The risk of up normal values of two parameters obesity and vitamin D in incidence of coronavirus disease-19 among Iraqi patients
et al., 1st Samarra International Conference for Pure and Applied Sciences (SICPS2021), doi:10.1063/5.0121166, Nov 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 86 COVID-19 hospitalized patients and 86 healthy controls in Iraq, showing COVID-19 cases associated with severe vitamin D deficiency.
This is the 149th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of hospitalization, 92.5% lower, OR 0.07, p < 0.001, high D levels (≥10ng/mL) 91, low D levels (<10ng/mL) 80, adjusted per study, inverted to make OR<1 favor high D levels (≥10ng/mL), case control OR, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Allami et al., 8 Nov 2022, retrospective, Iraq, peer-reviewed, 6 authors.
Contact: ahmed.suleiman@uoanbar.edu.iq.
The Risk of Up Normal Values of Two Parameters Obesity and Vitamin D in Incidence of Coronavirus Disease-19 Among Iraqi Patients
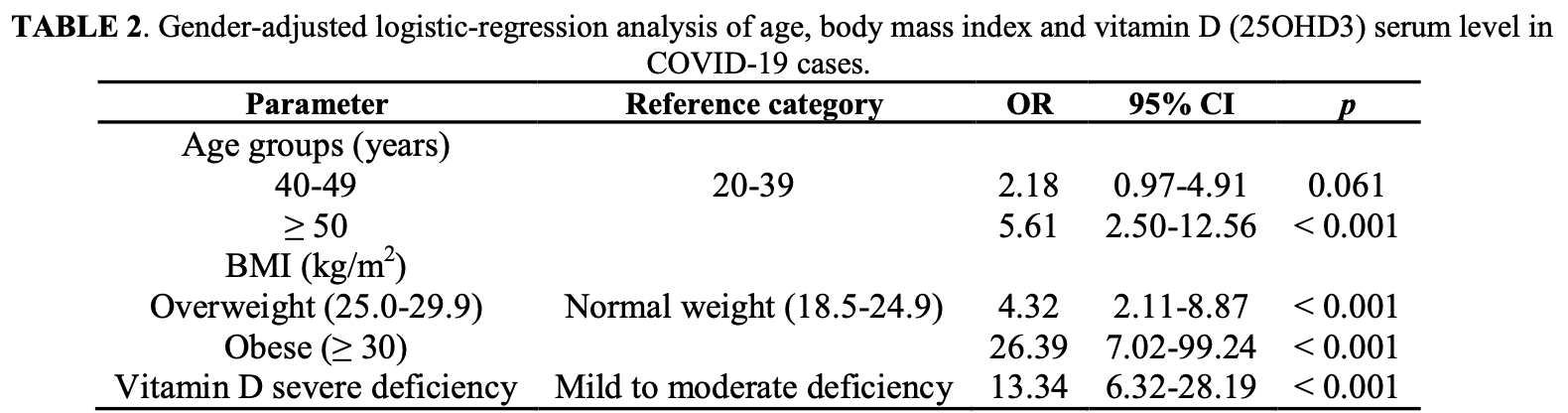
The new epidemic of coronavirus disease-19 outbreak has caused rapid morbidity and mortality rates worldwide, and health parameters have been proposed to influence disease progression. Among these parameters are index of body mass (BMI) and D vitamin. 86 patients with same number of control were studied( case-control) to find the relationship between the BMI, vitamin D and risk of COVID-19. Vitamin D (25-hydroxyvitamin D) serum level was estimated by ELISA. Results revealed that the age mean value was elevated significantly in cases compared to normal persons , and 50% of patients were 50 years of age or older. patients BMI were higher significantly in comparison with controls, and most of patients were overweight/obese (76.7%). The Vitamin D level decreased in patients significantly compared to control, and most of patients were severely-deficient (75.6%). Logistic-regression-analysis depicted a high risk of COVID-19 in obese cases (OR= 26.39; 95% interval of confidence [CI]: 7.02-99.24; p < 0.001), and in patients with severe deficient in vitamin D (OR = 13.34; 95% CI: 6.32-28.19; < 0.001). Moreover, overweight/obese patients severely deficient in vitamin D were at high risk of developing COVID-19 infection (OR = 230.55; 95% CI: 43.98-1208.67; p < 0.001). Curve analysis of ROC(Receiver-operating-characteristic) showed that BMI and vitamin D occupied under curve significant area (0.770 and 0.864, respectively). In conclusions, the study indicated that individuals who were overweight/obese and severely deficient in vitamin D were more susceptible to develop COVID-19.
