Relationship Between Dairy Intake and Hospitalization Risk and Disease Severity in Patients With COVID-19
et al., Clinical Nutrition Research, doi:10.7762/cnr.2023.12.4.283, Oct 2023
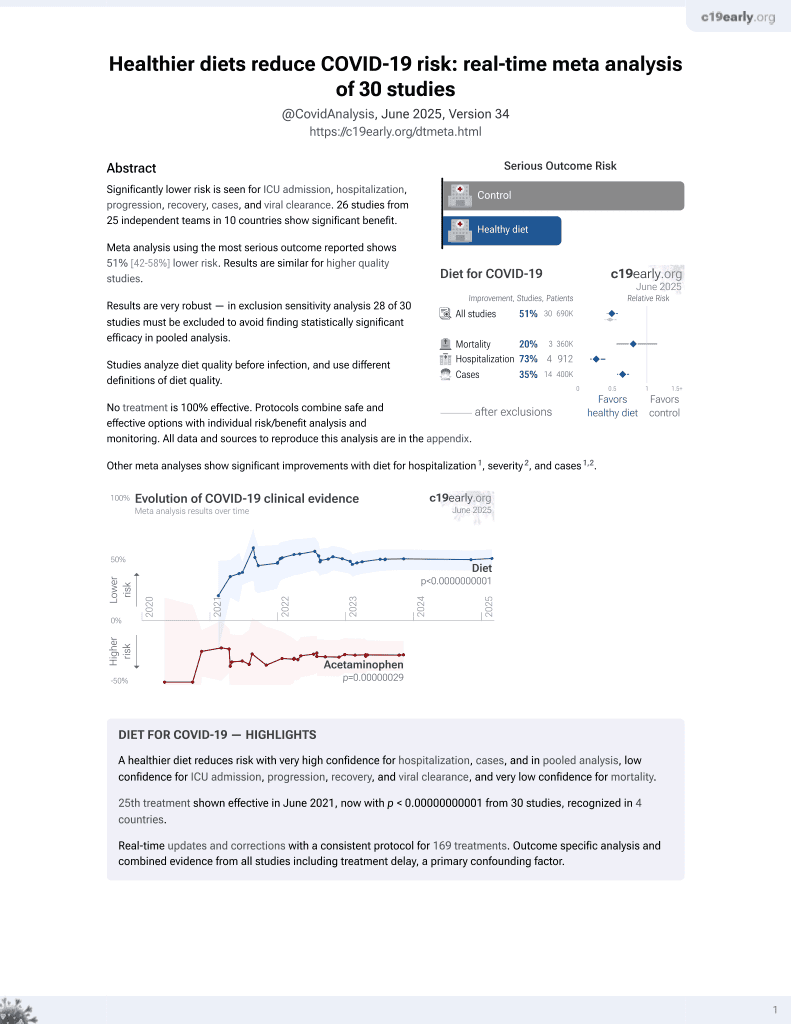
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 141 COVID-19 patients showing that higher dairy intake was associated with lower risk of hospitalization. The risk of hospitalization was 31% lower in the highest tertile of dairy intake compared to the lowest, after adjustment for confounders (p trend = 0.023). Dairy is a good source of several nutrients shown to be beneficial including vitamins A, B12, D, zinc, and probiotics.
|
risk of hospitalization, 31.0% lower, OR 0.69, p = 0.23, higher quality diet 48, lower quality diet 46, T3 vs. T1, model 3, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Abbas-Hashemi et al., 27 Oct 2023, retrospective, Iran, peer-reviewed, mean age 50.2, 10 authors.
Contact: zahrayari_nut@yahoo.com.
