Survival implications vs. complications: unraveling the impact of vitamin D adjunctive use in critically ill patients with COVID-19—A multicenter cohort study
et al., Frontiers in Medicine, doi:10.3389/fmed.2023.1237903, Aug 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
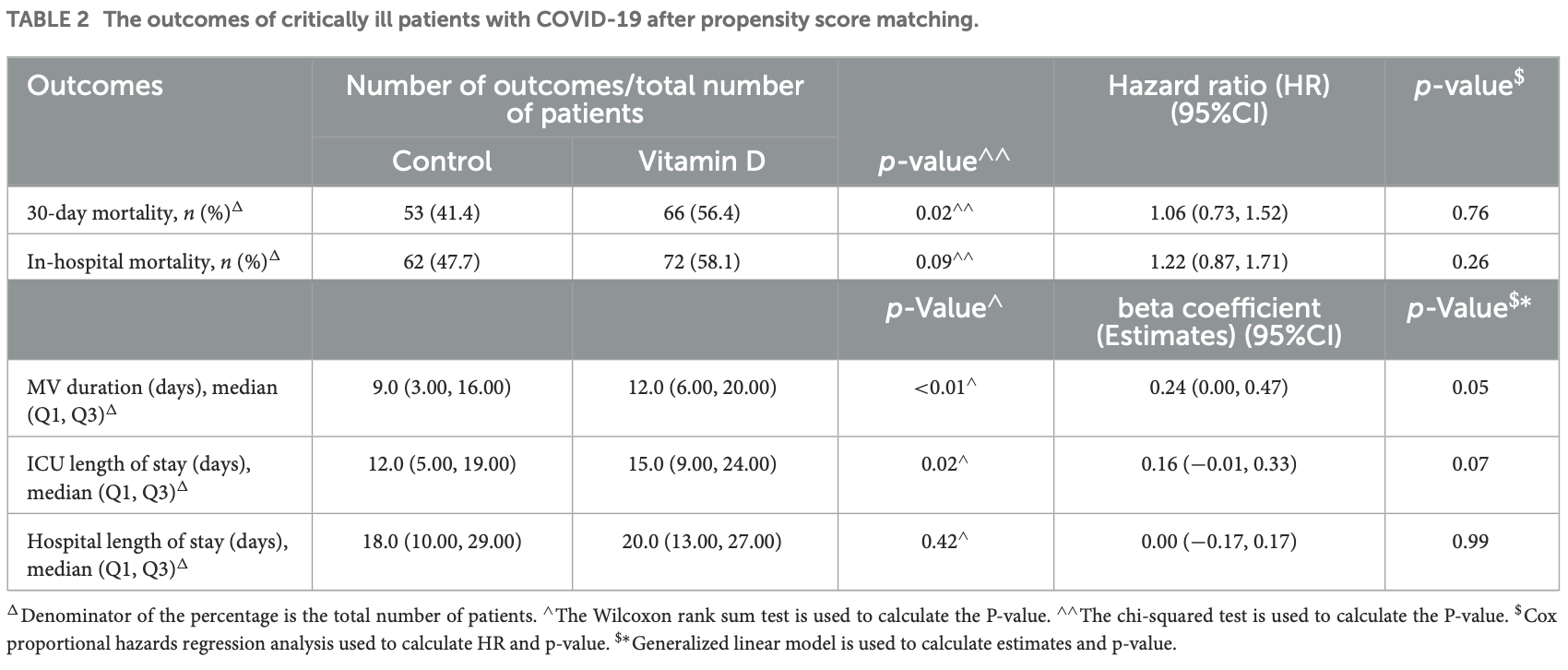
Retrospective 1,435 ICU patients in Saudi Arabia, showing no significant difference in mortality, and longer mechanical ventilation with treatment. Vitamin D patients had higher Q1, median, and Q3 SOFA scores after propensity score matching. 98% of patients were treated with cholecalciferol.
Cholecalciferol was used in this study.
Meta-analysis shows that late stage treatment with calcitriol / calcifediol (or
paricalcitol, alfacalcidol, etc.) is more effective than cholecalciferol: 66% [47‑78%] lower risk vs. 44% [33‑53%] lower risk.