References
Ali, None, J. Infect. Public Health, doi:10.1016/j.jiph.2020.06.021
Amiri, Behnezhad, Hasani, None, Obes. Med, doi:10.1016/j.obmed.2020.100196
Annweiler, Cao, Sabatier, None, Maturitas, doi:10.1016/j.maturitas.2020.06.003
De Heredia, Gómez-Martínez, Marcos, None, CUP
Ge, Wang, Yuan, Xiao, Wang et al., None, Eur. J. Clin. Microbiol. Infect. Dis, doi:10.1007/s10096-020-03874-z
Gombart, None, Future Microbiol
Hegde, Dhurandhar, None, Clin. Microbiol. Infect
Holick, None, Rev. Endocr. Metab. Disord, doi:10.1007/s11154-017-9424-1
Hussain, Mahawar, Xia, Yang, El-Hasani, None, Obes. Res. Clin. Pract, doi:10.1016/j.orcp.2020.07.002
Kennel, Drake, Hurley, None, Mayo Clin. Proc
Kościuczuk, Lisowski, Jarczak, Strzałkowska, Jóźwik et al., None, Mol. Biol. Rep
Lee, None, Best Pract. Res. Clin. Endocrinol. Metab, doi:10.1016/j.beem.2011.03.001
Lisowski, Jarczak, Strzałkowska, Jóźwik, Horbańczuk et al., None, Mol. Biol. Rep
Liu, Zhang, Li, Li, Zhou et al., None, J. Clin. Virol
Maresova, Javanmardi, Barakovic, Barakovic, Husic et al., None, BMC Public Health, doi:10.1186/s12889-019-7762-5
Montecino-Rodriguez, Berent-Maoz, Dorshkind, None, J. Clin. Invest
Muscogiuri, Pugliese, Barrea, Savastano, Colao, None, Metabolism, doi:10.1016/j.metabol.2020.154251
Nuttall, None, Nutr. Today, doi:10.1097/NT.0000000000000092
O'shea, Corrigan, Dunne, Jackson, Woods et al., None, Int. J. Obes, doi:10.1038/ijo.2013.16
Palacios, Gonzalez, None, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2013.11.003
Pan, Liu, Wang, Guo, Hao et al., None, JAMA -J. Am. Med. Assoc, doi:10.1001/jama.2020.6130
Peng, None, Biomed. Pharmacother, doi:10.1016/j.biopha.2020.110499
Prietl, Treiber, Pieber, Amrein, None, Nutrients, doi:10.3390/nu5072502
Quesada-Gomez, Castillo, Bouillon, None, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105719
Rojas-Osornio, Cruz-Hernández, Drago-Serrano, Campos-Rodríguez, None, Obes. Res. Clin. Pract, doi:10.1016/j.orcp.2019.05.003
Tamara, Tahapary, None, Diabetes Metab. Syndr. Clin. Res. Rev, doi:10.1016/j.dsx.2020.05.020
Wilder-Smith, Chiew, Lee, None, Lancet Infect. Dis, doi:10.1016/S1473-3099(20)30129-8
Yang, Liu, Zhang, Li, Li et al., None, J. Clin. Virol, doi:10.1016/j.jcv.2020.104475
Yegorov, Bromage, Boldbaatar, Ganmaa, None, Front. Nutr, doi:10.3389/fnut.2019.00166
DOI record:
{
"DOI": "10.1063/5.0121166",
"ISSN": [
"0094-243X"
],
"URL": "http://dx.doi.org/10.1063/5.0121166",
"author": [
{
"affiliation": [],
"family": "Allami",
"given": "Risala H.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Suleiman",
"given": "Ahmed A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mouhamad",
"given": "Raghad S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abdullah",
"given": "Maha H.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alsudani",
"given": "Mustafa Y.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Adhiah",
"given": "Ali H.",
"sequence": "additional"
}
],
"container-title": "1ST SAMARRA INTERNATIONAL CONFERENCE FOR PURE AND APPLIED SCIENCES (SICPS2021): SICPS2021",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
11,
9
]
],
"date-time": "2022-11-09T01:30:26Z",
"timestamp": 1667957426000
},
"deposited": {
"date-parts": [
[
2023,
4,
20
]
],
"date-time": "2023-04-20T01:58:33Z",
"timestamp": 1681955913000
},
"event": "1ST SAMARRA INTERNATIONAL CONFERENCE FOR PURE AND APPLIED SCIENCES (SICPS2021): SICPS2021",
"indexed": {
"date-parts": [
[
2023,
4,
20
]
],
"date-time": "2023-04-20T05:31:33Z",
"timestamp": 1681968693308
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022
]
]
},
"link": [
{
"URL": "http://aip.scitation.org/doi/pdf/10.1063/5.0121166",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "317",
"original-title": [],
"prefix": "10.1063",
"published": {
"date-parts": [
[
2022
]
]
},
"published-print": {
"date-parts": [
[
2022
]
]
},
"publisher": "AIP Publishing",
"reference": [
{
"DOI": "10.1016/j.jiph.2020.06.021",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c1"
},
{
"DOI": "10.1016/j.obmed.2020.100196",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c2"
},
{
"DOI": "10.1016/j.maturitas.2020.06.003",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c3"
},
{
"DOI": "10.1017/S0029665112000092",
"doi-asserted-by": "crossref",
"key": "10.1063/5.0121166_c4",
"unstructured": "F.P. De Heredia, S. Gómez-Martínez, A. Marcos. CUP. 332–338. (2012)."
