Correlation between 25-hydroxyvitamin D/D3 Deficiency and COVID-19 Disease Severity in Adults from Northern Colorado
et al., Nutrients, doi:10.3390/nu14245204, NCT04603677, Dec 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of 131 COVID+ patients and 18 healthy controls, showing COVID-19 severity associated with lower vitamin D levels.
Baxter et al., 7 Dec 2022, USA, peer-reviewed, mean age 57.0, 14 authors, study period July 2020 - March 2021, trial NCT04603677 (history).
Contact: e.p.ryan@colostate.edu (corresponding author).
Correlation between 25-hydroxyvitamin D/D3 Deficiency and COVID-19 Disease Severity in Adults from Northern Colorado
Nutrients, doi:10.3390/nu14245204
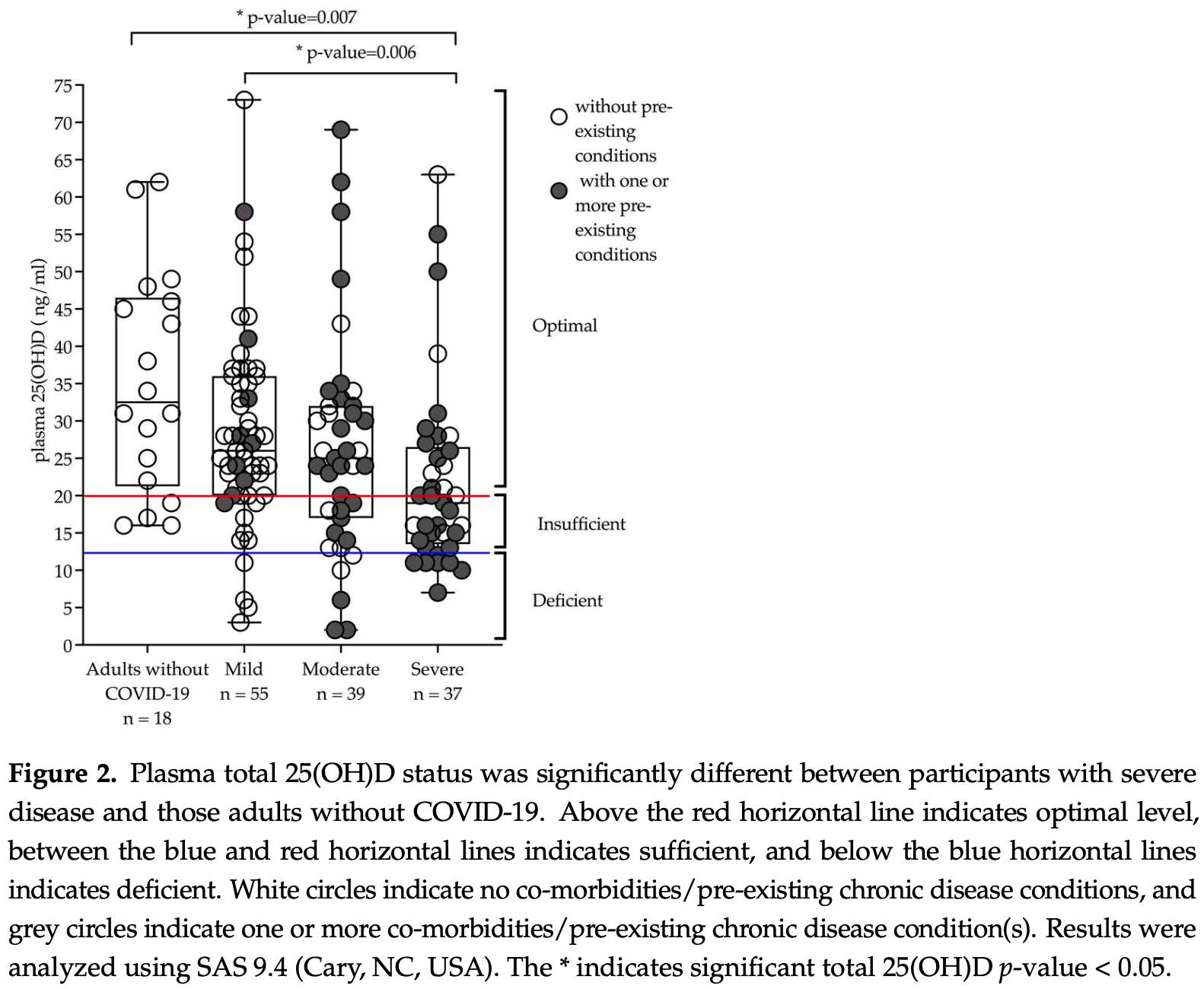
Vitamin D deficiency is common in the United States and leads to altered immune function, including T cell and macrophage activity that may impact responses to SARS-CoV-2 infection. This study investigated 131 adults with a history of a positive SARS-CoV-2 nasopharyngeal PCR and 18 adults with no COVID-19 diagnosis that were recruited from the community or hospital into the Northern Colorado Coronavirus Biorepository (NoCo-COBIO). Participants consented to enrollment for a period of 6 months and provided biospecimens at multiple visits for longitudinal analysis. Plasma 25-hydroxyvitamin D levels were quantified by LC-MS/MS at the initial visit (n = 149) and after 4 months (n = 89). Adults were classified as deficient (<30 nM or <12 ng/mL), insufficient (<30-50 nM or 12-20 ng/mL), or optimal (50-75 nM or >20 ng/mL) for 25-hydroxyvitamin D status. Fisher's exact test demonstrated an association between disease severity, gender, and body mass index (BMI) at baseline. Mixed model analyses with Tukey-Kramer were used for longitudinal analysis according to BMI. Sixty-nine percent (n = 103) of the entire cohort had optimal levels of total 25(OH)D, 22% (n = 32) had insufficient levels, and 9% (n = 14) had deficent levels. Participants with severe disease (n = 37) had significantly lower 25-hydroxyvitamin D (total 25(OH)D) when compared to adults with mild disease (p = 0.006) or no COVID-19 diagnosis (p = 0.007). There was 44% of the cohort with post-acute sequalae of COVID-19 (PASC) as defined by experiencing at least one of the following symptoms after 60 days' post-infection: fatigue, dyspnea, joint pain, chest pain, forgetfulness or absent-mindedness, confusion, or difficulty breathing. While significant differences were detected in 25-hydroxyvitamin D status by sex and BMI, there were no correlations between 25-hydroxyvitamin D for those without and without PASC. This longitudinal study of COVID-19 survivors demonstrates an important association between sex, BMI, and disease severity for 25-hydroxyvitamin D deficiency during acute stages of infection, yet it is not clear whether supplementation efforts would influence long term outcomes such as developing PASC.
Conflicts of Interest: The authors declare no conflict of interest.
References
Aloia, Patel, Dimaano, Li-Ng, Talwar et al., Vitamin D intake to attain a desired serum 25-hydroxyvitamin D concentration, Am. J. Clin. Nutr, doi:10.1093/ajcn/87.6.1952
Alquaiz, Kazi, Fouda, Alyousefi, Age and gender differences in the prevalence and correlates of vitamin D deficiency, Arch. Osteoporos, doi:10.1007/s11657-018-0461-5