Cholecalciferol requires two hydroxylation steps to become activated - first
in the liver to calcifediol, then in the kidney to calcitriol. Calcitriol,
paricalcitol, and alfacalcidol are active vitamin D analogs that do not
require conversion. This allows them to have more rapid onset of action
compared to cholecalciferol. The time delay for cholecalciferol to increase
serum calcifediol levels can be 2-3 days, and the delay for converting
calcifediol to active calcitriol can be up to 7 days.
This is the 123rd of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
This study is excluded in the after exclusion results of meta-analysis:
very late stage study using cholecalciferol instead of calcifediol or calcitriol.
|
risk of death, 22.0% higher, HR 1.22, p = 0.25, treatment 72 of 144 (50.0%), control 62 of 144 (43.1%).
|
|
risk of mechanical ventilation, 27.0% higher, OR 1.27, p = 0.046, treatment 144, control 144, RR approximated with OR.
|
|
risk of ICU admission, 17.0% higher, OR 1.17, p = 0.07, treatment 144, control 144, RR approximated with OR.
|
|
risk of hospitalization, no change, OR 1.00, p = 1.00, treatment 144, control 144, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Al Sulaiman et al., 14 Aug 2023, retrospective, Saudi Arabia, peer-reviewed, 25 authors, study period March 2020 - July 2021, dosage not specified.
DOI record:
{
"DOI": "10.3389/fmed.2023.1237903",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2023.1237903",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>Despite insufficient evidence, vitamin D has been used as adjunctive therapy in critically ill patients with COVID-19. This study evaluates the effectiveness and safety of vitamin D as an adjunctive therapy in critically ill COVID-19 patients.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>A multicenter retrospective cohort study that included all adult COVID-19 patients admitted to the intensive care units (ICUs) between March 2020 and July 2021. Patients were categorized into two groups based on their vitamin D use throughout their ICU stay (control vs. vitamin D). The primary endpoint was in-hospital mortality. Secondary outcomes were the length of stay (LOS), mechanical ventilation (MV) duration, and ICU-acquired complications. Propensity score (PS) matching (1:1) was used based on the predefined criteria. Multivariable logistic, Cox proportional hazards, and negative binomial regression analyses were employed as appropriate.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>A total of 1,435 patients were included in the study. Vitamin D was initiated in 177 patients (12.3%), whereas 1,258 patients did not receive it. A total of 288 patients were matched (1:1) using PS. The in-hospital mortality showed no difference between patients who received vitamin D and the control group (HR 1.22, 95% CI 0.87–1.71; <jats:italic>p</jats:italic> = 0.26). However, MV duration and ICU LOS were longer in the vitamin D group (beta coefficient 0.24 (95% CI 0.00–0.47), <jats:italic>p</jats:italic> = 0.05 and beta coefficient 0.16 (95% CI −0.01 to 0.33), <jats:italic>p</jats:italic> = 0.07, respectively). As an exploratory outcome, patients who received vitamin D were more likely to develop major bleeding than those who did not [OR 3.48 (95% CI 1.10, 10.94), <jats:italic>p</jats:italic> = 0.03].</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>The use of vitamin D as adjunctive therapy in COVID-19 critically ill patients was not associated with survival benefits but was linked with longer MV duration, ICU LOS, and higher odds of major bleeding.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fmed.2023.1237903"
],
"author": [
{
"affiliation": [],
"family": "Al Sulaiman",
"given": "Khalid",
"sequence": "first"
},
{
"affiliation": [],
"family": "Korayem",
"given": "Ghazwa B.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aljuhani",
"given": "Ohoud",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Altebainawi",
"given": "Ali F.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shawaqfeh",
"given": "Mohammad S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alarfaj",
"given": "Sumaiah J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alharbi",
"given": "Reham A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ageeli",
"given": "Mawaddah M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alissa",
"given": "Abdulrahman",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vishwakarma",
"given": "Ramesh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ibrahim",
