Correlates of poor clinical outcomes related to COVID-19 among older people with psychiatric illness - a mixed methods study
et al., The International Journal of Psychiatry in Medicine, doi:10.1177/00912174231171220, Apr 2023
Retrospective 81 pyschiatric inpatients in the UK, mean age 76, showing no significant difference in COVID-19 mortality with folate deficiency.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
Study covers vitamin B9 and vitamin D.
|
risk of death, 75.4% higher, OR 1.75, p = 0.63, high vitamin B9 levels (≥3ng/mL) 72, low vitamin B9 levels (<3ng/mL) 9, adjusted per study, inverted to make OR<1 favor high vitamin B9 levels (≥3ng/mL), multivariable, RR approximated with OR.
|
|
risk of progression, 44.8% lower, OR 0.55, p = 0.42, high vitamin B9 levels (≥3ng/mL) 72, low vitamin B9 levels (<3ng/mL) 9, adjusted per study, inverted to make OR<1 favor high vitamin B9 levels (≥3ng/mL), hospitalization, ICU, or death, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Abdulrahman et al., 17 Apr 2023, retrospective, United Kingdom, peer-reviewed, mean age 69.0, 7 authors, study period April 2020 - May 2021.
Contact: anto.rajamani@nottingham.ac.uk.
Correlates of poor clinical outcomes related to COVID-19 among older people with psychiatric illness - a mixed methods study
The International Journal of Psychiatry in Medicine, doi:10.1177/00912174231171220
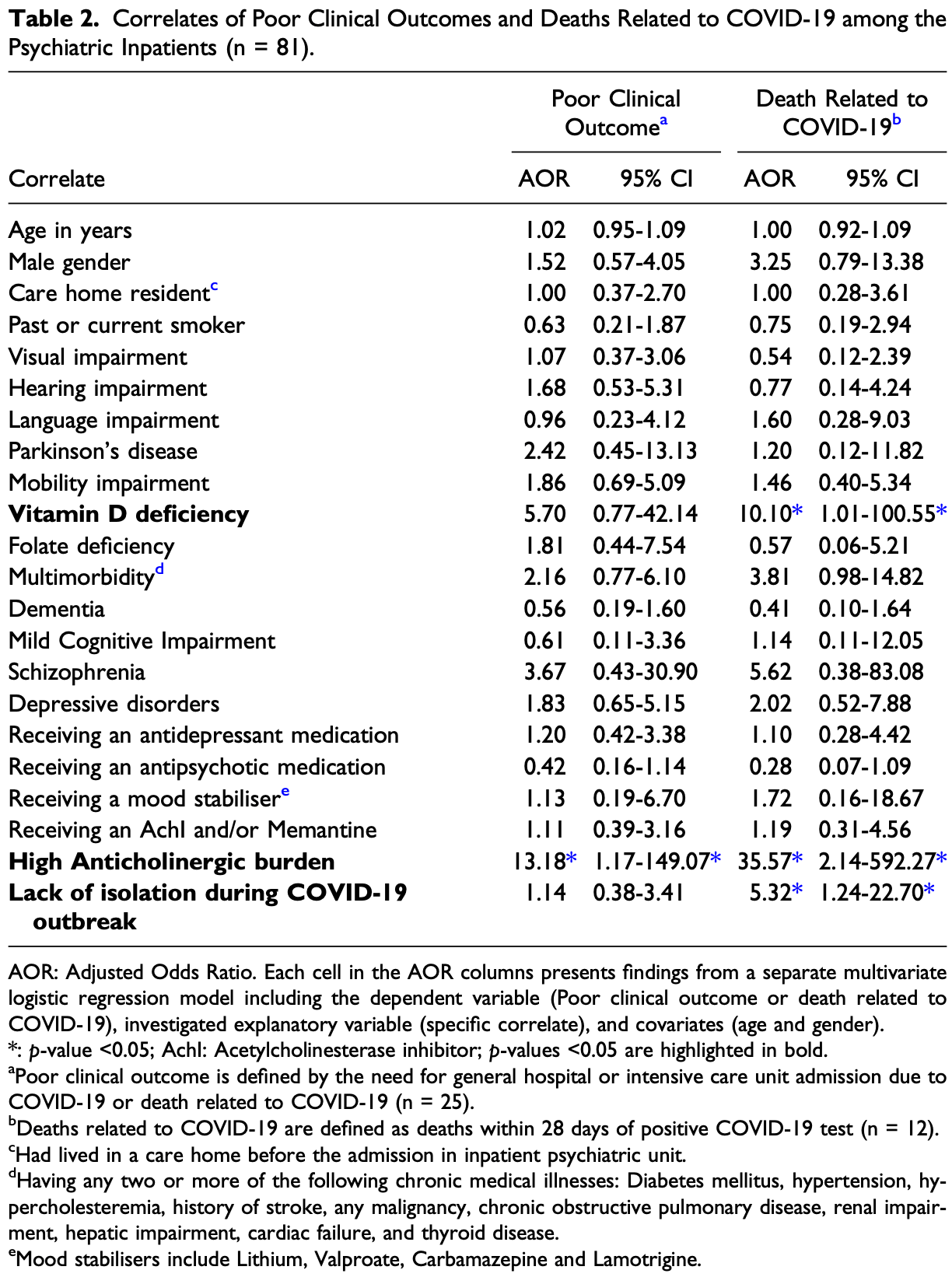
Objective: COVID-19 leads to highly variable clinical outcomes among older people with psychiatric and medical co-morbidities. Evidence guiding management of future outbreaks among this vulnerable population in in-patient psychiatry settings are sparse. Hence, we aimed to investigate the correlates of poor clinical outcomes related to COVID-19 and to explore the perspectives of COVID-19 survivors in in-patient psychiatry settings. Method: We investigated the correlates of poor clinical outcomes related to COVID-19 using retrospective chart review of 81 older people in in-patient psychiatry settings. Correlates of clinical outcomes related to COVID-19 were assessed by multiple logistic regression models. Moreover, we explored the perspectives of 10 of
Author contributions We confirm that all authors met the four ICMJE criteria for authorship. SD, BR and APR conceived this study, and APR wrote the study protocol. JHL, UK, SD, BR, and APR completed the retrospective chart review. SA completed the in-depth interviews. SA and APR transcribed the in-depth interviews. NA and APR analysed the retrospective chart review data. SA analysed the qualitative data. SA and NA wrote the initial manuscript. APR provided necessary supervision for SA and NA. All authors were involved in critical revisions of the manuscript and all authors have approved the final submitted version.
Declaration of conflicting interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval This research has obtained ethics approval from the London South-East Research Ethics Committee (20/LO/1282/133124/2020).
Informed consent Written informed consent was obtained from all participants before the in-depth interviews.
ORCID iDs Anto P Rajkumar https://orcid.org/0000-0003-3203-6326 Surajudeen Abdulrahman https://orcid.org/0000-0003-4445-1295
Supplemental Material Supplemental material for this article is available online.
References