Armas, Heaney, Vitamin, The Iceberg Nutrient, J. Ren. Nutr, doi:10.1053/j.jrn.2010.09.002
Baz-Hecht, Goldfine, The impact of vitamin D deficiency on diabetes and cardiovascular risk, Curr. Opin. Endocrinol. Diabetes Obes, doi:10.1097/MED.0b013e3283372859
Berridge, Vitamin D deficiency and diabetes, Biochem. J, doi:10.1042/BCJ20170042
Biesalski, Vitamin D deficiency and co-morbidities in COVID-19 patients-A fatal relationship?, Nfs J
Bishop, Ismailova, Dimeloe, Hewison, White, Vitamin D and Immune Regulation: Antibacterial, Antiviral, Anti-Inflammatory, JBMR Plus, doi:10.1002/jbm4.10405
Braun, Gibbons, Litonjua, Giovannucci, Christopher, Low serum 25-hydroxyvitamin D at critical care initiation is associated with increased mortality, Crit. Care Med, doi:10.1097/CCM.0b013e31822d74f3
Chen, Zhang, Ge, Du, Deb et al., Vitamin D receptor inhibits nuclear factor κB activation by interacting with IκB kinase β protein, J. Biol. Chem, doi:10.1074/jbc.M113.467670
Connors, Sheikholislam, Irias, Vitamin D toxicity after dieting in hypoparathyroidism, Pediatrics
Edward, Macdonald, Zeisel, Present Knowledge in Nutrition
Forrest, Stuhldreher, Prevalence and correlates of vitamin D deficiency in US adults, Nutr. Res
Hars, Mendes, Serratrice, Herrmann, Gold et al., Sex-specific association between vitamin D deficiency and COVID-19 mortality in older patients, Osteoporos. Int, doi:10.1007/s00198-020-05677-6
Hayashi, Okamatsu, Ogasawara, Tsugawa, Isoda et al., Oral Supplementation of the Vitamin D Metabolite 25(OH)D3 Against Influenza Virus Infection in Mice, Nutrients, doi:10.3390/nu12072000
Judd, Tangpricha, Vitamin D Deficiency and Risk for Cardiovascular Disease, Am. J. Med. Sci, doi:10.1097/MAJ.0b013e3181aaee91
Khan, Ullah, Randhawa, Iqtadar, Butt et al., Role of Vitamin D in reducing number of acute exacerbations in Chronic Obstructive Pulmonary Disease (COPD) patients, Pak. J. Med. Sci, doi:10.12669/pjms.333.12397
Laires, Nunes, Population-based Estimates for High Risk of Severe COVID-19 Disease due to Age and Underlying Health Conditions, Acta Med. Port, doi:10.20344/amp.14222
Latic, Erben, Vitamin, Cardiovascular Disease, with Emphasis on Hypertension, Atherosclerosis, and Heart Failure, Int. J. Mol. Sci, doi:10.3390/ijms21186483
Lavergne, Stromberg, Baxter, Webb, Dutt et al., A longitudinal SARS-CoV-2 biorepository for COVID-19 survivors with and without post-acute sequelae, BMC Infect. Dis, doi:10.1186/s12879-021-06359-2
Lima, Rocha, Moreira, Genetic and epigenetic control of ACE2 expression and its possible role in COVID-19, Cell Biochem. Funct, doi:10.1002/cbf.3648
Lips, Cashman, Lamberg-Allardt, Bischoff-Ferrari, Obermayer-Pietsch et al., Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: A position statement of the European Calcified Tissue Society, Eur. J. Endocrinol, doi:10.1530/EJE-18-0736
Looker, Schleicher, Vitamin, Status: United States, 2001-2006, NCHS Data Brief
Lucas, Wong, Klein, Castro, Silva et al., Longitudinal analyses reveal immunological misfiring in severe COVID-19, Nature, doi:10.1038/s41586-020-2588-y