"given": "Alnada",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alenazi",
"given": "Abeer A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alghnam",
"given": "Suliman",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alshehri",
"given": "Nadiyah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alshammari",
"given": "Maqbulah M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alhubaishi",
"given": "Alaa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aldhaeefi",
"given": "Mohammed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alamri",
"given": "Faisal F.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Syed",
"given": "Yadullah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khan",
"given": "Raymond",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alalawi",
"given": "Mai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alanazi",
"given": "Khalaf A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alresayes",
"given": "Faisal S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Albarqi",
"given": "Khalid J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Al Ghamdi",
"given": "Ghassan",
"sequence": "additional"
}
],
"container-title": "Frontiers in Medicine",
"container-title-short": "Front. Med.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
8,
25
]
],
"date-time": "2023-08-25T03:02:12Z",
"timestamp": 1692932532000
},
"deposited": {
"date-parts": [
[
2023,
8,
25
]
],
"date-time": "2023-08-25T03:02:17Z",
"timestamp": 1692932537000
},
"indexed": {
"date-parts": [
[
2023,
8,
26
]
],
"date-time": "2023-08-26T08:16:04Z",
"timestamp": 1693037764963
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
8,
24
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
8,
24
]
],
"date-time": "2023-08-24T00:00:00Z",
"timestamp": 1692835200000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2023.1237903/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
8,
24
]
]
},
"published-online": {
"date-parts": [
[
2023,
8,
24
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1097/JCMA.0000000000000270",
"article-title": "The outbreak of COVID-19: an overview",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "217",
"journal-title": "J Chinese Med Assoc.",
"key": "B1",
"volume": "83",
"year": "2020"
},
{
"DOI": "10.7326/M20-6448",
"doi-asserted-by": "publisher",
"first-page": "93",
"journal-title": "Annal Int Med",
"key": "B2",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.2174/1389557515666150519110830",
"article-title": "Vitamin-D in the immune system: genomic and non-genomic actions",
"author": "Trochoutsou",
"doi-asserted-by": "publisher",
"first-page": "953",
"journal-title": "Mini-Rev Med Chem",
"key": "B3",
"volume": "15",
"year": "2015"
},
{
"DOI": "10.1017/S0950268806007175",
"article-title": "Epidemic influenza and vitamin D",
"author": "Cannell",
"doi-asserted-by": "publisher",
"first-page": "1129",
"journal-title": "Epidemiol Infect.",
"key": "B4",
"volume": "134",
"year": "2006"
},
{
"DOI": "10.1186/s13054-018-2185-8",
"article-title": "Vitamin D deficiency and supplementation in critical illness - The known knowns and known unknowns",
"author": "Nair",
"doi-asserted-by": "publisher",
"first-page": "276",
"journal-title": "Crit Care.",
"key": "B5",
"volume": "22",
"year": "2018"
},
{
"DOI": "10.1186/cc10120",
"article-title": "Short-term effects of high-dose oral vitamin D3 in critically ill vitamin D deficient patients: a randomized, double-blind, placebo-controlled pilot study",
"author": "Amrein",
"doi-asserted-by": "publisher",
"first-page": "R104",
"journal-title": "Crit Care.",
"key": "B6",
"volume": "15",
"year": "2011"
},
{
"DOI": "10.1016/j.earlhumdev.2006.05.022",
"article-title": "Measurement of pain-like response to various NICU stimulants for high-risk infants",
"author": "Ahn",
"doi-asserted-by": "publisher",
"first-page": "255",
"journal-title": "Early Hum Dev.",
"key": "B7",
"volume": "83",
"year": "2007"
},
{
"DOI": "10.1001/jama.2014.13204",
"article-title": "Effect of high-dose vitamin D3on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial",
"author": "Amrein",
"doi-asserted-by": "publisher",
"first-page": "1520",
"journal-title": "JAMA - J Am Med Assoc.",
"key": "B8",
"volume": "312",
"year": "2014"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"article-title": "Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers",
"author": "Jain",
"doi-asserted-by": "publisher",
"first-page": "20191",
"journal-title": "Sci Rep.",
"key": "B9",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1093/ajcn/nqab227",
