remittent, persistent, or incident based on the 3-month change in symptom number compared to study entry: remittent (median; min, max: -4; -17, 3), persistent (-2; -14, 7), or incident (4.5; -5, 17) (p = 0.041 remittent vs. persistent, p < 0.001 remittent vs. incident, p < 0.001 persistent vs. incident). Despite younger age and lower hospitalization rates, the incident phenotype had a greater number of symptoms (15; 8, 24) and a higher proportion of participants with PASC (63.2%) than the persistent (6; 2, 9 and 52.2%) or remittent clusters (1; 0, 6 and 18.7%). Systemic corticosteroid administration during acute infection was also associated with PASC at 3 months [OR (95% CI): 2.23 (1.14, 4.36)].
Conclusion: An incident disease phenotype characterized by symptoms that were absent during acute illness and the observed association with high dose steroids during acute illness have potential critical implications for preventing PASC.
Ethics statement The studies involving humans were approved by the Study Protocol # 20201016 WCG Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions HZ, WC, and CK conceptualized the study. CC, KD, HZ, WC, VR, MB, and JK were involved in the study design. SP, VT, JM, CRd, IR, MB, MS, and JK recruited patients and collected the samples. CC, SP, JL, MW, and MS analyzed the data. CC, SP, JL, MW, MS, JK, and CK wrote the manuscript. CC, SP, JL, MW, KD, VR, HZ, WC, VT, JM, CRd, IR, BP, MB, MS, JK, and CK reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest CC, JL, MW, KD, and CK maintain equity ownership and employment at Verily Life Sciences. SP reports personal fees from Jazz Pharmaceuticals, Inc., and UpToDate, Inc., and grants from Philips, Inc., Sommetrics, Inc., and Regeneron. CRd serves on advisory boards for Abbott Diagnostics, Ortho/Quidel Diagnostics, and Roche Diagnostics. JK receives research funding from Regeneron. JK has also provided consulting for GlaxoSmithKline, AstraZeneca, CereVu Medical, Propeller/ResMed, and BData, Inc. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The..
References
Ballering, Van Zon, Hartman, Rosmalen, Lifelines Corona Research Initiative. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study, Lancet, doi:10.1016/S0140-6736(22)01214-4
Beigel, Tomashek, Dodd, Mehta, Zingman et al., Remdesivir for the treatment of Covid-19 -Final report, N Engl J Med
Bowe, Xie, Al-Aly, Postacute sequelae of COVID-19 at 2 years, Nat Med, doi:10.1038/s41591-023-02521-2
Bull-Otterson, Post-COVID conditions among adult COVID-19 survivors aged 18-64 and ≥65 Years-United States, March 2020, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7121e1
Chen, Haupert, Zimmermann, Shi, Fritsche et al., Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review, J Infect Dis
Covid, None
De Melo, Lazarini, Levallois, Hautefort, Michel et al., COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters, Sci Transl Med, doi:10.1126/scitranslmed.abf8396
Frontera, Simon, Bridging knowledge gaps in the diagnosis and management of neuropsychiatric sequelae of COVID-19, JAMA Psychiatry, doi:10.1001/jamapsychiatry.2022.1616
Frontera, Thorpe, Simon, De Havenon, Yaghi et al., Post-acute sequelae of COVID-19 symptom phenotypes and therapeutic strategies: a prospective, observational study, PLoS One, doi:10.1371/journal.pone.0275274
Gottlieb, Wang, Yu, Spatz, Montoy et al., Severe fatigue and persistent symptoms at three months following SARS-CoV-2 infections during the pre-delta, delta, and omicron time periods: a multicenter prospective cohort study, Clin Infect Dis, doi:10.1093/cid/ciad045
Groff, Sun, Ssentongo, Ba, Parsons et al., Shortterm and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.28568
Han, Zheng, Daines, Sheikh, Long-term sequelae of COVID-19: a systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms, Pathogens, doi:10.3390/pathogens11020269
Hulter, Licht, Bonner, Glynn, Sebastian, Effects of glucocorticoid steroids on renal and systemic acid-base metabolism, Am J Physiol
James, Georgopoulos, At the root of 3 "Long" diseases: persistent antigens inflicting chronic damage on the brain and other organs in gulf war illness, Long-COVID-19, and chronic fatigue syndrome, Neurosci Insights, doi:10.1177/26331055221114817
Kenny, Mccann, 'brien, Savinelli, Tinago et al., Identification of distinct long COVID clinical phenotypes through cluster analysis of self-reported symptoms, Open Forum Infect Dis, doi:10.1093/ofid/ofac060
Klein, Wood, Jaycox, Lu, Dhodapkar et al., Distinguishing features of Long COVID identified through immune profiling, medRxiv, doi:10.1101/2022.08.09.22278592
Merad, Blish, Sallusto, Iwasaki, The immunology and immunopathology of COVID-19, Science