Mcfann, Baxter, Lavergne, Stromberg, Berry et al., Quality of Life (QoL) Is Reduced in Those with Severe COVID-19 Disease, Post-Acute Sequelae of COVID-19, and Hospitalization in United States Adults from Northern Colorado, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph182111048
Mcmullan, Borgi, Curhan, Fisher, Forman, The effect of vitamin D on renin-angiotensin system activation and blood pressure: A randomized control trial, J. Hypertens, doi:10.1097/HJH.0000000000001220
Molloy, Murphy, Vitamin, COVID-19 and Children, Ir. Med. J
Murdoch, Slow, Chambers, Jennings, Stewart et al., Effect of vitamin D3 supplementation on upper respiratory tract infections in healthy adults: The VIDARIS randomized controlled trial, JAMA, doi:10.1001/jama.2012.12505
Oristrell, Oliva, Casado, Subirana, Domínguez et al., Vitamin D supplementation and COVID-19 risk: A population-based, cohort study, J. Endocrinol. Investig, doi:10.1007/s40618-021-01639-9
Park, Pichiah, Cha, Vitamin, Metabolic Diseases: Growing Roles of Vitamin D, J. Obes. Metab. Syndr, doi:10.7570/jomes.2018.27.4.223
Perticone, Maio, Sciacqua, Suraci, Pinto et al., Ketogenic Diet-Induced Weight Loss is Associated with an Increase in Vitamin D Levels in Obese Adults, Molecules
Pike, Christakos, Biology and Mechanisms of Action of the Vitamin D Hormone, Endocrinol. Metab. Clin. N. Am, doi:10.1016/j.ecl.2017.07.001
Prietl, Treiber, Pieber, Amrein, Vitamin D and immune function, Nutrients, doi:10.3390/nu5072502
Quraishi, Camargo, Vitamin D in acute stress and critical illness, Curr. Opin. Clin. Nutr. Metab. Care
Rybchyn, Abboud, Puglisi, Gordon-Thomson, Brennan-Speranza et al., Skeletal Muscle and the Maintenance of Vitamin D Status, Nutrients, doi:10.3390/nu12113270
Sabetta, Depetrillo, Cipriani, Smardin, Burns et al., Serum 25-hydroxyvitamin d and the incidence of acute viral respiratory tract infections in healthy adults, PLoS ONE, doi:10.1371/journal.pone.0011088
Sanghera, Sapkota, Aston, Blackett, Vitamin et al., Gender Differences and Cardiometabolic Health Disparities, Ann. Nutr. Metab, doi:10.1159/000458765
Scherer, Kirwan, Rosen, Post-acute sequelae of COVID-19: A metabolic perspective, eLife, doi:10.7554/eLife.78200
Shirvaliloo, Epigenomics in COVID-19; the link between DNA methylation, histone modifications and SARS-CoV-2 infection, Epigenomics, doi:10.2217/epi-2021-0057
Thacher, Evaluating the Evidence in Clinical Studies of Vitamin D in COVID-19, Nutrients, doi:10.3390/nu14030464
Wang, Chen, Li, Yin, Zhang et al., Vitamin D and Chronic Diseases, Aging Dis
Wortsman, Matsuoka, Chen, Lu, Holick, Decreased bioavailability of vitamin D in obesity, Am. J. Clin. Nutr, doi:10.1093/ajcn/72.3.690
Zdrenghea, Makrinioti, Bagacean, Bush, Johnston et al., Vitamin D modulation of innate immune responses to respiratory viral infections, Rev. Med. Virol, doi:10.1002/rmv.1909
Ziaie, Razmjou, Jomhouri, Jenabi, Vitamin D Toxicity; Stored and Released from Adipose Tissue?, Arch. Iran. Med
DOI record:
{
"DOI": "10.3390/nu14245204",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu14245204",