Ashique, Gupta, Gupta, Vitamin D-A prominent immunomodulator to prevent COVID-19 infection, Int J Rheum Dis, doi:10.1111/1756-185X.14477
Bassatne, Basbous, Chakhtoura, El Zein, Fuleihan, The link between COVID-19 and vitamin D (VIVID): A systematic review and meta-analysis, Metabolism, doi:10.1016/j.metabol.2021.154753
Bishara, Scott, Stewart, Safe prescribing in cognitively vulnerable patients: The use of the anticholinergic effect on cognition (AEC) tool in older adult mental health services, BJPsych Bull, doi:10.1192/bjb.2019.43
Booth, Reed, Ponzo, Population risk factors for severe disease and mortality in COVID-19: A global systematic review and meta-analysis, PLoS One, doi:10.1371/journal.pone.0247461
Chatterjee, Carnahan, Chen, Holmes, Aparasu, Anticholinergic medication use and risk of pneumonia in elderly adults: A nested case-control study, J Am Geriatr Soc, doi:10.1111/jgs.13932
Docherty, Harrison, Green, Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: Prospective observational cohort study, BMJ, doi:10.1136/bmj.m1985
Fond, Pauly, Leone, Disparities in intensive care unit admission and mortality among patients with schizophrenia and COVID-19: A national cohort study, Schizophr Bull, doi:10.1093/schbul/sbaa158
Ghasemi, Darvishi, Salari, Hosseinian-Far, Akbari et al., Global prevalence of polypharmacy among the COVID-19 patients: A comprehensive systematic review and meta-analysis of observational studies, Trop Med Health, doi:10.1186/s41182-022-00456-x
Iloanusi, Mgbere, Essien, Polypharmacy among COVID-19 patients: A systematic review, J Am Pharm Assoc, doi:10.1016/j.japh.2021.05.006
Jick, Mixing qualitative and quantitative methods: Triangulation in action, Adm Sci Q
Kennedy, Helfand, Gou, Delirium in older patients with COVID-19 presenting to the emergency department, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.29540
Kiyumi, Kalra, Davies, Kalhan, The impact of Vitamin D deficiency on the severity of symptoms and mortality rate among adult patients with Covid-19: A systematic review and meta-analysis, Indian J Endocrinol Metab, doi:10.4103/ijem.ijem_115_21
Kummel, Krumbein, Fragkou, Vitamin D supplementation for the treatment of COVID-19: A systematic review and meta-analysis of randomized controlled trials, Front Immunol, doi:10.3389/fimmu.2022.1023903
Li, Huang, Zou, Epidemiology of COVID-19: A systematic review and metaanalysis of clinical characteristics, risk factors, and outcomes, J Med Virol, doi:10.1002/jmv.26424
Li, Li, Fortunati, Krystal, Association of a prior psychiatric diagnosis with mortality among hospitalized patients with coronavirus disease 2019 (COVID-19) infection, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.23282
Li, Liu, Jing, Mortality risk of COVID-19 in elderly males with comorbidities: A multi-country study, Aging, doi:10.18632/aging.202456
Li, Wang, Liu, Huang, Shi, Epidemiological characteristics of confirmed COVID-19 in Guizhou province, China, Disaster Med Public Health Prep, doi:10.1017/dmp.2020.134
Liu, Chen, Han, Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients, J Infect, doi:10.1016/j.jinf.2020.03.005
Liu, Sun, Wang, Zhang, Zhao et al., Low vitamin D status is associated with coronavirus disease 2019 outcomes: A systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.12.077