Nalbandian, Sehgal, Gupta, Madhavan, Mcgroder et al., Post-acute COVID-19 syndrome, Nat Med
Nasserie, Hittle, Goodman, Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review, JAMA Netw Open
Peluso, Deeks, Early clues regarding the pathogenesis of long-COVID, Trends Immunol
Peluso, Deitchman, Torres, Iyer, Munter et al., Long-term SARS-CoV-2-specific immune and inflammatory responses in individuals recovering from COVID-19 with and without post-acute symptoms, Cell Rep
Recovery, Group, Horby, Lim, Emberson et al., Dexamethasone in hospitalized patients with Covid-19, N Engl J Med
Rensen, Gemke, Van Dalen, Rotteveel, Kaspers, Hypothalamicpituitary-adrenal (HPA) axis suppression after treatment with glucocorticoid therapy for childhood acute lymphoblastic leukaemia, Cochrane Database Syst Rev
Su, Yuan, Chen, Ng, Wang et al., Multiple early factors anticipate post-acute COVID-19 sequelae, Cell
Sudre, Lee, Lochlainn, Varsavsky, Murray et al., Symptom clusters in COVID-19: a potential clinical prediction tool from the COVID symptom study app, Sci Adv, doi:10.1126/sciadv.abd4177
Søvik, Barrat-Due, Kåsine, Olasveengen, Strand et al., Corticosteroids and superinfections in COVID-19 patients on invasive mechanical ventilation, J Infect
Xie, Bowe, Al-Aly, Burdens of post-acute sequelae of COVID-19 by severity of acute infection, demographics and health status, Nat Commun
Zhang, Zang, Xu, Zhang, Xu et al., Data-driven identification of post-acute SARS-CoV-2 infection subphenotypes, Nat Med, doi:10.1038/s41591-022-02116-3
DOI record:
{
"DOI": "10.3389/fmed.2023.1227883",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2023.1227883",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>The understanding of Post-acute sequelae of SARS-CoV-2 infection (PASC) can be improved by longitudinal assessment of symptoms encompassing the acute illness period. To gain insight into the various disease trajectories of PASC, we assessed symptom evolution and clinical factors associated with the development of PASC over 3 months, starting with the acute illness period.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We conducted a prospective cohort study to identify parameters associated with PASC. We performed cluster and case control analyses of clinical data, including symptomatology collected over 3 months following infection.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>We identified three phenotypic clusters associated with PASC that could be characterized as remittent, persistent, or incident based on the 3-month change in symptom number compared to study entry: remittent (median; min, max: −4; −17, 3), persistent (−2; −14, 7), or incident (4.5; −5, 17) (<jats:italic>p</jats:italic> = 0.041 remittent vs. persistent, <jats:italic>p</jats:italic> &lt; 0.001 remittent vs. incident, <jats:italic>p</jats:italic> &lt; 0.001 persistent vs. incident). Despite younger age and lower hospitalization rates, the incident phenotype had a greater number of symptoms (15; 8, 24) and a higher proportion of participants with PASC (63.2%) than the persistent (6; 2, 9 and 52.2%) or remittent clusters (1; 0, 6 and 18.7%). Systemic corticosteroid administration during acute infection was also associated with PASC at 3 months [OR (95% CI): 2.23 (1.14, 4.36)].</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>An incident disease phenotype characterized by symptoms that were absent during acute illness and the observed association with high dose steroids during acute illness have potential critical implications for preventing PASC.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fmed.2023.1227883"
],
"author": [
{
"affiliation": [],
"family": "Chen",
"given": "Chen",
"sequence": "first"
},
{
"affiliation": [],
"family": "Parthasarathy",
"given": "Sairam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leung",
"given": "Jacqueline M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wu",
"given": "Michelle J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Drake",
"given": "Katherine A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ridaura",
"given": "Vanessa K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zisser",
"given": "Howard C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Conrad",
"given": "William A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tapson",
"given": "Victor F.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moy",
"given": "James N.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "deFilippi",
"given": "Christopher R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rosas",
"given": "Ivan O.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prabhakar",
"given": "Bellur S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Basit",