Relationship Between Dairy Intake and Hospitalization Risk and Disease Severity in Patients With COVID-19
Clinical Nutrition Research, doi:10.7762/cnr.2023.12.4.283
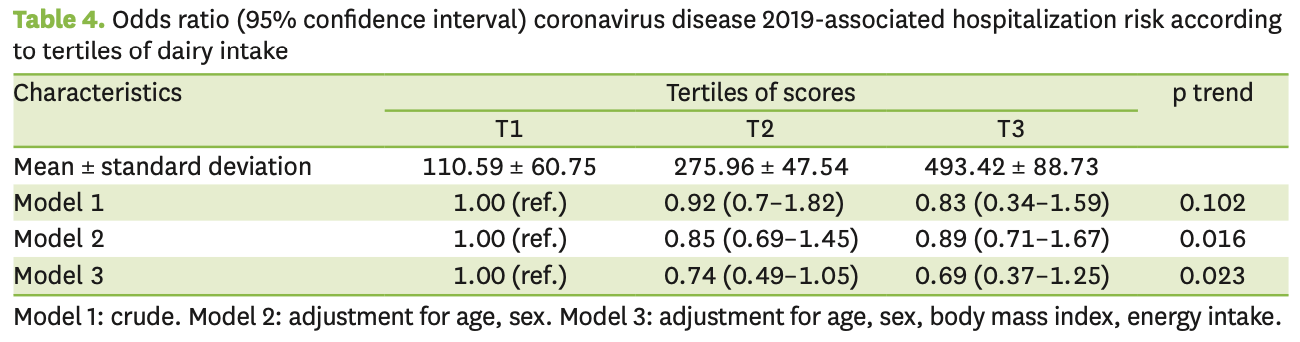
The aim of this study was to investigate whether dairy intake was associated with the severity of coronavirus disease 2019 (COVID-19) disease and the probability of hospitalization of patients. This cross-sectional study was conducted on 141 patients with COVID-19 with an average age of 46.23 ± 15.88 years. The number of men (52.5%) participating in this study was higher than that of women. The association between dairy intake and COVID-19 was evaluated by multivariable logistic regression analysis. The risk of hospitalization in the highest tertile of dairy intake was 31% lower than in the lowest tertile (odds ratio [OR], 0.69; 95% confidence interval [CI], 0.37-1.25, p trend = 0.023). Higher milk and yogurt intake was associated with a reduced risk of hospitalization due to COVID-19. Patients in the third tertiles were about 65% (p for trend = 0.014) and 12% (p for trend = 0.050) less likely to be hospitalized than those in the first tertile, respectively. Dairy consumption, especially low-fat ones, was associated with a lower risk of hospitalization due to COVID-19 and lower severity of COVID-19.
Conflict of Interest The authors declare that they have no competing interests.
Clinical parameters In this study, for measuring the height a wall-mounted stadiometer was used with 0.1 cm accuracy, also for weight measuring a digital scale with an accuracy of 0.1 kg was used. We calculate body mass index (BMI) by dividing weight (in kg) by height (in m 2 ). Biochemical parameters measured included white blood cells (WBCs), neutrophil-lymphocyte ratio (NLR), interleukin-6 (IL-6), and C-reactive protein (CRP). WBCs were measured by microscopy method with a BA310 microscope (MOTIC, Barcelona, Spain). Lymphocytes and neutrophils were assessed by Mindary BC-6800 and NLR was calculated accordingly. The enzyme-linked immunosorbent assay method was applied to measure IL-6 (Diaclone, Besançon, France) and CRP (Pars Azmoon Inc., Karaj, Iran).
Statistical analysis The data were analyzed by the Statistical Package for Social Sciences (version 20.0; SPSS Inc., Chicago, IL, USA). The level that was considered statistically significant was < 0.05. For assessing the normality of variables, the Kolmogorov-Smirnov analysis was used. Quantitative data were reported as mean ± standard deviation or median (25-75), interquartile range and qualitative data as a percentage. Linear regression analysis was applied to comparing the basic characteristics of participants based on dairy intake tertiles. Logistic regression was carried out to evaluate the odds ratios (ORs) and 95% confidence..
