Evaluation of Vitamin-D Status and Its Association with Clinical Outcomes Among COVID-19 Patients in Pakistan
et al., Am. J. Trop. Med. Hyg., doi:10.4269/ajtmh.21-0577, Nov 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 91 hospitalized patients in Pakistan, showing vitamin D deficiency associated with mortality in multivariate Cox regression.
This is the 102nd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
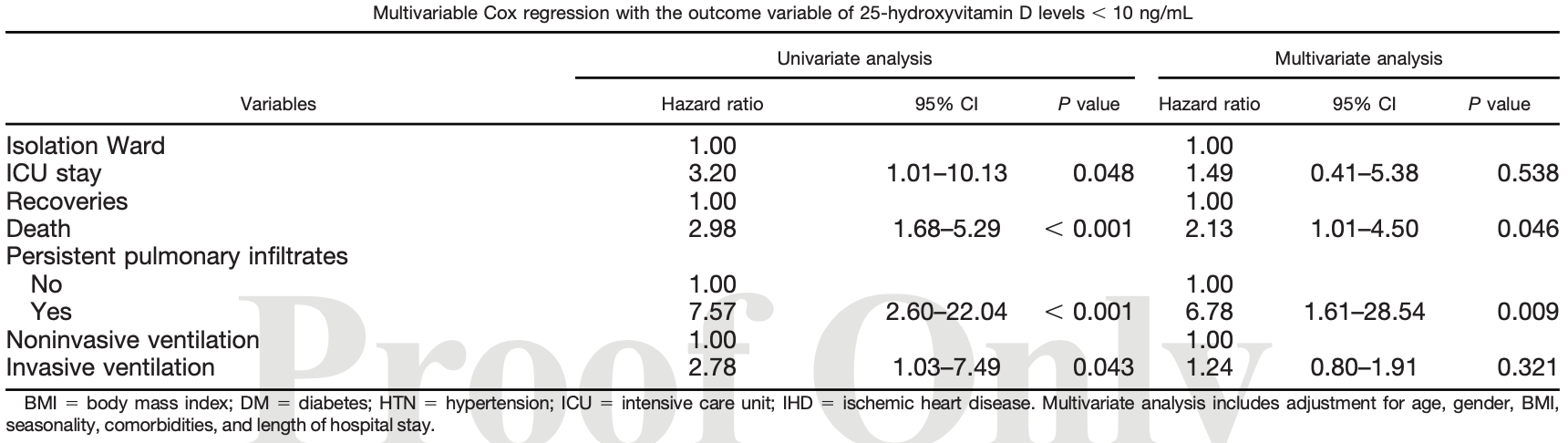
risk of death, 53.1% lower, HR 0.47, p = 0.046, high D levels (≥10ng/mL) 73, low D levels (<10ng/mL) 18, inverted to make HR<1 favor high D levels (≥10ng/mL), multivariate Cox regression.
|
|
risk of mechanical ventilation, 19.4% lower, HR 0.81, p = 0.32, high D levels (≥10ng/mL) 5 of 73 (6.8%), low D levels (<10ng/mL) 6 of 18 (33.3%), NNT 3.8, adjusted per study, inverted to make HR<1 favor high D levels (≥10ng/mL), multivariate Cox regression.
|
|
risk of ICU admission, 32.9% lower, HR 0.67, p = 0.54, high D levels (≥10ng/mL) 73, low D levels (<10ng/mL) 18, inverted to make HR<1 favor high D levels (≥10ng/mL), multivariate Cox regression.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Asghar et al., 10 Nov 2021, retrospective, Pakistan, peer-reviewed, 8 authors.