Lowry, Woodman, Soiza, Mangoni, Associations between the anticholinergic risk scale score and physical function: Potential implications for adverse outcomes in older hospitalized patients, J Am Med Dir Assoc, doi:10.1016/j.jamda.2011.03.006
Ma, Liu, Liu, Global percentage of asymptomatic SARS-CoV-2 infections among the tested population and individuals with confirmed COVID-19 diagnosis: A systematic review and meta-analysis, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.37257
Mehta, Bhandari, Raut, Kacimi, Huy, Coronavirus disease (COVID-19): Comprehensive review of clinical presentation, Front Public Health, doi:10.3389/fpubh.2020.582932
Saragih, Saragih, Batubara, Lin, Dementia as a mortality predictor among older adults with COVID-19: A systematic review and meta-analysis of observational study, Geriatr Nurs, doi:10.1016/j.gerinurse.2021.03.007
Schultze, Nightingale, Evans, Mortality among care home residents in England during the first and second waves of the COVID-19 pandemic: an observational study of 4.3 million adults over the age of 65, Lancet Reg Health Eur, doi:10.1016/j.lanepe.2021.100295
Serafini, Bondi, Locatelli, Amore, Aged patients with mental disorders in the COVID-19 Era: The experience of northern Italy, Am J Geriatr Psychiatry, doi:10.1016/j.jagp.2020.04.015
Shah, Varna, Sharma, Mavalankar, Does vitamin D supplementation reduce COVID-19 severity?: A systematic review, Qjm, doi:10.1093/qjmed/hcac040
Solis, Salas, Bartolome, Ballestín, The effects of vitamin D Supplementation in COVID-19 patients: A systematic review, Int J Mol Sci, doi:10.3390/ijms232012424
Taquet, Luciano, Geddes, Harrison, Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA, Lancet Psychiatry, doi:10.1016/S2215-0366(20)30462-4
Tehrani, Killander, Astrand, Jakobsson, Gille-Johnson, Risk factors for death in adult COVID-19 patients: Frailty predicts fatal outcome in older patients, Int J Infect Dis, doi:10.1016/j.ijid.2020.10.071
Teshome, Adane, Girma, Mekonnen, The impact of vitamin D level on COVID-19 infection: Systematic review and meta-analysis, Front Public Health, doi:10.3389/fpubh.2021.624559
Tilley, Walters, Shaykhiev, Rg, Cilia dysfunction in lung disease, Annu Rev Physio, doi:10.1146/annurev-physiol-021014-071931
Wang, Xu, Volkow, Increased risk of COVID-19 infection and mortality in people with mental disorders: Analysis from electronic health records in the United States, World Psychiatry, doi:10.1002/wps.20806
Wynants, Van Calster, Collins, Prediction models for diagnosis and prognosis of covid-19: Systematic review and critical appraisal, BMJ, doi:10.1136/bmj.m1328
Zheng, Peng, Xu, Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis, J Infect, doi:10.1016/j.jinf.2020.04.021
Zuin, Guasti, Roncon, Cervellati, Zuliani, Dementia and the risk of death in elderly patients with COVID-19 infection: Systematic review and meta-analysis, Int J Geriatr Psychiatry, doi:10.1002/gps.5468
DOI record:
{
"DOI": "10.1177/00912174231171220",
"ISSN": [
"0091-2174",
"1541-3527"
],