"abstract": "<jats:p>Vitamin D deficiency is common in the United States and leads to altered immune function, including T cell and macrophage activity that may impact responses to SARS-CoV-2 infection. This study investigated 131 adults with a history of a positive SARS-CoV-2 nasopharyngeal PCR and 18 adults with no COVID-19 diagnosis that were recruited from the community or hospital into the Northern Colorado Coronavirus Biorepository (NoCo-COBIO). Participants consented to enrollment for a period of 6 months and provided biospecimens at multiple visits for longitudinal analysis. Plasma 25-hydroxyvitamin D levels were quantified by LC-MS/MS at the initial visit (n = 149) and after 4 months (n = 89). Adults were classified as deficient (<30 nM or <12 ng/mL), insufficient (<30–50 nM or 12–20 ng/mL), or optimal (50–75 nM or >20 ng/mL) for 25-hydroxyvitamin D status. Fisher’s exact test demonstrated an association between disease severity, gender, and body mass index (BMI) at baseline. Mixed model analyses with Tukey-Kramer were used for longitudinal analysis according to BMI. Sixty-nine percent (n = 103) of the entire cohort had optimal levels of total 25(OH)D, 22% (n = 32) had insufficient levels, and 9% (n = 14) had deficent levels. Participants with severe disease (n = 37) had significantly lower 25-hydroxyvitamin D (total 25(OH)D) when compared to adults with mild disease (p = 0.006) or no COVID-19 diagnosis (p = 0.007). There was 44% of the cohort with post-acute sequalae of COVID-19 (PASC) as defined by experiencing at least one of the following symptoms after 60 days’ post-infection: fatigue, dyspnea, joint pain, chest pain, forgetfulness or absent-mindedness, confusion, or difficulty breathing. While significant differences were detected in 25-hydroxyvitamin D status by sex and BMI, there were no correlations between 25-hydroxyvitamin D for those without and without PASC. This longitudinal study of COVID-19 survivors demonstrates an important association between sex, BMI, and disease severity for 25-hydroxyvitamin D deficiency during acute stages of infection, yet it is not clear whether supplementation efforts would influence long term outcomes such as developing PASC.</jats:p>",
"alternative-id": [
"nu14245204"
],
"author": [
{
"affiliation": [],
"family": "Baxter",
"given": "Bridget A.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ryan",
"given": "Michaela G.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "LaVergne",
"given": "Stephanie M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stromberg",
"given": "Sophia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Berry",
"given": "Kailey",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tipton",
"given": "Madison",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Natter",
"given": "Nicole",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2414-2025",
"affiliation": [],
"authenticated-orcid": false,
"family": "Nudell",
"given": "Nikiah",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9348-9954",
"affiliation": [],
"authenticated-orcid": false,
"family": "McFann",
"given": "Kim",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dunn",
"given": "Julie",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4547-3787",
"affiliation": [],
"authenticated-orcid": false,
"family": "Webb",
"given": "Tracy L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Armstrong",
"given": "Michael",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0425-8012",
"affiliation": [],
"authenticated-orcid": false,
"family": "Reisdorph",