"article-title": "Influence of vitamin D status on hospital length of stay and prognosis in hospitalized patients with moderate to severe COVID-19: a multicenter prospective cohort study",
"author": "Reis",
"doi-asserted-by": "publisher",
"first-page": "598",
"journal-title": "Am J Clin Nutr.",
"key": "B10",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.1101/2022.02.03.22270409",
"article-title": "Vitamin D and acute respiratory infection: secondary analysis of a previous randomised controlled trial and updated meta-analyses",
"author": "Bolland",
"doi-asserted-by": "publisher",
"first-page": "22270409",
"journal-title": "medRxiv.",
"key": "B11",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.3390/nu12092879",
"article-title": "Immune modulatory effects of vitamin d on viral infections",
"author": "Siddiqui",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Nutrients.",
"key": "B12",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1111/irv.12615",
"article-title": "Effect of Vitamin D supplementation to reduce respiratory infections in children and adolescents in Vietnam: a randomized controlled trial",
"author": "Loeb",
"doi-asserted-by": "publisher",
"first-page": "176",
"journal-title": "Influenza Other Respi Viruses.",
"key": "B13",
"volume": "13",
"year": "2019"
},
{
"DOI": "10.1056/NEJMoa1911124",
"article-title": "3 for Critically Ill, vitamin D–deficient patients",
"author": "Early",
"doi-asserted-by": "publisher",
"first-page": "2529",
"journal-title": "N Engl J Med.",
"key": "B14",
"volume": "381",
"year": "2019"
},
{
"DOI": "10.1093/qjmed/hcac040",
"article-title": "Does vitamin D supplementation reduce COVID-19 severity? A systematic review",
"author": "Shah",
"doi-asserted-by": "publisher",
"first-page": "665",
"journal-title": "QJM.",
"key": "B15",
"volume": "115",
"year": "2022"
},
{
"DOI": "10.1093/qjmed/hcab009",
"article-title": "Vitamin D supplementation, COVID-19 and disease severity: a meta-analysis",
"author": "Shah",
"doi-asserted-by": "publisher",
"first-page": "175",
"journal-title": "QJM.",
"key": "B16",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.1038/s41430-021-00984-5",
"article-title": "The effect of high-dose parenteral vitamin D3 on COVID-19-related in hospital mortality in critical COVID-19 patients during intensive care unit admission: an observational cohort study",
"author": "Güven",
"doi-asserted-by": "publisher",
"first-page": "1383",
"journal-title": "Eur J Clin Nutr.",
"key": "B17",
"volume": "75",
"year": "2021"
},
{
"key": "B18",
"unstructured": ""
},
{
"DOI": "10.1016/j.ijid.2021.02.037",
"article-title": "Clinical features and outcomes of critically ill patients with coronavirus disease 2019 (COVID-19): a multicenter cohort study",
"author": "Al Sulaiman",
"doi-asserted-by": "publisher",
"first-page": "180",
"journal-title": "Int J Infect Dis.",
"key": "B19",
"volume": "105",
"year": "2021"
},
{
"DOI": "10.1186/s12879-021-06813-1",
"article-title": "Association between tocilizumab and emerging multidrug-resistant organisms in critically ill patients with COVID-19: a multicenter, retrospective cohort study",
"author": "Aljuhani",
"doi-asserted-by": "publisher",
"first-page": "1127",
"journal-title": "BMC Infect Dis.",
"key": "B20",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1186/s13054-022-04158-y",
"article-title": "Evaluation of inhaled nitric oxide (iNO) treatment for moderate-to-severe ARDS in critically ill patients with COVID-19: a multicenter cohort study",
"author": "Al Sulaiman",
"doi-asserted-by": "publisher",
"first-page": "304",
"journal-title": "Crit Care.",
"key": "B21",
"volume": "26",
"year": "2022"
},
{
"DOI": "10.1186/s12959-022-00432-9",
"article-title": "Standard dosing of enoxaparin versus unfractionated heparin in critically ill patient with COVID-19: a multicenter propensity-score matched study",
"author": "Al Sulaiman",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Thromb J.",
"key": "B22",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1177/10760296221103864",
"article-title": "Statins and risk of thrombosis in critically ill 1patients with COVID-19: a multicenter cohort study",
"author": "Al Harbi",
"doi-asserted-by": "publisher",
"first-page": "10760",
"journal-title": "Clin Appl Thromb.",
"key": "B23",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1186/s13054-021-03785-1",
"article-title": "Evaluation of zinc sulfate as an adjunctive therapy in COVID-19 critically ill patients: a two center propensity-score matched study",
"author": "Al Sulaiman",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Crit Care.",