"URL": "http://dx.doi.org/10.1177/00912174231171220",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p> COVID-19 leads to highly variable clinical outcomes among older people with psychiatric and medical co-morbidities. Evidence guiding management of future outbreaks among this vulnerable population in in-patient psychiatry settings are sparse. Hence, we aimed to investigate the correlates of poor clinical outcomes related to COVID-19 and to explore the perspectives of COVID-19 survivors in in-patient psychiatry settings. </jats:p></jats:sec><jats:sec><jats:title>Method</jats:title><jats:p> We investigated the correlates of poor clinical outcomes related to COVID-19 using retrospective chart review of 81 older people in in-patient psychiatry settings. Correlates of clinical outcomes related to COVID-19 were assessed by multiple logistic regression models. Moreover, we explored the perspectives of 10 of those COVID-19 survivors by qualitative interviews. We analysed the qualitative data using thematic analysis. </jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p> Although 25.9% (n = 21) participants were asymptomatic, there was high COVID-19 related mortality rate (14.8%; n = 12). Vitamin-D deficiency, anticholinergic burden, and isolation policies within psychiatric wards were significantly ( P < 0.05) associated with COVID-19 related deaths. Participants emphasised the importance of strengthening local support networks and making vaccination centres more accessible. </jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p> Reducing anticholinergic prescriptions and improving isolation policies may mitigate poor clinical outcomes. Future research investigating the impact of vitamin-D supplementation on COVID-19 related outcomes are warranted. </jats:p></jats:sec>",
"alternative-id": [
"10.1177/00912174231171220"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-4445-1295",
"affiliation": [
{
"name": "Nottinghamshire Healthcare NHS Foundation trust, Nottingham, United Kingdom"
}
],
"authenticated-orcid": false,
"family": "Abdulrahman",
"given": "Surajudeen",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Nottinghamshire Healthcare NHS Foundation trust, Nottingham, United Kingdom"
},
{
"name": "Department of Behavioural Medicine, College of Medicine & Health Science, Sultan Qaboos University, Al Khod, Muscat, Sultanate of Oman"
}
],
"family": "Al-Balushi",
"given": "Naser",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nottinghamshire Healthcare NHS Foundation trust, Nottingham, United Kingdom"
}
],
"family": "Holdcroft-Long",
"given": "Jason",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nottinghamshire Healthcare NHS Foundation trust, Nottingham, United Kingdom"
}
],
"family": "Khan",
"given": "Uzma",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nottinghamshire Healthcare NHS Foundation trust, Nottingham, United Kingdom"
}
],
"family": "Ravindran",
"given": "Bipin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nottinghamshire Healthcare NHS Foundation trust, Nottingham, United Kingdom"
}
],
"family": "Das",
"given": "Sujata",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3203-6326",
"affiliation": [
{
"name": "Nottinghamshire Healthcare NHS Foundation trust, Nottingham, United Kingdom"
},
{
"name": "Institute of Mental Health, Mental Health and Clinical Neurosciences Academic Unit, University of Nottingham, Nottingham, United Kingdom"
}
],
"authenticated-orcid": false,
"family": "Rajkumar",
"given": "Anto P",
"sequence": "additional"
}
],
"container-title": "The International Journal of Psychiatry in Medicine",
"container-title-short": "Int J Psychiatry Med",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"journals.sagepub.com"
]
},
"created": {
"date-parts": [
[
2023,
4,
17
]
],
"date-time": "2023-04-17T19:42:16Z",
