Effects of antidiabetic drugs on mortality risks in individuals with type 2 diabetes: A prospective cohort study of UK Biobank participants
et al., medRxiv, doi:10.1101/2023.05.19.23290214, May 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
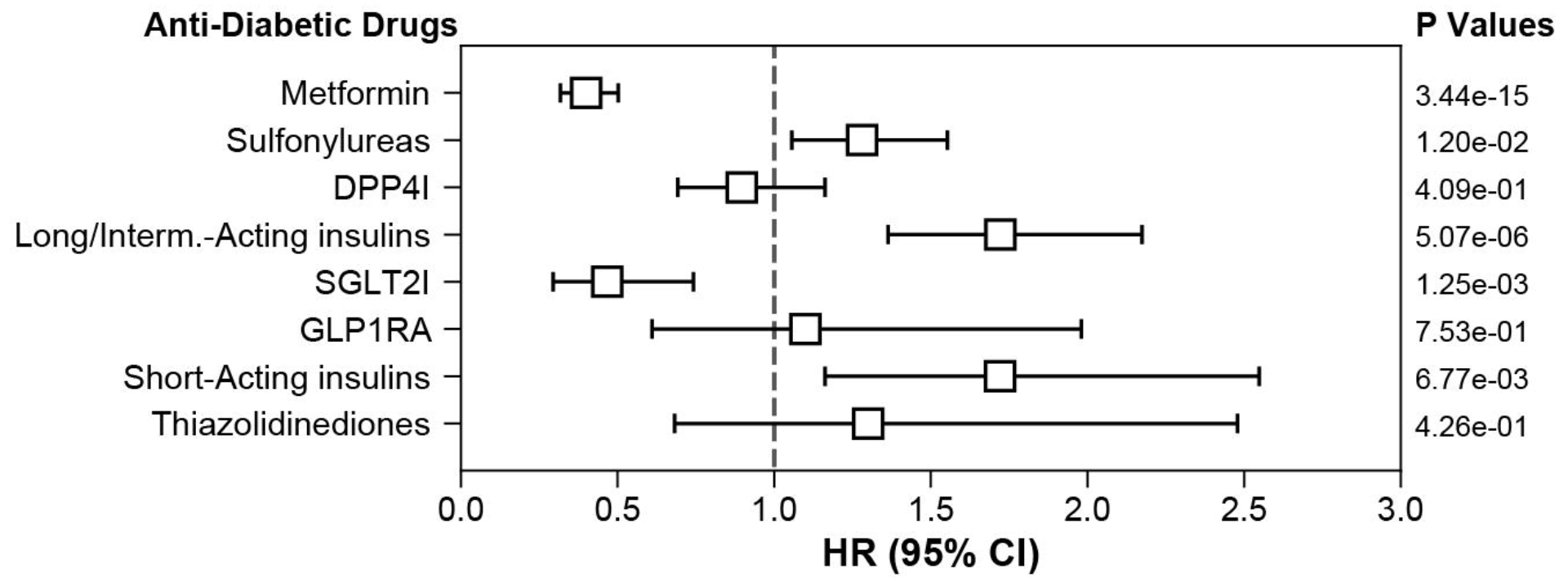
UK Biobank retrospective including 43,610 type 2 diabetes patients, showing lower mortality with metformin use within matched type 2 diabetes patients.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 60.0% lower, HR 0.40, p < 0.001, treatment 107 of 2,598 (4.1%), control 263 of 2,598 (10.1%), NNT 17, adjusted per study, type 2 diabetes patients, matched cohort, multivariable, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Araldi et al., 19 May 2023, retrospective, United Kingdom, preprint, 3 authors.
Contact: michael.ristow@charite.de.
Effects of antidiabetic drugs on mortality risks in individuals with type 2 diabetes: A prospective cohort study of UK Biobank participants
doi:10.1101/2023.05.19.23290214
Objective: To investigate the mortality risk linked to prescription of different anti-diabetic medication classes. Design: Prospective population-based study. Setting: UK Biobank. Participants: 410 389 of the 502 536 participants in UK Biobank with covariate data, clinical and prescription records were included in the analyses, 43 610 of which had been diagnosed type 2 diabetes (T2D). A nearest neighbour covariate matching (NNCM) algorithm based on covariates with relevant effects on survival was applied to match cohorts of anti-diabetic medication class users to minimally differing control cohorts, either with a T2D diagnosis or without. Kaplan Meier estimates and Cox proportional models were used to evaluate survival differences and hazard ratio between drug classes and controls. Main outcome measures: All-cause mortality and causes of death. Results : 13667 (3.3%) individuals died during a median of 12.2 years of follow-up. After applying NNCM, participants with T2D on metformin (average hazard ratio 0.39, 95% confidence interval 0.31 to 0.49) or SGLT2I (average hazard ratio 0.58, 95% confidence interval 0.36 to 0.93) have an increased survival probability compared to matched individuals with T2D. When compared to matched individuals without T2D, the survival probability of individuals with T2D increases only if prescribed SGLT2I (average hazard ratio 0.31, 95% confidence interval 0.19 to 0.51). NNCMbased analysis of matched individuals with T2D on both SGLT2I and metformin versus metformin only reveals increased survival in the presence of SGLT2I (average hazard ratio 0.29, 95% confidence interval 0.09 to 0.91), also when compared to matched identical individuals without T2D (average hazard ratio 0.05, 95% confidence interval 0.01 to 0.19). All the other anti-diabetic drugs analyzed are either detrimental in prolonging lifespan (insulin, thiazolidinediones, and sulfonylureas), or have no effect (DPP4 inhibitors and GLP1 receptor agonists).