"key": "B24",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1186/s12879-023-08010-8",
"article-title": "The clinical outcomes of COVID-19 critically ill patients co-infected with other respiratory viruses: a multicenter, cohort study",
"author": "Al Sulaiman",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "BMC Infect Dis.",
"key": "B25",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"article-title": "The link between COVID-19 and VItamin D (VIVID): a systematic review and meta-analysis",
"author": "Bassatne",
"doi-asserted-by": "publisher",
"first-page": "154753",
"journal-title": "Metabolism.",
"key": "B26",
"volume": "119",
"year": "2021"
},
{
"DOI": "10.1111/cen.14540",
"article-title": "Association of vitamin D deficiency with COVID-19 infection severity: systematic review and meta-analysis",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "281",
"journal-title": "Clin Endocrinol.",
"key": "B27",
"volume": "96",
"year": "2022"
},
{
"DOI": "10.3389/fpubh.2021.624559",
"article-title": "The impact of vitamin d level on COVID-19 infection: systematic review and meta-analysis",
"author": "Teshome",
"doi-asserted-by": "publisher",
"first-page": "169",
"journal-title": "Front Public Heal.",
"key": "B28",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.4103/jfcm.JFCM_73_17",
"article-title": "Vitamin D deficiency in Saudi Arabians: a reality or simply hype: a meta-analysis (2008-2015)",
"author": "Al-Alyani",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Fam Community Med.",
"key": "B29",
"volume": "25",
"year": "2018"
},
{
"DOI": "10.34172/PS.2021.13",
"article-title": "The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: a systematic review and meta-analysis",
"author": "Nikniaz",
"doi-asserted-by": "publisher",
"first-page": "S1",
"journal-title": "Pharm Sci.",
"key": "B30",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.3390/nu14030464",
"article-title": "Evaluating the evidence in clinical studies of vitamin D in COVID-19",
"author": "Thacher",
"doi-asserted-by": "publisher",
"first-page": "464",
"journal-title": "Nutrients.",
"key": "B31",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a single high dose of vitamin d3on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial",
"author": "Murai",
"doi-asserted-by": "publisher",
"first-page": "1053",
"journal-title": "JAMA.",
"key": "B32",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"article-title": "“Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study",
"author": "Entrenas Castillo",
"doi-asserted-by": "publisher",
"first-page": "105751",
"key": "B33",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2021.102189",
"article-title": "“Vitamin D supplementation and COVID-19 treatment: a systematic review and meta-analysis",
"author": "Rawat",
"doi-asserted-by": "publisher",
"first-page": "102189",
"key": "B34",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1136/bmjopen-2020-043737",
"article-title": "Association between vitamin D supplementation or serum vitamin D level and susceptibility to SARS-CoV-2 infection or COVID-19 including clinical course, morbidity and mortality outcomes? A systematic review",
"author": "Grove",
"doi-asserted-by": "publisher",
"first-page": "e043737",
"journal-title": "BMJ Open.",
"key": "B35",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1007/s40618-021-01614-4",
"article-title": "Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis",
"author": "Pal",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "J Endocrinol Invest.",
"key": "B36",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.1016/j.critrevonc.2021.103529",
"article-title": "COVID-19 and immunothrombosis: Pathophysiology and therapeutic implications",
"author": "Lim",
"doi-asserted-by": "publisher",
"first-page": "103529",
"journal-title": "Crit Rev Oncol Hematol.",
"key": "B37",
"volume": "168",
"year": "2021"
},
{
"DOI": "10.1136/thoraxjnl-2020-216243",
"article-title": "COVID-19, immunothrombosis and venous thromboembolism: Biological mechanisms",
"author": "Loo",
"doi-asserted-by": "publisher",
"first-page": "412",
"journal-title": "Thorax.",
"key": "B38",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1007/s42399-020-00521-8",
"article-title": "immune thrombocytopenia secondary to COVID-19: a systematic review",
"author": "Bhattacharjee",
"doi-asserted-by": "publisher",
"first-page": "2048",
"journal-title": "SN Compr Clin Med.",
"key": "B39",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1007/s11010-021-04093-6",
"article-title": "Role of vitamin D in treating COVID-19-associated coagulopathy: problems and perspectives",