References
Abdulah, Hassan, Relation of dietary factors with infection and mortality rates of COVID-19 across the world, J Nutr Health Aging, doi:10.1007/s12603-020-1512-3
Alimohamadi, Sepandi, Taghdir, Hosamirudsari, Determine the most common clinical symptoms in COVID-19 patients: a systematic review and meta-analysis, J Prev Med Hyg, doi:10.15167/2421-4248/jpmh2020.61.3.1530
Batiha, Alqarni, Awad, Algammal, Nyamota et al., Dairy-derived and egg white proteins in enhancing immune system against COVID-19, Front Nutr, doi:10.3389/fnut.2021.629440
Brown-Riggs, Nutrition and health disparities: the role of dairy in improving minority health outcomes, Int J Environ Res Public Health, doi:10.3390/ijerph13010028
Calder, Carr, Gombart, Eggersdorfer, Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections, Nutrients, doi:10.3390/nu12041181
Calder, Nutrition and immunity: lessons for COVID-19, Nutr Diabetes, doi:10.1038/s41387-021-00165-0
Calder, Nutrition, immunity and COVID-19, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000085
Cena, Chieppa, Coronavirus disease (COVID-19-SARS-CoV-2) and nutrition: is infection in Italy suggesting a connection?, Front Immunol, doi:10.3389/fimmu.2020.00944
Chaari, Bendriss, Zakaria, Mcveigh, Importance of dietary changes during the coronavirus pandemic: how to upgrade your immune response, Front Public Health, doi:10.3389/fpubh.2020.00476
Childs, Calder, Miles, Diet and immune function, Nutrients, doi:10.3390/nu11081933
Cobre, Surek, Vilhena, Böger, Fachi et al., Influence of foods and nutrients on COVID-19 recovery: a multivariate analysis of data from 170 countries using a generalized linear model, Clin Nutr, doi:10.1016/j.clnu.2021.03.018
Darand, Hassanizadeh, Marzban, Mirzaei, Hosseinzadeh, The association between dairy products and the risk of COVID-19, Eur J Clin Nutr, doi:10.1038/s41430-022-01149-8
Emami, Javanmardi, Pirbonyeh, Akbari, Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis, Arch Acad Emerg Med
Fonseca, Rivas, Romaguera, Quijal, Czarlewski et al., Association between consumption of fermented vegetables and COVID-19 mortality at a country level in Europe. medRxiv. Forthcoming, doi:10.1101/2020.07.06.20147025
Ghazanfari, Salehi, Namaki, Arabkheradmand, Rostamian et al., Interpretation of hematological, biochemical, and immunological findings of COVID-19 disease: biomarkers associated with severity and mortality, Iran J Allergy Asthma Immunol, doi:10.18502/ijaai.v20i1.5412
Gombart, Pierre, Maggini, A review of micronutrients and the immune system-working in harmony to reduce the risk of infection, Nutrients, doi:10.3390/nu12010236
Gouda, Adbelruhman, Alenezi, Mégarbane, Theoretical benefits of yogurt-derived bioactive peptides and probiotics in COVID-19 patients -a narrative review and hypotheses, Saudi J Biol Sci, doi:10.1016/j.sjbs.2021.06.046
Huang, Liu, Qi, Brand, Zheng, Role of vitamin A in the Immune system, J Clin Med, doi:10.3390/jcm7090258
King, Glanville, Sanders, Fitzgerald, Varley, Effectiveness of probiotics on the duration of illness in healthy children and adults who develop common acute respiratory infectious conditions: a systematic review and meta-analysis, Br J Nutr, doi:10.1017/S0007114514000075
Ksiazek, Erdman, Goldsmith, Zaki, Peret et al., A novel coronavirus associated with severe acute respiratory syndrome, N Engl J Med, doi:10.1056/NEJMoa030781
Maggini, Pierre, Calder, Immune function and micronutrient requirements change over the life course, Nutrients, doi:10.3390/nu10101531
Mirmiran, Esfahani, Mehrabi, Hedayati, Azizi, Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study, Public Health Nutr, doi:10.1017/S1368980009991698