Evaluation of Vitamin-D Status and Its Association with Clinical Outcomes Among COVID-19 Patients in Pakistan
The American Journal of Tropical Medicine and Hygiene, doi:10.4269/ajtmh.21-0577
The risk of acute respiratory tract infections is particularly pronounced in patients deficient in 25-hydroxyvitamin D (25(OH)D). With respect to COVID-19, there are conflicting evidence on the association of 25(OH)D levels with disease severity. We undertook this study to evaluate the 25(OH)D status in COVID-19 patients admitted in Karachi, Pakistan, and associated vitamin D deficiency with primary outcomes of mortality, length of stay, intubation, and frequency of COVID-19 symptoms. A total of 91 patients were evaluated for 25(OH)D status during their COVID-19 disease course. 25-hydroxyvitamin D levels were classified as deficient (, 10 ng/mL), insufficient (10-30 ng/mL), or sufficient (. 30 ng/mL). The study population comprised 68.1% males (N 5 62). The mean age was 52.6 6 15.7 years. Vitamin D deficiency was significantly associated with intensive care unit (ICU) admission (RR: 3.20; P 5 0.048), invasive ventilation (RR: 2.78; P 5 0.043), persistent pulmonary infiltrates (RR: 7.58; P , 0.001), and death (RR: 2.98; P , 0.001) on univariate Cox regression. On multivariate Cox regression, only death (RR: 2.13; P 5 0.046) and persistent pulmonary infiltrates (RR: 6.78; P 5 0.009) remained significant after adjustment for confounding factors. On Kaplan Meier curves, vitamin D deficient patients had persistent pulmonary infiltrates and a greater probability of requiring mechanical ventilation than patients with 25(OH)D $ 10 ng/mL. Mechanical ventilation had to be initiated early in the deficient group during the 30-day hospital stay (Chi-square: 4.565, P 5 0.033). Patients with 25(OH)D $ 10 ng/mL also demonstrated a higher probability of survival than those with 25(OH)D concentrations , 10 ng/mL. 25-hydroxyvitamin D deficient population had longer hospital stays and worse outcomes.
References
Abrishami, Dalili, Torbati, Asgari, Arab-Ahmadi et al., Possible association of vitamin D status with lung involvement and outcome in patients with COVID-19: a retrospective study, Eur J Nutr
Baktash, Hosack, Patel, Shah, Kandiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med J
G€ Uven, G€ Ultekin H, The effect of high-dose parenteral vitamin D3 on COVID-19-related inhospital mortality in critical COVID-19 patients during intensive care unit admission: an observational cohort study, Eur J Clin Nutr
Hutchings, Patients hospitalized with COVID-19 have low levels of 25-hydroxyvitamin D, Endocrine
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One
Kloc, Ghobrial, Lipi Nska-Opałka, Wawrzyniak, Zdanowski et al., Effects of vitamin D on macrophages and myeloid-derived suppressor cells (MDSCs) hyperinflammatory response in the lungs of COVID-19 patients, Cell Immunol
Kumar, Rathi, Haq, Wimalawansa, Sharma, Putative roles of vitamin D in modulating immune response and immunopathology associated with COVID-19, Virus Res
Mahdavi, A brief review of interplay between vitamin D and angiotensin-converting enzyme 2: implications for a potential treatment for COVID-19, Rev Med Virol
Mercola, Grant, Wagner, Evidence regarding vitamin D and risk of COVID-19 and its severity, Nutrients
Murai, Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, JAMA
Szeto, Zucker, Lasota, Rubin, Walker et al., Vitamin D status and COVID-19 clinical outcomes in hospitalized patients, Endocr Res
Waldron, Ashby, Cornes, Bechervaise, Razavi et al., Vitamin D: a negative acute phase reactant, J Clin Pathol
Weir, Thenappan, Bhargava, Chen, Does vitamin D deficiency increase the severity of COVID-19?, Clin Med (Lond)
Yisak, Ewunetei, Kefale, Mamuye, Teshome et al., Effects of vitamin D on COVID-19 infection and prognosis: a systematic review, Risk Manag Healthc Policy
DOI record:
{
"DOI": "10.4269/ajtmh.21-0577",
"ISSN": [
"0002-9637",
"1476-1645"
],
"URL": "http://dx.doi.org/10.4269/ajtmh.21-0577",