"given": "Nichole",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1577-0919",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ryan",
"given": "Elizabeth P.",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
12,
7
]
],
"date-time": "2022-12-07T09:00:37Z",
"timestamp": 1670403637000
},
"deposited": {
"date-parts": [
[
2022,
12,
7
]
],
"date-time": "2022-12-07T10:03:47Z",
"timestamp": 1670407427000
},
"funder": [
{
"name": "translational research infrastructure in the Colorado State University department of Environmental and Radiological Health Sciences"
},
{
"name": "CSU Vice President for the Research Office to Elizabeth P. Ryan"
},
{
"award": [
"1S10OD010366-01A1"
],
"name": "UCHealth North Foundation Funds to Julie Dunn"
}
],
"indexed": {
"date-parts": [
[
2022,
12,
7
]
],
"date-time": "2022-12-07T10:42:20Z",
"timestamp": 1670409740988
},
"is-referenced-by-count": 0,
"issue": "24",
"issued": {
"date-parts": [
[
2022,
12,
7
]
]
},
"journal-issue": {
"issue": "24",
"published-online": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
12,
7
]
],
"date-time": "2022-12-07T00:00:00Z",
"timestamp": 1670371200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/14/24/5204/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "5204",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
12,
7
]
]
},
"published-online": {
"date-parts": [
[
2022,
12,
7
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "Ross, A.C., Taylor, C.L., Yaktine, A.L., and Del Valle, H.B. (2022, June 23). Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium, Dietary Reference Intakes for Calcium and Vitamin D, Available online: http://www.ncbi.nlm.nih.gov/books/NBK56070/."
},
{
"key": "ref_2",
"unstructured": "Edward, J., Macdonald, I., and Zeisel, S. (2012). Present Knowledge in Nutrition, Wiley. [10th ed.]."
},
{
"DOI": "10.3390/nu5072502",
"article-title": "Vitamin D and immune function",
"author": "Prietl",
"doi-asserted-by": "crossref",
"first-page": "2502",
"journal-title": "Nutrients",
"key": "ref_3",
"volume": "5",
"year": "2013"
},
{
"DOI": "10.7570/jomes.2018.27.4.223",
"article-title": "Vitamin D and Metabolic Diseases: Growing Roles of Vitamin D",
"author": "Park",
"doi-asserted-by": "crossref",
"first-page": "223",
"journal-title": "J. Obes. Metab. Syndr.",
"key": "ref_4",
"volume": "27",
"year": "2018"
},
{
"DOI": "10.1002/jbm4.10405",
"article-title": "Vitamin D and Immune Regulation: Antibacterial, Antiviral, Anti-Inflammatory",
"author": "Bishop",
"doi-asserted-by": "crossref",
"first-page": "e10405",
"journal-title": "JBMR Plus",
"key": "ref_5",
"volume": "5",
"year": "2021"
},
{
"article-title": "Vitamin D Status: United States, 2001–2006",
"author": "Looker",
"first-page": "1",
"journal-title": "NCHS Data Brief",
"key": "ref_6",
"volume": "59",
"year": "2011"
},
{
"DOI": "10.1530/EJE-18-0736",
"article-title": "Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: A position statement of the European Calcified Tissue Society",
"author": "Lips",
"doi-asserted-by": "crossref",
"first-page": "P23",
"journal-title": "Eur. J. Endocrinol.",
"key": "ref_7",
"volume": "180",
"year": "2019"
},
{
"DOI": "10.1002/rmv.1909",
"article-title": "Vitamin D modulation of innate immune responses to respiratory viral infections",