Mohseni, Amini, Abiri, Kalantar, Kaydani et al., Are history of dietary intake and food habits of patients with clinical symptoms of COVID 19 different from healthy controls? A case-control study, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2021.01.021
Morais, Aquino, Da Silva-Maia, Vale, Maciel et al., Nutritional status, diet and viral respiratory infections: perspectives for severe acute respiratory syndrome coronavirus 2, Br J Nutr, doi:10.1017/S0007114520003311
Prasad, Zinc in human health: effect of zinc on immune cells, Mol Med, doi:10.2119/2008-00033.Prasad
Reynolds, Roche, Conjugated linoleic acid and inflammatory cell signalling, Prostaglandins Leukot Essent Fatty Acids, doi:10.1016/j.plefa.2010.02.021
Seidelmann, Claggett, Cheng, Henglin, Shah et al., Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis, Lancet Public Health, doi:10.1016/S2468-2667(18)30135-X
Simonnet, Chetboun, Poissy, Raverdy, Noulette et al., LICORN and the Lille COVID-19 and Obesity study group. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obesity, doi:10.1002/oby.22831
Vouloumanou, Makris, Karageorgopoulos, Falagas, Probiotics for the prevention of respiratory tract infections: a systematic review, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2008.11.005
Yahfoufi, Alsadi, Jambi, Matar, The immunomodulatory and anti-inflammatory role of polyphenols, Nutrients, doi:10.3390/nu10111618
Yang, Zheng, Gou, Pu, Chen et al., Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.03.017
Yoshii, Hosomi, Sawane, Kunisawa, Metabolism of dietary and microbial vitamin B Family in the regulation of host immunity, Front Nutr, doi:10.3389/fnut.2019.00048
Young, Mine, Anti-inflammatory/oxidative stress proteins and peptides
DOI record:
{
"DOI": "10.7762/cnr.2023.12.4.283",
"ISSN": [
"2287-3732",
"2287-3740"
],
"URL": "http://dx.doi.org/10.7762/cnr.2023.12.4.283",
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"value": "2023-05-06"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Revised",
"name": "revised",
"value": "2023-09-16"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"value": "2023-09-24"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published online",
"name": "published_online",
"value": "2023-10-27"
},
{
"group": {
"label": "Copyright and Licensing",
"name": "Copyright_and_licensing"
},
"label": "Copyright",
"name": "copyright",
"value": "Copyright © 2023. The Korean Society of Clinical Nutrition"
},
{
"explanation": {
"URL": "https://creativecommons.org/licenses/by-nc/4.0/"
},
"group": {
"label": "Copyright and Licensing",
"name": "Copyright_and_licensing"
},
"label": "License",
"name": "license",
"value": "This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-8347-3625",
"affiliation": [
{
"name": "Department of Clinical Nutrition and Dietetics, Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Science, Tehran 1985717413, Iran."
}
],
"authenticated-orcid": false,
"family": "Abbas-Hashemi",
"given": "Seyed Ali",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-2796-2413",
"affiliation": [
{
"name": "Department of Nutrition Research, National Nutrition and Food Technology Research Institute and Faculty of Nutrition Sciences and Food Technology, Shahid Beheshti University of Medical Sciences, Tehran 1985717413, Iran."
}
],
"authenticated-orcid": false,
"family": "Yari",
"given": "Zahra",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1224-0234",
"affiliation": [
{
"name": "Department of Clinical Nutrition and Dietetics, Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Science, Tehran 1985717413, Iran."
}
],
"authenticated-orcid": false,
"family": "Soltanieh",
"given": "Samira",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1005-5649",
"affiliation": [
{
"name": "Department of Clinical Nutrition and Dietetics, Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Science, Tehran 1985717413, Iran."