Conclusion: The use of the current first-line anti-diabetic treatment, metformin, or sodiumglucose cotransporter 2 inhibitors (SGLT2I) increases the survival probability compared to matched individuals with diabetes using other anti-diabetic drugs. Only individuals on SGLT2I experience increased survival when compared to individuals without T2D.
Contributors EA and MR designed the study. EA conducted the statistical analysis. EA and MR wrote the first draft. EA, CRJ, and MR critically revised the manuscript. MR is the guarantor of the manuscript and accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Ethics approval UK Biobank has obtained ethics approval from the North West Multi-Centre Research Ethics Committee (approval number: 11/NW/0382) and has obtained informed consent from all participants.
Transparency statement The manuscript's guarantor (MR) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Competing interests
All
References
Atkins, Masoli, Delgado, Preexisting Comorbidities Predicting COVID-19 and Mortality in the UK Biobank Community Cohort, J Gerontol A Biol Sci Med Sci, doi:10.1093/gerona/glaa183
Austin, A comparison of 12 algorithms for matching on the propensity score, Stat Med, doi:10.1002/sim.6004
Barzilai, Crandall, Kritchevsky, Metformin as a tool to target aging, Cell Metab, doi:10.1016/j.cmet.2016.05.011
Buse, Wexler, Tsapas, Update to: Management of Hyperglycemia in Type 2 Diabetes, doi:10.2337/dci19-0066
Bycroft, Freeman, Petkova, The UK Biobank resource with deep phenotyping and genomic data, Nature, doi:10.1038/s41586-018-0579
Ceriello, Prattichizzo, Phillip, Glycaemic management in diabetes: old and new approaches, The lancet Diabetes & endocrinology, doi:10.1016/S2213-8587(21)00245-X[publishedOnlineFirst:2021/11/19
Davies, Aroda, Collins, Management of Hyperglycemia in Type 2 Diabetes, doi:10.2337/dci22-0034
Fang, Wang, Coresh, Trends in Diabetes Treatment and Control in U.S. Adults, 1999-2018, N Engl J Med, doi:10.1056/NEJMsa2032271
Ferrannini, Solini, SGLT2 inhibition in diabetes mellitus: rationale and clinical prospects, Nat Rev Endocrinol, doi:10.1038/nrendo.2011.243
Garcia, Arteche-Martinez, Lertxundi, SGLT2 Inhibitors and Bladder Cancer: Analysis of Cases Reported in the European Pharmacovigilance Database, J Clin Pharmacol, doi:10.1002/jcph.1722
Group, Nathan, Lachin, Glycemia Reduction in Type 2 Diabetes -Glycemic Outcomes, N Engl J Med, doi:10.1056/NEJMoa2200433
Holman, Paul, Bethel, 10-year follow-up of intensive glucose control in type 2 diabetes, N Engl J Med, doi:10.1056/NEJMoa0806470
Ito, Inoue, Saito, Effects of Dapagliflozin Compared with Sitagliptin and Metformin in Drug-Naive Japanese Patients with Type 2 Diabetes: A 12-Week, Open-Label, Randomized, Active-Controlled Trial, Diabetes Ther, doi:10.1007/s13300-021-01176-x
Kalyani, Glucose-lowering drugs to reduce cardiovascular risk in type 2 diabetes, N Engl J Med, doi:10.1056/NEJMcp2000280
Kaul, Is the Mortality Benefit With Empagliflozin in Type 2 Diabetes Mellitus Too Good To Be True?, Circulation, doi:10.1161/CIRCULATIONAHA.116.022537
Kondapally Seshasai, Kaptoge, Thompson, Diabetes mellitus, fasting glucose, and risk of cause-specific death, N Engl J Med, doi:10.1056/NEJMoa1008862
Kyriacou, Lewis, Confounding by Indication in Clinical Research, JAMA, doi:10.1001/jama.2016.16435[publishedOnlineFirst:2016/11/02
Panzram, Mortality and survival in type 2 (non-insulin-dependent) diabetes mellitus, Diabetologia, doi:10.1007/BF00274216
Pelletier, Ng, Alkabbani, The association of sodium-glucose cotransporter 2 inhibitors with cancer: An overview of quantitative systematic reviews, Endocrinol Diabetes Metab, doi:10.1002/edm2.145
Ravichandran, Grandl, Ristow, Dietary carbohydrates impair healthspan and promote mortality, Cell Metab, doi:10.1016/j.cmet.2017.09.011
Shields, Dennis, Angwin, Patient stratification for determining optimal second-line and third-line therapy for type 2 diabetes: the TriMaster study, Nat Med, doi:10.1038/s41591-022-02120-7
Stuart, Matching methods for causal inference: A review and a look forward, Stat Sci, doi:10.1214/09-STS313
Sudlow, Gallacher, Allen, UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age, PLoS Med, doi:10.1371/journal.pmed.1001779
Szeker, Vathy-Fogarassy, Weighted nearest neighbours-based control group selection method for observational studies, PLoS One, doi:10.1371/journal.pone.0236531
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wu, Foote, Blomster, Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular events, death, and major safety outcomes in adults with type 2 diabetes: a systematic review and meta-analysis, The lancet Diabetes & endocrinology, doi:10.1016/S2213-8587(16)00052-8
