Association of sleep quality before and after SARS-CoV-2 infection with clinical outcomes in hospitalized patients with COVID-19 in China
et al., EXCLI Journal, doi:10.17179/excli2021-3451, May 2021
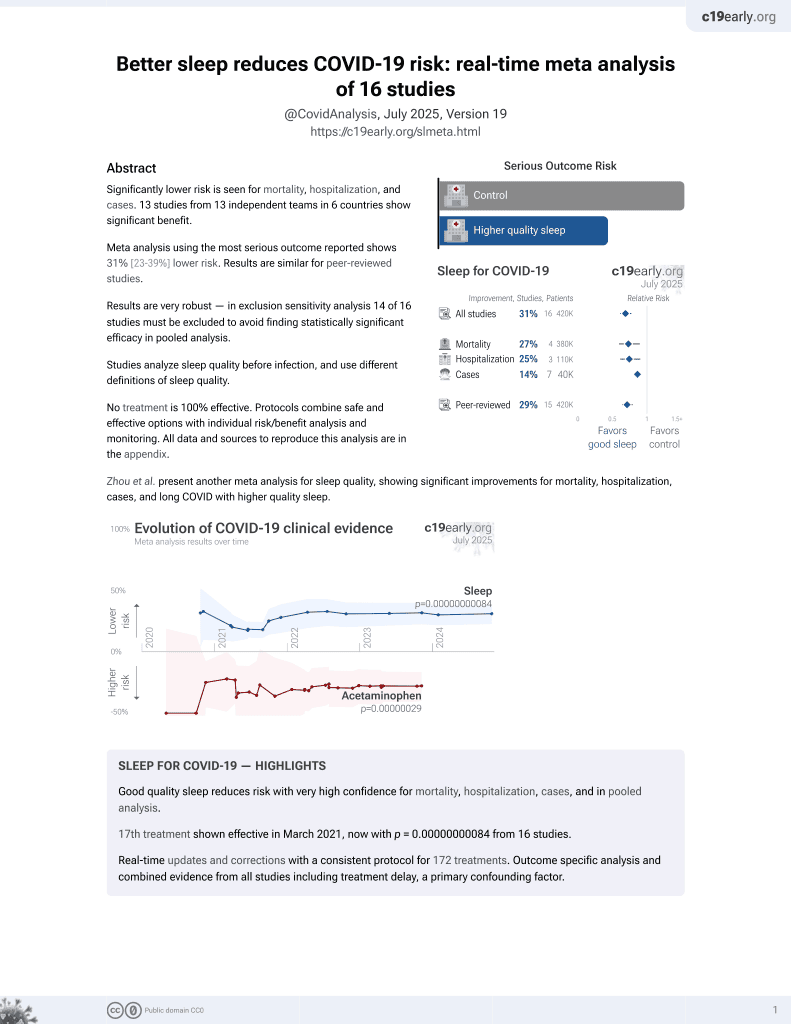
Sleep for COVID-19
18th treatment shown to reduce risk in
March 2021, now with p = 0.00000000084 from 16 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 205 hospitalized COVID-19 patients in China, showing higher risk of severe cases with poor sleep quality.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
This study is excluded in meta-analysis:
results only provided with respect to continuous values.
|
risk of severe case, 18.7% lower, HR 0.81, p < 0.001, inverted to make HR<1 favor improved sleep, global PQSI before infection, Cox proportional hazards, model 3.
|
|
risk of severe case, 25.9% lower, HR 0.74, p = 0.007, inverted to make HR<1 favor improved sleep, global PQSI after infection, Cox proportional hazards, model 3.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Zhang et al., 14 May 2021, prospective, China, peer-reviewed, survey, mean age 58.0, 15 authors, study period 6 January, 2020 - 9 March, 2020.
Contact: rongshuang@wust.edu.cn, wei-bao@uiowa.edu.