"timestamp": 1681760536000
},
"deposited": {
"date-parts": [
[
2023,
4,
17
]
],
"date-time": "2023-04-17T19:42:22Z",
"timestamp": 1681760542000
},
"funder": [
{
"name": "Nottinghamshire Healthcare NHS Foundation Trust"
}
],
"indexed": {
"date-parts": [
[
2023,
4,
18
]
],
"date-time": "2023-04-18T05:24:04Z",
"timestamp": 1681795444730
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
4,
17
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
17
]
],
"date-time": "2023-04-17T00:00:00Z",
"timestamp": 1681689600000
}
}
],
"link": [
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/00912174231171220",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/full-xml/10.1177/00912174231171220",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/00912174231171220",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "179",
"original-title": [],
"page": "009121742311712",
"prefix": "10.1177",
"published": {
"date-parts": [
[
2023,
4,
17
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
17
]
]
},
"publisher": "SAGE Publications",
"reference": [
{
"key": "bibr1-00912174231171220",
"unstructured": "WHO coronavirus (COVID-19) dashboard, https://covid19.who.int/ (2022)."
},
{
"key": "bibr2-00912174231171220",
"unstructured": "Deaths in United Kingdom, https://coronavirus.data.gov.uk/details/deaths (2022)."
},
{
"DOI": "10.1002/gps.5468",
"doi-asserted-by": "publisher",
"key": "bibr3-00912174231171220"
},
{
"DOI": "10.3389/fpubh.2020.582932",
"doi-asserted-by": "publisher",
"key": "bibr4-00912174231171220"
},
{
"DOI": "10.1016/j.ijid.2020.10.071",
"doi-asserted-by": "publisher",
"key": "bibr5-00912174231171220"
},
{
"DOI": "10.1017/dmp.2020.134",
"doi-asserted-by": "publisher",
"key": "bibr6-00912174231171220"
},
{
"DOI": "10.1016/j.jinf.2020.03.005",
"doi-asserted-by": "publisher",
"key": "bibr7-00912174231171220"
},
{
"key": "bibr8-00912174231171220",
"unstructured": "Coronavirus (COVID-19) latest insights: Infections, https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19latestinsights/infections (2022)."
},
{
"DOI": "10.1016/j.jinf.2020.04.021",
"doi-asserted-by": "publisher",
"key": "bibr9-00912174231171220"
},
{
"DOI": "10.1002/jmv.26424",
"doi-asserted-by": "publisher",
"key": "bibr10-00912174231171220"
},
{
"DOI": "10.1371/journal.pone.0247461",
"doi-asserted-by": "publisher",
"key": "bibr11-00912174231171220"
},
{
"DOI": "10.1136/bmj.m1328",
"doi-asserted-by": "publisher",
"key": "bibr12-00912174231171220"
},
{
"DOI": "10.1002/wps.20806",
"doi-asserted-by": "publisher",
"key": "bibr13-00912174231171220"
},
{
"DOI": "10.1001/jamanetworkopen.2020.23282",
"doi-asserted-by": "publisher",
"key": "bibr14-00912174231171220"
},
{
"DOI": "10.18632/aging.202456",
"doi-asserted-by": "publisher",
"key": "bibr15-00912174231171220"
},
{
"DOI": "10.1093/schbul/sbaa158",
"doi-asserted-by": "publisher",
"key": "bibr16-00912174231171220"
},
{
"DOI": "10.1016/S2215-0366(20)30462-4",
"doi-asserted-by": "publisher",
"key": "bibr17-00912174231171220"
},
{
"DOI": "10.1016/j.jagp.2020.04.015",
"doi-asserted-by": "publisher",
"key": "bibr18-00912174231171220"
},
{
"key": "bibr19-00912174231171220",
"unstructured": "Legal guidance for services supporting people of all ages during the coronavirus, https://www.england.nhs.uk/coronavirus/documents/c0175-legal-guidance-for-services-supporting-people-of-all-ages-during-the-coronavirus/ (2022)."