Yadav, Lewis, Immortal Time Bias in Observational Studies, JAMA, doi:10.1001/jama.2020.9151
Zheng, Roddick, Aghar-Jaffar, Association Between Use of Sodium-Glucose Cotransporter 2 Inhibitors, Glucagon-like Peptide 1 Agonists, and Dipeptidyl Peptidase 4 Inhibitors With All-Cause Mortality in Patients With Type 2 Diabetes: A Systematic Review and Meta-analysis, JAMA, doi:10.1001/jama.2018.3024
Zinman, Wanner, Lachin, Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes, N Engl J Med, doi:10.1056/NEJMoa1504720
DOI record:
{
"DOI": "10.1101/2023.05.19.23290214",
"URL": "http://dx.doi.org/10.1101/2023.05.19.23290214",
"abstract": "<jats:p>Objective: To investigate the mortality risk linked to prescription of different anti-diabetic medication classes. Design: Prospective population-based study. Setting UK Biobank. Participants: 410 389 of the 502 536 participants in UK Biobank with covariate data, clinical and prescription records were included in the analyses, 43 610 of which had been diagnosed type 2 diabetes (T2D). A nearest neighbour covariate matching (NNCM) algorithm based on covariates with relevant effects on survival was applied to match cohorts of anti-diabetic medication class users to minimally differing control cohorts, either with a T2D diagnosis or without. Kaplan Meier estimates and Cox proportional models were used to evaluate survival differences and hazard ratio between drug classes and controls. Main outcome measures: All-cause mortality and causes of death. Results: 13667 (3.3%) individuals died during a median of 12.2 years of follow-up. After applying NNCM, participants with T2D on metformin (average hazard ratio 0.39, 95% confidence interval 0.31 to 0.49) or SGLT2I (average hazard ratio 0.58, 95% confidence interval 0.36 to 0.93) have an increased survival probability compared to matched individuals with T2D. When compared to matched individuals without T2D, the survival probability of individuals with T2D increases only if prescribed SGLT2I (average hazard ratio 0.31, 95% confidence interval 0.19 to 0.51). NNCM-based analysis of matched individuals with T2D on both SGLT2I and metformin versus metformin only reveals increased survival in the presence of SGLT2I (average hazard ratio 0.29, 95% confidence interval 0.09 to 0.91), also when compared to matched identical individuals without T2D (average hazard ratio 0.05, 95% confidence interval 0.01 to 0.19). All the other anti-diabetic drugs analyzed are either detrimental in prolonging lifespan (insulin, thiazolidinediones, and sulfonylureas), or have no effect (DPP4 inhibitors and GLP1 receptor agonists). Conclusion: The use of the current first-line anti-diabetic treatment, metformin, or sodium-glucose cotransporter 2 inhibitors (SGLT2I) increases the survival probability compared to matched individuals with diabetes using other anti-diabetic drugs. Only individuals on SGLT2I experience increased survival when compared to individuals without T2D.</jats:p>",
"accepted": {
"date-parts": [
[
2023,
5,
19
]
]
},
"author": [
{
"ORCID": "http://orcid.org/0000-0002-6596-6784",
"affiliation": [],
"authenticated-orcid": false,
"family": "Araldi",
"given": "Elisa",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-7167-8271",
"affiliation": [],
"authenticated-orcid": false,
"family": "Jutzeler",
"given": "Catherine R",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2109-2453",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ristow",
"given": "Michael",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
5,
19
]
],
"date-time": "2023-05-19T23:45:11Z",
"timestamp": 1684539911000
},
"deposited": {
"date-parts": [
[
2023,
5,
19
]
],
"date-time": "2023-05-19T23:45:11Z",
"timestamp": 1684539911000
},
"group-title": "Endocrinology (including Diabetes Mellitus and Metabolic Disease)",
"indexed": {
"date-parts": [
[
2023,
5,
20
]
],
"date-time": "2023-05-20T04:39:56Z",
"timestamp": 1684557596432
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
5,
19
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2023.05.19.23290214",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2023,
5,
19
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2023,
5,
19
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2023.05.19.23290214"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Effects of antidiabetic drugs on mortality risks in individuals with type 2 diabetes: A prospective cohort study of UK Biobank participants",
"type": "posted-content"
}