}
],
"authenticated-orcid": false,
"family": "Salavatizadeh",
"given": "Marieh",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6874-2893",
"affiliation": [
{
"name": "Department of Clinical Nutrition and Dietetics, Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Science, Tehran 1985717413, Iran."
}
],
"authenticated-orcid": false,
"family": "Karimi",
"given": "Sara",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7023-9285",
"affiliation": [
{
"name": "Department of Immunology, Institute of Biochemistry and Biophysics, University of Tehran, Tehran 1417466191, Iran."
}
],
"authenticated-orcid": false,
"family": "Ardestani",
"given": "Sussan K.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2707-6027",
"affiliation": [
{
"name": "Department of Infectious Diseases, School of Medicine, Tehran University of Medical Sciences, Tehran 1417466191, Iran."
}
],
"authenticated-orcid": false,
"family": "Salehi",
"given": "Mohammadreza",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6696-6583",
"affiliation": [
{
"name": "Department of Clinical Nutrition and Dietetics, Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Science, Tehran 1985717413, Iran."
}
],
"authenticated-orcid": false,
"family": "Jahromi",
"given": "Soodeh Razeghi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1049-7095",
"affiliation": [
{
"name": "Department of Infectious Diseases, School of Medicine, Tehran University of Medical Sciences, Tehran 1417466191, Iran."
}
],
"authenticated-orcid": false,
"family": "Ghazanfari",
"given": "Tooba",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1944-0052",
"affiliation": [
{
"name": "Department of Clinical Nutrition and Dietetics, Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Science, Tehran 1985717413, Iran."
}
],
"authenticated-orcid": false,
"family": "Hekmatdoost",
"given": "Azita",
"sequence": "additional"
}
],
"container-title": "Clinical Nutrition Research",
"container-title-short": "Clin Nutr Res",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"e-cnr.org"
]
},
"created": {
"date-parts": [
[
2023,
11,
3
]
],
"date-time": "2023-11-03T07:24:46Z",
"timestamp": 1698996286000
},
"deposited": {
"date-parts": [
[
2023,
11,
3
]
],
"date-time": "2023-11-03T07:29:47Z",
"timestamp": 1698996587000
},
"indexed": {
"date-parts": [
[
2023,
11,
4
]
],
"date-time": "2023-11-04T00:48:36Z",
"timestamp": 1699058916807
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2023
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2023
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
1,
1
]
],
"date-time": "2023-01-01T00:00:00Z",
"timestamp": 1672531200000
}
}
],
"link": [
{
"URL": "https://e-cnr.org/pdf/10.7762/cnr.2023.12.4.283",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://e-cnr.org/DOIx.php?id=10.7762/cnr.2023.12.4.283",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://e-cnr.org/DOIx.php?id=10.7762/cnr.2023.12.4.283",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "18617",
"original-title": [],
"page": "283",
"prefix": "10.7762",
"published": {
"date-parts": [
[
2023
]
]
},
"published-online": {
"date-parts": [
[
2023
]
]
},
"publisher": "XMLink",
"reference": [
{
"DOI": "10.1056/NEJMoa030781",
"author": "Ksiazek",
"doi-asserted-by": "crossref",
"first-page": "1953",
"journal-title": "N Engl J Med",
"key": "10.7762/cnr.2023.12.4.283_ref1",
"volume": "348",
"year": "2003"
},
{
"author": "Alimohamadi",
"first-page": "E304",
"journal-title": "J Prev Med Hyg",
"key": "10.7762/cnr.2023.12.4.283_ref2",
"volume": "61",
"year": "2020"
},
{
"author": "Emami",