},
{
"key": "bibr20-00912174231171220",
"unstructured": "Coronavirus. 2022. Lessons learned to date report: Government response. https://www.gov.uk/government/publications/coronavirus-lessons-learned-to-date-report-government-response"
},
{
"DOI": "10.1192/bjb.2019.43",
"doi-asserted-by": "publisher",
"key": "bibr21-00912174231171220"
},
{
"DOI": "10.2307/2392366",
"doi-asserted-by": "publisher",
"key": "bibr22-00912174231171220"
},
{
"DOI": "10.1001/jamanetworkopen.2021.37257",
"doi-asserted-by": "publisher",
"key": "bibr23-00912174231171220"
},
{
"DOI": "10.1001/jamanetworkopen.2020.29540",
"doi-asserted-by": "publisher",
"key": "bibr24-00912174231171220"
},
{
"DOI": "10.1016/j.lanepe.2021.100295",
"doi-asserted-by": "publisher",
"key": "bibr25-00912174231171220"
},
{
"DOI": "10.1016/j.jamda.2011.03.006",
"doi-asserted-by": "publisher",
"key": "bibr26-00912174231171220"
},
{
"DOI": "10.1016/j.japh.2021.05.006",
"doi-asserted-by": "publisher",
"key": "bibr27-00912174231171220"
},
{
"DOI": "10.1186/s41182-022-00456-x",
"doi-asserted-by": "publisher",
"key": "bibr28-00912174231171220"
},
{
"DOI": "10.1146/annurev-physiol-021014-071931",
"doi-asserted-by": "publisher",
"key": "bibr29-00912174231171220"
},
{
"DOI": "10.1111/jgs.13932",
"doi-asserted-by": "publisher",
"key": "bibr30-00912174231171220"
},
{
"DOI": "10.1016/j.gerinurse.2021.03.007",
"doi-asserted-by": "publisher",
"key": "bibr31-00912174231171220"
},
{
"DOI": "10.1136/bmj.m1985",
"doi-asserted-by": "publisher",
"key": "bibr32-00912174231171220"
},
{
"DOI": "10.3389/fpubh.2021.624559",
"doi-asserted-by": "publisher",
"key": "bibr33-00912174231171220"
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"doi-asserted-by": "publisher",
"key": "bibr34-00912174231171220"
},
{
"DOI": "10.4103/ijem.ijem_115_21",
"doi-asserted-by": "publisher",
"key": "bibr35-00912174231171220"
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"doi-asserted-by": "publisher",
"key": "bibr36-00912174231171220"
},
{
"DOI": "10.1111/1756-185X.14477",
"doi-asserted-by": "publisher",
"key": "bibr37-00912174231171220"
},
{
"DOI": "10.1093/qjmed/hcac040",
"doi-asserted-by": "publisher",
"key": "bibr38-00912174231171220"
},
{
"DOI": "10.3389/fimmu.2022.1023903",
"doi-asserted-by": "publisher",
"key": "bibr39-00912174231171220"
},
{
"DOI": "10.3390/ijms232012424",
"doi-asserted-by": "publisher",
"key": "bibr40-00912174231171220"
}
],
"reference-count": 40,
"references-count": 40,
"relation": {},
"resource": {
"primary": {
"URL": "http://journals.sagepub.com/doi/10.1177/00912174231171220"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Psychiatry and Mental health"
],
"subtitle": [],
"title": "Correlates of poor clinical outcomes related to COVID-19 among older people with psychiatric illness - a mixed methods study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1177/sage-journals-update-policy"
}
abdulrahman3