"given": "Mujeeb",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Salvatore",
"given": "Mirella",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Krishnan",
"given": "Jerry A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kim",
"given": "Charles C.",
"sequence": "additional"
}
],
"container-title": "Frontiers in Medicine",
"container-title-short": "Front. Med.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
10,
16
]
],
"date-time": "2023-10-16T15:18:54Z",
"timestamp": 1697469534000
},
"deposited": {
"date-parts": [
[
2023,
10,
16
]
],
"date-time": "2023-10-16T15:19:03Z",
"timestamp": 1697469543000
},
"indexed": {
"date-parts": [
[
2023,
10,
29
]
],
"date-time": "2023-10-29T05:12:56Z",
"timestamp": 1698556376680
},
"is-referenced-by-count": 1,
"issued": {
"date-parts": [
[
2023,
10,
16
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
10,
16
]
],
"date-time": "2023-10-16T00:00:00Z",
"timestamp": 1697414400000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2023.1227883/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
10,
16
]
]
},
"published-online": {
"date-parts": [
[
2023,
10,
16
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.15585/mmwr.mm7121e1",
"article-title": "Post–COVID conditions among adult COVID-19 survivors aged 18–64 and ≥65 Years–United States, March 2020–November 2021.",
"author": "Bull-Otterson",
"doi-asserted-by": "publisher",
"first-page": "713",
"journal-title": "MMWR Morb Mortal Wkly Rep.",
"key": "B1",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1038/s41467-021-26513-3",
"article-title": "Burdens of post-acute sequelae of COVID-19 by severity of acute infection, demographics and health status.",
"author": "Xie",
"doi-asserted-by": "crossref",
"journal-title": "Nat Commun.",
"key": "B2",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1126/science.abm8108",
"article-title": "The immunology and immunopathology of COVID-19.",
"author": "Merad",
"doi-asserted-by": "crossref",
"first-page": "1122",
"journal-title": "Science.",
"key": "B3",
"volume": "375",
"year": "2022"
},
{
"DOI": "10.1016/j.it.2022.02.008",
"article-title": "Early clues regarding the pathogenesis of long-COVID.",
"author": "Peluso",
"doi-asserted-by": "crossref",
"first-page": "268",
"journal-title": "Trends Immunol.",
"key": "B4",
"volume": "43",
"year": "2022"
},
{
"journal-title": "Department of Health and Human Services, Office of the Assistant Secretary for Health. National Research Action Plan on Long COVID.",
"key": "B5",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(22)01214-4",
"article-title": "Lifelines Corona Research Initiative. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study.",
"author": "Ballering",
"doi-asserted-by": "publisher",
"first-page": "452",
"journal-title": "Lancet.",
"key": "B6",
"volume": "400",
"year": "2022"
},
{
"DOI": "10.1038/s41591-023-02521-2",
"article-title": "Postacute sequelae of COVID-19 at 2 years.",
"author": "Bowe",
"doi-asserted-by": "publisher",
"first-page": "2347",
"journal-title": "Nat Med.",
"key": "B7",
"volume": "29",
"year": "2023"
},
{
"journal-title": "WHO R&D Blueprint novel Coronavirus COVID-19 Therapeutic Trial Synopsis.",
"key": "B8",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2021436",
"article-title": "Dexamethasone in hospitalized patients with Covid-19.",
"author": "Horby",
"doi-asserted-by": "crossref",
"first-page": "693",
"journal-title": "N Engl J Med.",
"key": "B9",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2007764",
"article-title": "Remdesivir for the treatment of Covid-19 - Final report.",
"author": "Beigel",
"doi-asserted-by": "crossref",
"first-page": "1813",
"journal-title": "N Engl J Med.",
"key": "B10",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1126/scitranslmed.abf8396",
"article-title": "COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters.",
"author": "de Melo",
"doi-asserted-by": "publisher",
"journal-title": "Sci Transl Med.",
"key": "B11",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1177/26331055221114817",
"article-title": "At the root of 3 “Long” diseases: persistent antigens inflicting chronic damage on the brain and other organs in gulf war illness, Long-COVID-19, and chronic fatigue syndrome.",
"author": "James",
"doi-asserted-by": "publisher",
"journal-title": "Neurosci Insights.",
"key": "B12",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1126/sciadv.abd4177",
"article-title": "Symptom clusters in COVID-19: a potential clinical prediction tool from the COVID symptom study app.",
"author": "Sudre",
"doi-asserted-by": "publisher",
"journal-title": "Sci Adv.",
"key": "B13",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1093/ofid/ofac060",
"article-title": "Identification of distinct long COVID clinical phenotypes through cluster analysis of self-reported symptoms.",
