Impact of Rapid Correction of Vitamin D Deficiency on Patients with COVID-19 Disease: A Randomized-Controlled Trial
et al., The Egyptian Journal of Hospital Medicine, doi:10.21608/EJHM.2024.368093, Jul 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
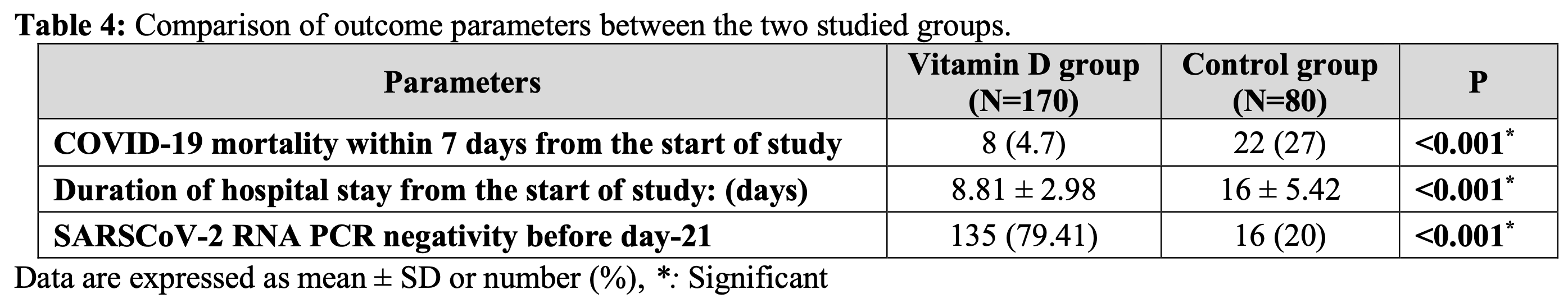
RCT 250 hospitalized COVID-19 patients showing significant clinical improvement with high-dose intramuscular vitamin D3 treatment. Patients receiving 200,000 IU cholecalciferol daily for 4 days had increased vitamin D levels, reduced inflammatory markers, higher oxygen saturation, shorter hospital stays, lower mortality, and improved viral clearance compared to controls receiving 10,000 IU oral vitamin D daily.
This is the 39th of 40 COVID-19 RCTs for vitamin D, which collectively show efficacy with p=0.0000001.
This is the 131st of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
|
risk of death, 82.9% lower, RR 0.17, p < 0.001, treatment 8 of 170 (4.7%), control 22 of 80 (27.5%), NNT 4.4.
|
|
hospitalization time, 44.9% lower, relative time 0.55, p < 0.001, treatment mean 8.81 (±2.98) n=170, control mean 16.0 (±5.42) n=80.
|
|
risk of no viral clearance, 74.3% lower, RR 0.26, p < 0.001, treatment 35 of 170 (20.6%), control 64 of 80 (80.0%), NNT 1.7.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Abdelhai et al., 15 Jul 2024, Randomized Controlled Trial, Egypt, peer-reviewed, 5 authors.
Impact of Rapid Correction of Vitamin D Deficiency on Patients with COVID-19 Disease: A Randomized-Controlled Trial
Background: Although antiviral properties of vitamin D are recognized, the influence of parental Vit D supplementation on COVID-19 disease has not been determined. Objective: The aim of study was to evaluate impact of prompt treatment of Vit D deficiency on COVID-19 patients. Patients and Methods: A randomized controlled experiment was carried out on 250 COVID-19 patients. Patients were categorized into two cohorts: one cohort received daily intramuscular injection of 200,000 IU cholecalciferol for four consecutive days, while other cohort received daily oral dose of 10,000 IU cholecalciferol. The latter group functioned as control group. Before and after therapy, serum 25(OH)D level, inflammatory markers and electrolytes were measured, besides, clinical follow-up. Results: In Vit D group, the 25(OH)D levels considerably increased after 7 days compared to initial levels (32.48 ±9.64 Vs 13.77 ±6.51 ng/mL, respectively). All Vit D deficient patients have transitioned to sufficient status. Levels of markers (ESR 50.99±17.56 mm/hr, CRP 30.75 ±24 mg/L, and ferritin 392.05 ±139.17 ng/mL) decreased after seven days (29.74±8.97 mm/hr, 10.52 ±13 mg/L, and 94.59 ±27.14 ng/mL, respectively). A substantial clinical improvement occurred in Vit D group compared to their initial condition. Also Vit D deficiency was found to significantly increase risk of COVID-19 mortality by factor of 15.375 [AOR = 15.375, 95% CI: 1.898-124.52, p=0.01].
Conclusion: A daily intramuscular injection of 200,000 IU cholecalciferol for four consecutive days has been proven to significantly enhance clinico-labarotaory parameters in COVID-19 patients. Considering higher Vit D supplementation as a potential treatment for COVID-19 is a viable option.
References
Amrein, Sourij, Wagner, Short-term effects of high-dose oral vitamin D3 in critically ill vitamin D deficient patients: a randomized, double-blind, placebocontrolled pilot study, Crit Care
Jakovac, COVID-19 and vitamin D-Is there a link and an opportunity for intervention?, Am J Physiol Endocrinol Metab
Kearns, Alvarez, Tangpricha, Large, single-dose, oral vitamin D supplementation in adult populations: a systematic review, Endocr Pract
Maghbooli, Sahraian, Ebrahimi, Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS One
Rastogi, Bhansali, Khare, Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study), Postgrad Med J
Tellioglu, Basaran, Guzel, Efficacy and safety of high dose intramuscular or oral cholecalciferol in vitamin D deficient/insufficient elderly, Maturitas
Velavan, Meyer, Mild versus severe COVID-19: Laboratory markers, Int J Infect Dis
Zdrenghea, Makrinioti, Bagacean, Vitamin D modulation of innate immune responses to respiratory viral infections, Rev Med Virol