},
{
"DOI": "10.1007/s10096-020-03874-z",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c5"
},
{
"key": "10.1063/5.0121166_c6",
"unstructured": "A.F. Gombart. Future Microbiol. (2009)."
},
{
"key": "10.1063/5.0121166_c7",
"unstructured": "V. Hegde, N. V. Dhurandhar. Clin. Microbiol. Infect. (2013)."
},
{
"DOI": "10.1007/s11154-017-9424-1",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c8"
},
{
"DOI": "10.1016/j.orcp.2020.07.002",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c9"
},
{
"key": "10.1063/5.0121166_c10",
"unstructured": "K.A. Kennel, M.T. Drake, D.L. Hurley. Mayo Clin. Proc. (2010)."
},
{
"key": "10.1063/5.0121166_c11",
"unstructured": "E.M. Kościuczuk, P.Lisowski, J. Jarczak, N. Strzałkowska, A. Jóźwik, J. Horbańczuk, J. Krzyżewski, L. Zwierzchowski, E. Bagnicka. Mol. Biol. Rep. (2012)."
},
{
"DOI": "10.1016/j.beem.2011.03.001",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c12"
},
{
"DOI": "10.1186/s12889-019-7762-5",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c13"
},
{
"key": "10.1063/5.0121166_c14",
"unstructured": "E. Montecino-Rodriguez, B. Berent-Maoz, K. Dorshkind. J. Clin. Invest. (2013)."
},
{
"DOI": "10.1016/j.metabol.2020.154251",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c15"
},
{
"DOI": "10.1097/NT.0000000000000092",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c16"
},
{
"key": "10.1063/5.0121166_c17",
"unstructured": "P.Lisowski, J. Jarczak, N. Strzałkowska, A. Jóźwik, J. Horbańczuk, J. Krzyżewski, L. Zwierzchowski, E. Bagnicka. Mol. Biol. Rep. (2013)."
},
{
"DOI": "10.1038/ijo.2013.16",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c18"
},
{
"DOI": "10.1016/j.jsbmb.2013.11.003",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c19"
},
{
"DOI": "10.1001/jama.2020.6130",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c20"
},
{
"DOI": "10.1016/j.biopha.2020.110499",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c21"
},
{
"DOI": "10.3390/nu5072502",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c22"
},
{
"DOI": "10.1016/j.jsbmb.2020.105719",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c23"
},
{
"DOI": "10.1016/j.orcp.2019.05.003",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c24"
},
{
"DOI": "10.1016/j.dsx.2020.05.020",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c25"
},
{
"key": "10.1063/5.0121166_c26",
"unstructured": "J. Liu, R. Zhang, M. Li, Z. Li, X. Zhou, C. Hu, F. Tian, F. Zhou, Y. Lei. J. Clin. Virol. 129. 104475. (2019)."
},
{
"DOI": "10.1016/S1473-3099(20)30129-8",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c27"
},
{
"DOI": "10.1016/j.jcv.2020.104475",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c28"
},
{
"DOI": "10.3389/fnut.2019.00166",
"doi-asserted-by": "publisher",
"key": "10.1063/5.0121166_c29"
}
],
"reference-count": 29,
"references-count": 29,
"relation": {},
"resource": {
"primary": {
"URL": "https://pubs.aip.org/aip/acp/article/2820933"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"title": "The risk of up normal values of two parameters obesity and vitamin D in incidence of coronavirus disease-19 among Iraqi patients",
"type": "proceedings-article"
}