"first-page": "e35",
"journal-title": "Arch Acad Emerg Med",
"key": "10.7762/cnr.2023.12.4.283_ref3",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "91",
"journal-title": "Int J Infect Dis",
"key": "10.7762/cnr.2023.12.4.283_ref4",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1002/oby.22831",
"author": "Simonnet",
"doi-asserted-by": "crossref",
"first-page": "1195",
"journal-title": "Obesity (Silver Spring)",
"key": "10.7762/cnr.2023.12.4.283_ref5",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1038/s41387-021-00165-0",
"author": "Calder",
"doi-asserted-by": "crossref",
"first-page": "19",
"journal-title": "Nutr Diabetes",
"key": "10.7762/cnr.2023.12.4.283_ref6",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1017/S0007114520003311",
"author": "Morais",
"doi-asserted-by": "crossref",
"first-page": "851",
"journal-title": "Br J Nutr",
"key": "10.7762/cnr.2023.12.4.283_ref7",
"volume": "125",
"year": "2021"
},
{
"DOI": "10.3389/fpubh.2020.00476",
"author": "Chaari",
"doi-asserted-by": "crossref",
"first-page": "476",
"journal-title": "Front Public Health",
"key": "10.7762/cnr.2023.12.4.283_ref8",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.3390/nu10101531",
"author": "Maggini",
"doi-asserted-by": "crossref",
"first-page": "1531",
"journal-title": "Nutrients",
"key": "10.7762/cnr.2023.12.4.283_ref9",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.3390/nu12010236",
"author": "Gombart",
"doi-asserted-by": "crossref",
"first-page": "236",
"journal-title": "Nutrients",
"key": "10.7762/cnr.2023.12.4.283_ref10",
"volume": "12",
"year": "2020"
},
{
"author": "Fonseca",
"journal-title": "medRxiv",
"key": "10.7762/cnr.2023.12.4.283_ref11",
"year": "2020"
},
{
"DOI": "10.1016/j.sjbs.2021.06.046",
"author": "Gouda",
"doi-asserted-by": "crossref",
"first-page": "5897",
"journal-title": "Saudi J Biol Sci",
"key": "10.7762/cnr.2023.12.4.283_ref12",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.3390/ijerph13010028",
"author": "Brown-Riggs",
"doi-asserted-by": "crossref",
"first-page": "ijerph13010028",
"journal-title": "Int J Environ Res Public Health",
"key": "10.7762/cnr.2023.12.4.283_ref13",
"volume": "13",
"year": "2015"
},
{
"author": "Ghazanfari",
"first-page": "46",
"journal-title": "Iran J Allergy Asthma Immunol",
"key": "10.7762/cnr.2023.12.4.283_ref14",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1017/S1368980009991698",
"author": "Mirmiran",
"doi-asserted-by": "crossref",
"first-page": "654",
"journal-title": "Public Health Nutr",
"key": "10.7762/cnr.2023.12.4.283_ref15",
"volume": "13",
"year": "2010"
},
{
"DOI": "10.1038/s41430-022-01149-8",
"author": "Darand",
"doi-asserted-by": "crossref",
"first-page": "1583",
"journal-title": "Eur J Clin Nutr",
"key": "10.7762/cnr.2023.12.4.283_ref16",
"volume": "76",
"year": "2022"
},
{
"DOI": "10.1016/j.clnu.2021.03.018",
"author": "Cobre",
"doi-asserted-by": "crossref",
"first-page": "3077",
"journal-title": "Clin Nutr",
"key": "10.7762/cnr.2023.12.4.283_ref17",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.1016/j.clnesp.2021.01.021",
"author": "Mohseni",
"doi-asserted-by": "crossref",
"first-page": "280",
"journal-title": "Clin Nutr ESPEN",
"key": "10.7762/cnr.2023.12.4.283_ref18",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1007/s12603-020-1512-3",
"author": "Abdulah",
"doi-asserted-by": "crossref",
"first-page": "1011",
"journal-title": "J Nutr Health Aging",
"key": "10.7762/cnr.2023.12.4.283_ref19",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.3390/nu11081933",
"author": "Childs",