"author": "Zdrenghea",
"doi-asserted-by": "crossref",
"first-page": "e1909",
"journal-title": "Rev. Med. Virol.",
"key": "ref_8",
"volume": "27",
"year": "2017"
},
{
"DOI": "10.1074/jbc.M113.467670",
"article-title": "Vitamin D receptor inhibits nuclear factor κB activation by interacting with IκB kinase β protein",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "19450",
"journal-title": "J. Biol. Chem.",
"key": "ref_9",
"volume": "288",
"year": "2013"
},
{
"DOI": "10.1093/ajcn/72.3.690",
"article-title": "Decreased bioavailability of vitamin D in obesity",
"author": "Wortsman",
"doi-asserted-by": "crossref",
"first-page": "690",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_10",
"volume": "72",
"year": "2000"
},
{
"DOI": "10.20944/preprints202008.0685.v1",
"doi-asserted-by": "crossref",
"key": "ref_11",
"unstructured": "Rybchyn, M.S., Abboud, M., Puglisi, D.A., Gordon-Thomson, C., Brennan-Speranza, T.C., Mason, R.S., and Fraser, D.R. (2020). Skeletal Muscle and the Maintenance of Vitamin D Status. Nutrients, 12."
},
{
"DOI": "10.7554/eLife.78200",
"article-title": "Post-acute sequelae of COVID-19: A metabolic perspective",
"author": "Scherer",
"doi-asserted-by": "crossref",
"first-page": "e78200",
"journal-title": "eLife",
"key": "ref_12",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1007/s00198-020-05677-6",
"article-title": "Sex-specific association between vitamin D deficiency and COVID-19 mortality in older patients",
"author": "Hars",
"doi-asserted-by": "crossref",
"first-page": "2495",
"journal-title": "Osteoporos. Int.",
"key": "ref_13",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.20344/amp.14222",
"article-title": "Population-based Estimates for High Risk of Severe COVID-19 Disease due to Age and Underlying Health Conditions",
"author": "Laires",
"doi-asserted-by": "crossref",
"first-page": "720",
"journal-title": "Acta Med. Port.",
"key": "ref_14",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1186/s12879-021-06359-2",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "LaVergne, S.M., Stromberg, S., Baxter, B.A., Webb, T.L., Dutt, T.S., Berry, K., Tipton, M., Haberman, J., Massey, B.R., and McFann, K. (2021). A longitudinal SARS-CoV-2 biorepository for COVID-19 survivors with and without post-acute sequelae. BMC Infect. Dis., 21."
},
{
"DOI": "10.1038/s41586-020-2588-y",
"article-title": "Longitudinal analyses reveal immunological misfiring in severe COVID-19",
"author": "Lucas",
"doi-asserted-by": "crossref",
"first-page": "463",
"journal-title": "Nature",
"key": "ref_16",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.3390/ijerph182111048",
"doi-asserted-by": "crossref",
"key": "ref_17",
"unstructured": "McFann, K., Baxter, B.A., LaVergne, S.M., Stromberg, S., Berry, K., Tipton, M., Haberman, J., Ladd, J., Webb, T.L., and Dunn, J.A. (2021). Quality of Life (QoL) Is Reduced in Those with Severe COVID-19 Disease, Post-Acute Sequelae of COVID-19, and Hospitalization in United States Adults from Northern Colorado. Int. J. Environ. Res. Public Health, 18."
},
{
"key": "ref_18",
"unstructured": "(2022, May 09). A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus. Available online: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1."