"abstract": "<jats:title>ABSTRACT.</jats:title>\n<jats:p>The risk of acute respiratory tract infections is particularly pronounced in patients deficient in 25-hydroxyvitamin D (25(OH)D). With respect to COVID-19, there are conflicting evidence on the association of 25(OH)D levels with disease severity. We undertook this study to evaluate the 25(OH)D status in COVID-19 patients admitted in Karachi, Pakistan, and associated vitamin D deficiency with primary outcomes of mortality, length of stay, intubation, and frequency of COVID-19 symptoms. A total of 91 patients were evaluated for 25(OH)D status during their COVID-19 disease course. 25-hydroxyvitamin D levels were classified as deficient (< 10 ng/mL), insufficient (10–30 ng/mL), or sufficient (> 30 ng/mL). The study population comprised 68.1% males (<jats:italic>N</jats:italic> = 62). The mean age was 52.6 ± 15.7 years. Vitamin D deficiency was significantly associated with intensive care unit (ICU) admission (RR: 3.20; <jats:italic>P</jats:italic> = 0.048), invasive ventilation (RR: 2.78; <jats:italic>P</jats:italic> = 0.043), persistent pulmonary infiltrates (RR: 7.58; <jats:italic>P</jats:italic> < 0.001), and death (RR: 2.98; <jats:italic>P</jats:italic> < 0.001) on univariate Cox regression. On multivariate Cox regression, only death (RR: 2.13; <jats:italic>P</jats:italic> = 0.046) and persistent pulmonary infiltrates (RR: 6.78; <jats:italic>P</jats:italic> = 0.009) remained significant after adjustment for confounding factors. On Kaplan Meier curves, vitamin D deficient patients had persistent pulmonary infiltrates and a greater probability of requiring mechanical ventilation than patients with 25(OH)D ≥ 10 ng/mL. Mechanical ventilation had to be initiated early in the deficient group during the 30-day hospital stay (Chi-square: 4.565, <jats:italic>P</jats:italic> = 0.033). Patients with 25(OH)D ≥ 10 ng/mL also demonstrated a higher probability of survival than those with 25(OH)D concentrations < 10 ng/mL. 25-hydroxyvitamin D deficient population had longer hospital stays and worse outcomes.</jats:p>",
"author": [
{
"affiliation": [
{
"name": "1Department of Internal Medicine, Dow University of Health Sciences–Ojha Campus, Karachi, Pakistan;"
}
],
"family": "Asghar",
"given": "Muhammad Sohaib",
"sequence": "first"
},
{
"affiliation": [
{
"name": "2Department of Internal Medicine, Dow University of Health Sciences, Karachi, Pakistan;"
}
],
"family": "Yasmin",
"given": "Farah",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "3Indira Gandhi Government Medical College, Nagpur, India;"
}
],
"family": "Dapke",
"given": "Kartik",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "4Department of Internal Medicine, Ziauddin Medical University, Karachi, Pakistan;"
}
],
"family": "Shah",
"given": "Syed Muhammad Ismail",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "2Department of Internal Medicine, Dow University of Health Sciences, Karachi, Pakistan;"
}
],
"family": "Zafar",
"given": "Muhammad Daim Bin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "2Department of Internal Medicine, Dow University of Health Sciences, Karachi, Pakistan;"
}
],
"family": "Khan",
"given": "Anosh Aslam",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "2Department of Internal Medicine, Dow University of Health Sciences, Karachi, Pakistan;"
}
],
"family": "Mohiuddin",
"given": "Osama",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "5Adjunct Clinical Professor of Medicine and Pharmacology, Texas A&M University, College Station, Texas"
}
],
"family": "Surani",
"given": "Salim",
"sequence": "additional"
}
],
"container-title": "The American Journal of Tropical Medicine and Hygiene",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
11,
10
]
],
"date-time": "2021-11-10T12:40:38Z",
"timestamp": 1636548038000
},
"deposited": {
"date-parts": [
[
2022,
1,
5
]
],
"date-time": "2022-01-05T12:08:59Z",
"timestamp": 1641384539000
},
"indexed": {
"date-parts": [
[
2023,
4,
26
]
],
"date-time": "2023-04-26T10:18:23Z",
"timestamp": 1682504303360
},
"is-referenced-by-count": 2,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
1,
5
]
]
},
"journal-issue": {
"issue": "1"
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
5
]
],
"date-time": "2022-01-05T00:00:00Z",
"timestamp": 1641340800000
}
}
],
"link": [
{
"URL": "https://www.ajtmh.org/view/journals/tpmd/106/1/article-p150.xml",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.ajtmh.org/downloadpdf/journals/tpmd/106/1/article-p150.xml",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "2795",
"original-title": [],
"page": "150-155",
"prefix": "10.4269",
"published": {
"date-parts": [
[
2022,
1,
5
]
]
},
"published-print": {
"date-parts": [
[
2022,
1,
5
]
]
},
"publisher": "American Society of Tropical Medicine and Hygiene",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.ajtmh.org/view/journals/tpmd/106/1/article-p150.xml"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Virology",
"Infectious Diseases",
"Parasitology"
],
"subtitle": [],
"title": "Evaluation of Vitamin-D Status and Its Association with Clinical Outcomes Among COVID-19 Patients in Pakistan",
"type": "journal-article",
"volume": "106"
}