Original article: ASSOCIATION OF SLEEP QUALITY BEFORE AND AFTER SARS-COV-2 INFECTION WITH CLINICAL OUTCOMES IN HOSPITALIZED PATIENTS WITH COVID-19 IN CHINA
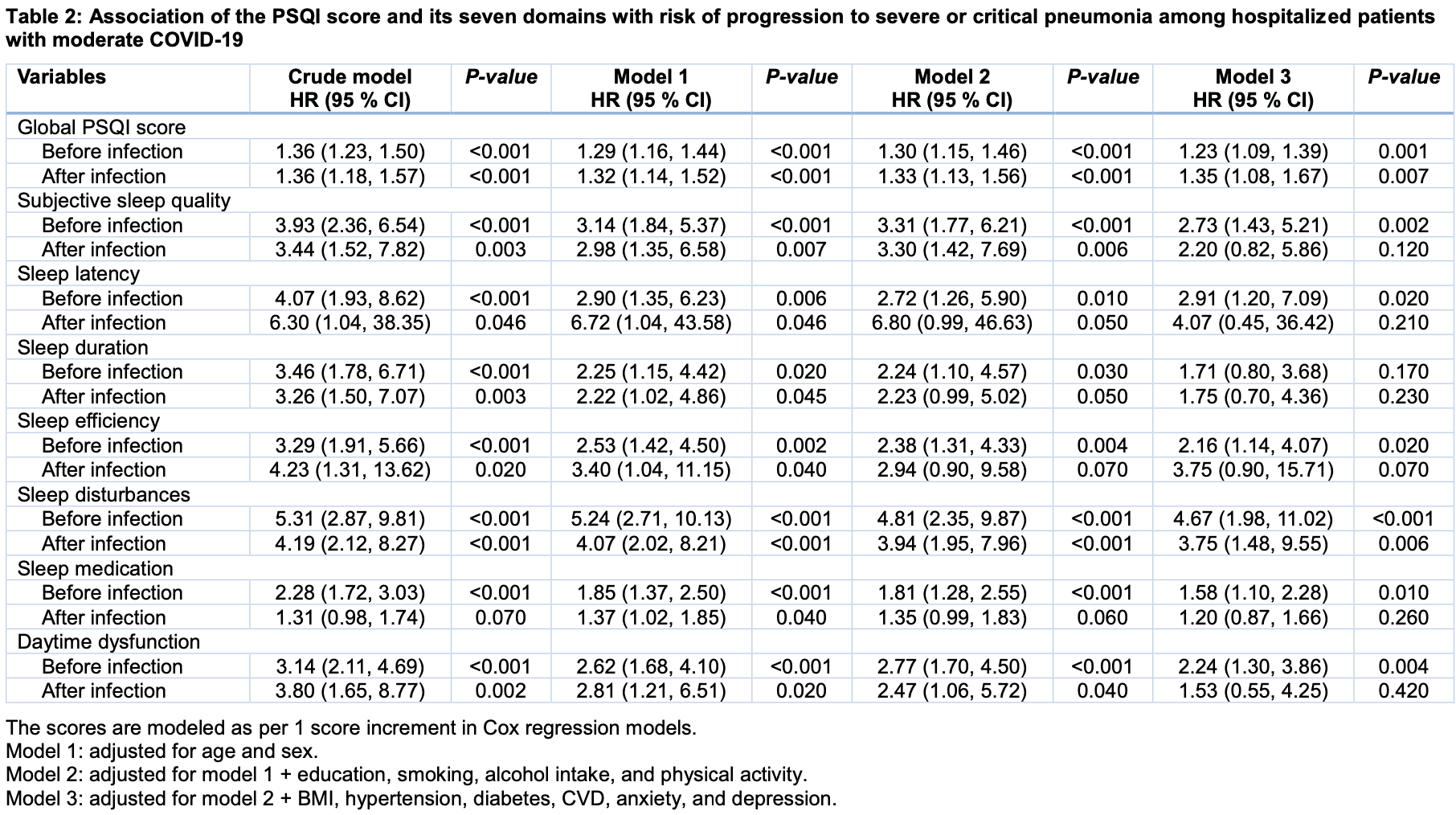
doi:10.17179/excli2021-3451
Sleep is believed to benefit the host defense against pathogens. We aimed to investigate the association of sleep quality with clinical outcomes among hospitalized patients with COVID-19. We conducted a prospective cohort study in 205 adult hospitalized patients with diagnosed moderate COVID-19, with follow-up until hospital discharge or death. Pittsburgh Sleep Quality Index (PSQI) assessed sleep quality before and after infection. The primary outcome was the incidence of severe or critical pneumonia, and the secondary outcomes were duration of hospital stay and laboratory measurements during the follow up. Among the 205 included hospitalized patients, 185 (90.2 %) experienced poorer sleep quality after infection than before according to the PSQI score, and 25 (12.2 %) developed severe or critical pneumonia during follow-up. In Cox regression models, the adjusted hazard ratio of developing severe or critical pneumonia associated with each 1 score increment in the PSQI score before and after infection was 1.23 (95% CI: 1.09, 1.39) and 1.35 (95 % CI: 1.08, 1.67), respectively. Poorer sleep quality was also significantly associated with a prolonged hospital stay and more serious dysregulations in immune system indicated by several laboratory markers. Poorer sleep quality, either in the daily time or after infection with SARS-CoV-2, was associated with worse clinical outcomes. These findings highlight the importance of good sleep in confronting the emerging pandemic of COVID-19.
Contributors SR, LZ, and WB designed research. LZ, FW, WX, MH, ZG, LS, HY, YZ, and YY contributed to the acquisition, analysis, or interpretation of the data. All authors contributed to critically revise the manuscript for important intellectual content. SR has primary responsibility for final content and is the study guarantor. All authors read and approved the final manuscript. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding No funding was received for the present study.
Competing interests The authors declare no conflict of interest.