},
{
"DOI": "10.1097/MCO.0b013e328358fc2b",
"article-title": "Vitamin D in acute stress and critical illness",
"author": "Quraishi",
"doi-asserted-by": "crossref",
"first-page": "625",
"journal-title": "Curr. Opin. Clin. Nutr. Metab. Care",
"key": "ref_19",
"volume": "15",
"year": "2012"
},
{
"DOI": "10.1001/jama.2012.12505",
"article-title": "Effect of vitamin D3 supplementation on upper respiratory tract infections in healthy adults: The VIDARIS randomized controlled trial",
"author": "Murdoch",
"doi-asserted-by": "crossref",
"first-page": "1333",
"journal-title": "JAMA",
"key": "ref_20",
"volume": "308",
"year": "2012"
},
{
"DOI": "10.1016/j.nutres.2010.12.001",
"article-title": "Prevalence and correlates of vitamin D deficiency in US adults",
"author": "Forrest",
"doi-asserted-by": "crossref",
"first-page": "48",
"journal-title": "Nutr. Res.",
"key": "ref_21",
"volume": "31",
"year": "2011"
},
{
"DOI": "10.1371/journal.pone.0011088",
"doi-asserted-by": "crossref",
"key": "ref_22",
"unstructured": "Sabetta, J.R., DePetrillo, P., Cipriani, R.J., Smardin, J., Burns, L.A., and Landry, M.L. (2010). Serum 25-hydroxyvitamin d and the incidence of acute viral respiratory tract infections in healthy adults. PLoS ONE, 5."
},
{
"DOI": "10.3390/nu12072000",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Hayashi, H., Okamatsu, M., Ogasawara, H., Tsugawa, N., Isoda, N., Matsuno, K., and Sakoda, Y. (2020). Oral Supplementation of the Vitamin D Metabolite 25(OH)D3 Against Influenza Virus Infection in Mice. Nutrients, 12."
},
{
"article-title": "Vitamin D, COVID-19 and Children",
"author": "Molloy",
"first-page": "64",
"journal-title": "Ir. Med. J.",
"key": "ref_24",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.14336/AD.2016.1021",
"article-title": "Vitamin D and Chronic Diseases",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "346",
"journal-title": "Aging Dis.",
"key": "ref_25",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1053/j.jrn.2010.09.002",
"article-title": "Vitamin D: The Iceberg Nutrient",
"author": "Armas",
"doi-asserted-by": "crossref",
"first-page": "134",
"journal-title": "J. Ren. Nutr.",
"key": "ref_26",
"volume": "21",
"year": "2011"
},
{
"DOI": "10.1016/j.ecl.2017.07.001",
"article-title": "Biology and Mechanisms of Action of the Vitamin D Hormone",
"author": "Pike",
"doi-asserted-by": "crossref",
"first-page": "815",
"journal-title": "Endocrinol. Metab. Clin. N. Am.",
"key": "ref_27",
"volume": "46",
"year": "2017"
},
{
"DOI": "10.1097/CCM.0b013e31822d74f3",
"article-title": "Low serum 25-hydroxyvitamin D at critical care initiation is associated with increased mortality",
"author": "Braun",
"doi-asserted-by": "crossref",
"first-page": "63",
"journal-title": "Crit. Care Med.",
"key": "ref_28",
"volume": "40",
"year": "2012"
},
{
"DOI": "10.1016/j.nfs.2020.06.001",
"article-title": "Vitamin D deficiency and co-morbidities in COVID-19 patients—A fatal relationship?",
"author": "Biesalski",
"doi-asserted-by": "crossref",
"first-page": "10",
"journal-title": "Nfs J.",
"key": "ref_29",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1007/s40618-021-01639-9",
"article-title": "Vitamin D supplementation and COVID-19 risk: A population-based, cohort study",
"author": "Oristrell",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "J. Endocrinol. Investig.",
"key": "ref_30",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.1093/ajcn/87.6.1952",
"article-title": "Vitamin D intake to attain a desired serum 25-hydroxyvitamin D concentration",
"author": "Aloia",
"doi-asserted-by": "crossref",
"first-page": "1952",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_31",
"volume": "87",
"year": "2008"
},
{
"DOI": "10.1097/MAJ.0b013e3181aaee91",
"article-title": "Vitamin D Deficiency and Risk for Cardiovascular Disease",
"author": "Judd",
"doi-asserted-by": "crossref",
"first-page": "40",
"journal-title": "Am. J. Med. Sci.",
"key": "ref_32",
"volume": "338",
"year": "2009"
},
{
"DOI": "10.1097/MED.0b013e3283372859",
"article-title": "The impact of vitamin D deficiency on diabetes and cardiovascular risk",
"author": "Goldfine",
"doi-asserted-by": "crossref",
"first-page": "113",
"journal-title": "Curr. Opin. Endocrinol. Diabetes Obes.",
"key": "ref_33",
"volume": "17",
"year": "2010"
},
{
"DOI": "10.3390/ijms21186483",
"doi-asserted-by": "crossref",
"key": "ref_34",
"unstructured": "Latic, N., and Erben, R.G. (2020). Vitamin D and Cardiovascular Disease, with Emphasis on Hypertension, Atherosclerosis, and Heart Failure. Int. J. Mol. Sci., 21."