"doi-asserted-by": "crossref",
"first-page": "1933",
"journal-title": "Nutrients",
"key": "10.7762/cnr.2023.12.4.283_ref20",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.3390/nu12041181",
"author": "Calder",
"doi-asserted-by": "crossref",
"first-page": "1181",
"journal-title": "Nutrients",
"key": "10.7762/cnr.2023.12.4.283_ref21",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/S2468-2667(18)30135-X",
"author": "Seidelmann",
"doi-asserted-by": "crossref",
"first-page": "e419",
"journal-title": "Lancet Public Health",
"key": "10.7762/cnr.2023.12.4.283_ref22",
"volume": "3",
"year": "2018"
},
{
"DOI": "10.3389/fimmu.2020.00944",
"author": "Cena",
"doi-asserted-by": "crossref",
"first-page": "944",
"journal-title": "Front Immunol",
"key": "10.7762/cnr.2023.12.4.283_ref23",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3390/nu10111618",
"author": "Yahfoufi",
"doi-asserted-by": "crossref",
"first-page": "1618",
"journal-title": "Nutrients",
"key": "10.7762/cnr.2023.12.4.283_ref24",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.3390/jcm7090258",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "258",
"journal-title": "J Clin Med",
"key": "10.7762/cnr.2023.12.4.283_ref25",
"volume": "7",
"year": "2018"
},
{
"DOI": "10.3389/fnut.2019.00048",
"author": "Yoshii",
"doi-asserted-by": "crossref",
"first-page": "48",
"journal-title": "Front Nutr",
"key": "10.7762/cnr.2023.12.4.283_ref26",
"volume": "6",
"year": "2019"
},
{
"DOI": "10.2119/2008-00033.Prasad",
"author": "Prasad",
"doi-asserted-by": "crossref",
"first-page": "353",
"journal-title": "Mol Med",
"key": "10.7762/cnr.2023.12.4.283_ref27",
"volume": "14",
"year": "2008"
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"author": "Calder",
"doi-asserted-by": "crossref",
"first-page": "74",
"journal-title": "BMJ Nutr Prev Health",
"key": "10.7762/cnr.2023.12.4.283_ref28",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/j.ijantimicag.2008.11.005",
"author": "Vouloumanou",
"doi-asserted-by": "crossref",
"first-page": "197.e1",
"journal-title": "Int J Antimicrob Agents",
"key": "10.7762/cnr.2023.12.4.283_ref29",
"volume": "34",
"year": "2009"
},
{
"DOI": "10.1017/S0007114514000075",
"author": "King",
"doi-asserted-by": "crossref",
"first-page": "41",
"journal-title": "Br J Nutr",
"key": "10.7762/cnr.2023.12.4.283_ref30",
"volume": "112",
"year": "2014"
},
{
"DOI": "10.1016/j.plefa.2010.02.021",
"author": "Reynolds",
"doi-asserted-by": "crossref",
"first-page": "199",
"journal-title": "Prostaglandins Leukot Essent Fatty Acids",
"key": "10.7762/cnr.2023.12.4.283_ref31",
"volume": "82",
"year": "2010"
},
{
"DOI": "10.3389/fnut.2021.629440",
"author": "Batiha",
"doi-asserted-by": "crossref",
"first-page": "629440",
"journal-title": "Front Nutr",
"key": "10.7762/cnr.2023.12.4.283_ref32",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1002/9780813811048.ch2",
"author": "Young",
"doi-asserted-by": "crossref",
"first-page": "13",
"key": "10.7762/cnr.2023.12.4.283_ref33",
"volume-title": "Bioactive proteins and peptides as functional foods and nutraceuticals",
"year": "2010"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {},
"resource": {
"primary": {
"URL": "https://e-cnr.org/DOIx.php?id=10.7762/cnr.2023.12.4.283"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Earth and Planetary Sciences",
"General Environmental Science"
],
"subtitle": [],
"title": "Relationship Between Dairy Intake and Hospitalization Risk and Disease Severity in Patients With COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.7762/crossmark_policy",
"volume": "12"
}