"author": "Sengupta",
"doi-asserted-by": "publisher",
"first-page": "2421",
"journal-title": "Mol Cell Biochem.",
"key": "B40",
"volume": "476",
"year": "2021"
},
{
"DOI": "10.1177/1076029620962853",
"article-title": "COVID-19 and hypercoagulability: a review",
"author": "Kichloo",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Clin Appl Thromb Hemostasis",
"key": "B41",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1007/s11239-021-02403-9",
"article-title": "Major bleeding complications in critically ill patients with COVID-19 pneumonia",
"author": "Godier",
"doi-asserted-by": "publisher",
"first-page": "18",
"journal-title": "J Thromb Thrombolysis.",
"key": "B42",
"volume": "52",
"year": "2021"
},
{
"DOI": "10.2139/ssrn.3582758",
"article-title": "Heparin-Induced thrombocytopenia is a high risk of mortality in critical COVID-19 patients receiving heparin-involved treatment",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "758",
"journal-title": "SSRN Electron J.",
"key": "B43",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.3390/biom9110649",
"article-title": "Emerging role of vitamin d and its associated molecules in pathways related to pathogenesis of thrombosis",
"author": "Mohammad",
"doi-asserted-by": "publisher",
"first-page": "649",
"journal-title": "Biomolecules.",
"key": "B44",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1177/1076029614568715",
"article-title": "The effect of high-dose vitamin d3 on soluble p-selectin and hs-CRP level in patients with venous thromboembolism",
"author": "Gholami",
"doi-asserted-by": "publisher",
"first-page": "483",
"journal-title": "Clin Appl Thromb.",
"key": "B45",
"volume": "22",
"year": "2016"
},
{
"DOI": "10.1111/j.1365-2141.2006.06322.x",
"article-title": "High dose calcitriol may reduce thrombosis in cancer patients",
"author": "Beer",
"doi-asserted-by": "publisher",
"first-page": "392",
"journal-title": "Br J Haematol.",
"key": "B46",
"volume": "135",
"year": "2006"
},
{
"DOI": "10.1096/fj.15-272872",
"article-title": "Vitamin D modulates tissue factor and protease-activated receptor 2 expression in vascular smooth muscle cells",
"author": "Martinez-Moreno",
"doi-asserted-by": "publisher",
"first-page": "1367",
"journal-title": "FASEB J.",
"key": "B47",
"volume": "30",
"year": "2016"
},
{
"DOI": "10.1177/1076029613509477",
"article-title": "Is there any association between thrombosis and tissue factor pathway inhibitor levels in patients with vitamin d deficiency?",
"author": "Topaloglu",
"doi-asserted-by": "publisher",
"first-page": "428",
"journal-title": "Clin Appl Thromb.",
"key": "B48",
"volume": "21",
"year": "2015"
},
{
"DOI": "10.1530/EC-19-0429",
"article-title": "Thrombin generation and fibrin clot structure after vitamin D supplementation",
"author": "Blondon",
"doi-asserted-by": "publisher",
"first-page": "1447",
"journal-title": "Endocr Connect.",
"key": "B49",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"article-title": "Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients",
"author": "Angelidi",
"doi-asserted-by": "publisher",
"first-page": "875",
"journal-title": "Mayo Clin Proc.",
"key": "B50",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1002/rmv.2269",
"article-title": "Vitamin D supplementation and Covid-19 outcomes: a systematic review, meta-analysis and meta-regression",
"author": "Hariyanto",
"doi-asserted-by": "publisher",
"first-page": "e2269",
"journal-title": "Rev Med Virol.",
"key": "B51",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.22037/ijpr.2019.1100647",
"article-title": "Effect of high-dose vitamin D on duration of mechanical ventilation in ICU patients",
"author": "Miri",
"doi-asserted-by": "publisher",
"first-page": "1067",
"journal-title": "Iran J Pharm Res.",
"key": "B52",
"volume": "18",
"year": "2019"
},
{
"DOI": "10.1016/j.jcte.2016.04.004",
"article-title": "High dose Vitamin D administration in ventilated intensive care unit patients: a pilot double blind randomized controlled trial",
"author": "Han",
"doi-asserted-by": "publisher",
"first-page": "59",
"journal-title": "J Clin Transl Endocrinol.",
"key": "B53",
"volume": "4",
"year": "2016"
}
],
"reference-count": 53,
"references-count": 53,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2023.1237903/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Survival implications vs. complications: unraveling the impact of vitamin D adjunctive use in critically ill patients with COVID-19—A multicenter cohort study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "10"
}