},
{
"DOI": "10.1097/HJH.0000000000001220",
"article-title": "The effect of vitamin D on renin-angiotensin system activation and blood pressure: A randomized control trial",
"author": "McMullan",
"doi-asserted-by": "crossref",
"first-page": "822",
"journal-title": "J. Hypertens.",
"key": "ref_35",
"volume": "35",
"year": "2017"
},
{
"DOI": "10.12669/pjms.333.12397",
"article-title": "Role of Vitamin D in reducing number of acute exacerbations in Chronic Obstructive Pulmonary Disease (COPD) patients",
"author": "Khan",
"doi-asserted-by": "crossref",
"first-page": "610",
"journal-title": "Pak. J. Med. Sci.",
"key": "ref_36",
"volume": "33",
"year": "2017"
},
{
"DOI": "10.1042/BCJ20170042",
"article-title": "Vitamin D deficiency and diabetes",
"author": "Berridge",
"doi-asserted-by": "crossref",
"first-page": "1321",
"journal-title": "Biochem. J.",
"key": "ref_37",
"volume": "474",
"year": "2017"
},
{
"DOI": "10.1002/cbf.3648",
"article-title": "Genetic and epigenetic control of ACE2 expression and its possible role in COVID-19",
"author": "Lima",
"doi-asserted-by": "crossref",
"first-page": "713",
"journal-title": "Cell Biochem. Funct.",
"key": "ref_38",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.2217/epi-2021-0057",
"article-title": "Epigenomics in COVID-19; the link between DNA methylation, histone modifications and SARS-CoV-2 infection",
"author": "Shirvaliloo",
"doi-asserted-by": "crossref",
"first-page": "745",
"journal-title": "Epigenomics",
"key": "ref_39",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/nu14030464",
"doi-asserted-by": "crossref",
"key": "ref_40",
"unstructured": "Thacher, T.D. (2022). Evaluating the Evidence in Clinical Studies of Vitamin D in COVID-19. Nutrients, 14."
},
{
"DOI": "10.1159/000458765",
"article-title": "Vitamin D Status, Gender Differences and Cardiometabolic Health Disparities",
"author": "Sanghera",
"doi-asserted-by": "crossref",
"first-page": "79",
"journal-title": "Ann. Nutr. Metab.",
"key": "ref_41",
"volume": "70",
"year": "2017"
},
{
"DOI": "10.1007/s11657-018-0461-5",
"article-title": "Age and gender differences in the prevalence and correlates of vitamin D deficiency",
"author": "AlQuaiz",
"doi-asserted-by": "crossref",
"first-page": "49",
"journal-title": "Arch. Osteoporos.",
"key": "ref_42",
"volume": "13",
"year": "2018"
},
{
"DOI": "10.1542/peds.57.5.794",
"article-title": "Vitamin D toxicity after dieting in hypoparathyroidism",
"author": "Connors",
"doi-asserted-by": "crossref",
"first-page": "794",
"journal-title": "Pediatrics",
"key": "ref_43",
"volume": "57",
"year": "1976"
},
{
"article-title": "Vitamin D Toxicity; Stored and Released from Adipose Tissue?",
"author": "Ziaie",
"first-page": "597",
"journal-title": "Arch. Iran. Med.",
"key": "ref_44",
"volume": "19",
"year": "2016"
},
{
"DOI": "10.3390/molecules24132499",
"doi-asserted-by": "crossref",
"key": "ref_45",
"unstructured": "Perticone, M., Maio, R., Sciacqua, A., Suraci, E., Pinto, A., Pujia, R., Zito, R., Gigliotti, S., Sesti, G., and Perticone, F. (2019). Ketogenic Diet-Induced Weight Loss is Associated with an Increase in Vitamin D Levels in Obese Adults. Molecules, 24."
}
],
"reference-count": 45,
"references-count": 45,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/14/24/5204"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Correlation between 25-hydroxyvitamin D/D3 Deficiency and COVID-19 Disease Severity in Adults from Northern Colorado",
"type": "journal-article",
"volume": "14"
}