"author": "Kenny",
"doi-asserted-by": "publisher",
"journal-title": "Open Forum Infect Dis.",
"key": "B14",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0275274",
"article-title": "Post-acute sequelae of COVID-19 symptom phenotypes and therapeutic strategies: a prospective, observational study.",
"author": "Frontera",
"doi-asserted-by": "publisher",
"journal-title": "PLoS One.",
"key": "B15",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1038/s41591-021-01283-z",
"article-title": "Post-acute COVID-19 syndrome.",
"author": "Nalbandian",
"doi-asserted-by": "crossref",
"first-page": "601",
"journal-title": "Nat Med.",
"key": "B16",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1038/s41591-022-02116-3",
"article-title": "Data-driven identification of post-acute SARS-CoV-2 infection subphenotypes.",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "226",
"journal-title": "Nat Med.",
"key": "B17",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.1016/j.cell.2022.01.014",
"article-title": "Multiple early factors anticipate post-acute COVID-19 sequelae.",
"author": "Su",
"doi-asserted-by": "crossref",
"first-page": "881",
"journal-title": "Cell.",
"key": "B18",
"volume": "185",
"year": "2022"
},
{
"DOI": "10.1093/cid/ciad045",
"article-title": "Severe fatigue and persistent symptoms at three months following SARS-CoV-2 infections during the pre-delta, delta, and omicron time periods: a multicenter prospective cohort study.",
"author": "Gottlieb",
"doi-asserted-by": "publisher",
"first-page": "1930",
"journal-title": "Clin Infect Dis.",
"key": "B19",
"volume": "76",
"year": "2023"
},
{
"DOI": "10.1093/infdis/jiac136",
"article-title": "Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review.",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "1593",
"journal-title": "J Infect Dis.",
"key": "B20",
"volume": "226",
"year": "2022"
},
{
"DOI": "10.3390/pathogens11020269",
"article-title": "Long-term sequelae of COVID-19: a systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms.",
"author": "Han",
"doi-asserted-by": "publisher",
"journal-title": "Pathogens.",
"key": "B21",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2021.28568",
"article-title": "Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review.",
"author": "Groff",
"doi-asserted-by": "publisher",
"journal-title": "JAMA Netw Open.",
"key": "B22",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1001/jamapsychiatry.2022.1616",
"article-title": "Bridging knowledge gaps in the diagnosis and management of neuropsychiatric sequelae of COVID-19.",
"author": "Frontera",
"doi-asserted-by": "publisher",
"first-page": "811",
"journal-title": "JAMA Psychiatry.",
"key": "B23",
"volume": "79",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2021.11417",
"article-title": "Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review.",
"author": "Nasserie",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open.",
"key": "B24",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/j.celrep.2021.109518",
"article-title": "Long-term SARS-CoV-2-specific immune and inflammatory responses in individuals recovering from COVID-19 with and without post-acute symptoms.",
"author": "Peluso",
"doi-asserted-by": "crossref",
"journal-title": "Cell Rep.",
"key": "B25",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1016/j.jinf.2022.05.015",
"article-title": "Corticosteroids and superinfections in COVID-19 patients on invasive mechanical ventilation.",
"author": "Søvik",
"doi-asserted-by": "crossref",
"first-page": "57",
"journal-title": "J Infect.",
"key": "B26",
"volume": "85",
"year": "2022"
},
{
"article-title": "Effects of glucocorticoid steroids on renal and systemic acid-base metabolism.",
"author": "Hulter",
"first-page": "F30",
"journal-title": "Am J Physiol.",
"key": "B27",
"volume": "239",
"year": "1980"
},
{
"DOI": "10.1101/2022.08.09.22278592",
"article-title": "Distinguishing features of Long COVID identified through immune profiling.",
"author": "Klein",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "B28",
"year": "2022"
},
{
"article-title": "Hypothalamic-pituitary-adrenal (HPA) axis suppression after treatment with glucocorticoid therapy for childhood acute lymphoblastic leukaemia.",
"author": "Rensen",
"journal-title": "Cochrane Database Syst Rev.",
"key": "B29",
"volume": "11",
"year": "2017"
}
],
"reference-count": 29,
"references-count": 29,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2023.1227883/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Distinct temporal trajectories and risk factors for Post-acute sequelae of SARS-CoV-2 infection",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "10"
}