References
Abell, Shipley, Ferrie, Kivimaki, Kumari, Recurrent short sleep, chronic insomnia symptoms and salivary cortisol: A 10-year follow-up in the Whitehall II study, Psychoneuroendocrinology
Akinci, Basar, Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19, Sleep Med
Buysse, Reynolds Cf 3rd, Monk, Berman, Kupfer et al., The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population, Psychiatry Res
Dobrosielski, Phan, Miller, Bohlen, Douglas-Burton et al., Associations between vasodilatory capacity, physical activity and sleep among younger and older adults, Eur J Appl Physiol
Gandhi, Lynch, Rio, Mild or moderate Covid-19, N Engl J Med
Hahn, Gunter, Schuhmacher, Bieber, Poschel et al., Reduced sleep in the week prior to diagnosis of COVID-19 is associated with the severity of COVID-19, Brain Behav Immun
Huang, Berube, Mcnamara, Saksena, Hartman et al., Lymphocyte subset counts in COVID-19 patients: A meta-analysis, Cytometry A
Irwin, Cole, Reciprocal regulation of the neural and innate immune systems, Nat Rev Immunol
Irwin, Sleep and inflammation: Partners in sickness and in health, Nat Rev Immunol
Irwin, Thompson, Miller, Gillin, Ziegler et al., Sleep disturbance, sleep duration, and inflammation: A systematic review and meta-analysis of cohort studies and experimental sleep deprivation, J Clin Endocrinol Metab
Jiang, Zhu, Wang, Hu, Pang et al., Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19, J Psychiatr Res
Kuo, Williams, Increased sleep promotes survival during a bacterial infection in Drosophila, Sleep
Liguori, Pierantozzi, Spanetta, Sarmati, Cesta et al., Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection, Brain Behav Immun
Loef, Van Der Beek, Hulsegge, Van Baarle, Proper, The mediating role of sleep, physical activity, and diet in the association between shift work and respiratory infections, Scand J Work Environ Health
Mollayeva, Thurairajah, Burton, Mollayeva, Shapiro et al., The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis, Sleep Med Rev
Patel, Malhotra, Gao, Hu, Neuman et al., A prospective study of sleep duration and pneumonia risk in women, Sleep
Perger, Soranna, Pengo, Meriggi, Lombardi et al., Sleep-disordered breathing among hospitalized patients with COVID-19, Am J Respir Crit Care Med
Prather, Janicki-Deverts, Hall, Cohen, Behaviorally assessed sleep and susceptibility to the common cold, Sleep
Prather, Leung, Association of insufficient sleep with respiratory infection among adults in the United States, JAMA Intern Med
Qin, Zhou, Hu, Zhang, Yang et al., Negative impact of COVID-19 pandemic on sleep quantitative parameters, quality, and circadian alignment: Implications for health and psychological well-being, Clin Infect Dis
Webster, Oakley, Jewell, Cidlowski, Proinflammatory cytokines regulate human glucocorticoid receptor gene expression and lead to the accumulation of the dominant negative beta isoform: a mechanism for the generation of glucocorticoid resistance
Wu, Mcgoogan, Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention, JAMA
Yang, Yu, Xu, Shu, Ja et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study, Lancet Respir Med
Zhu, Zhang, Li, Yang, Song, A novel coronavirus from patients with pneumonia in China, 2019, N Engl J Med
Zigmond, Snaith, The hospital anxiety and depression scale, Acta Psychiatr Scand
DOI record:
{
"DOI": "10.17179/EXCLI2021-3451",
"URL": "https://www.excli.de/index.php/excli/article/view/3451",
"abstract": "Sleep is believed to benefit the host defense against pathogens. We aimed to investigate the association of sleep quality with clinical outcomes among hospitalized patients with COVID-19. We conducted a prospective cohort study in 205 adult hospitalized patients with diagnosed moderate COVID-19, with follow-up until hospital discharge or death. Pittsburgh Sleep Quality Index (PSQI) assessed sleep quality before and after infection. The primary outcome was the incidence of severe or critical pneumonia, and the secondary outcomes were duration of hospital stay and laboratory measurements during the follow up. Among the 205 included hospitalized patients, 185 (90.2 %) experienced poorer sleep quality after infection than before according to the PSQI score, and 25 (12.2 %) developed severe or critical pneumonia during follow-up. In Cox regression models, the adjusted hazard ratio of developing severe or critical pneumonia associated with each 1 score increment in the PSQI score before and after infection was 1.23 (95% CI: 1.09, 1.39) and 1.35 (95 % CI: 1.08, 1.67), respectively. Poorer sleep quality was also significantly associated with a prolonged hospital stay and more serious dysregulations in immune system indicated by several laboratory markers. Poorer sleep quality, either in the daily time or after infection with SARS-CoV-2, was associated with worse clinical outcomes. These findings highlight the importance of good sleep in confronting the emerging pandemic of COVID-19.",
"author": [
{
"family": "Zhang",
"given": "Li"
},
{
"family": "Li",
"given": "Tingting"
},
{
"family": "Chen",
"given": "Liangkai"
},
{
"family": "Wu",
"given": "Feng"
},
{
"family": "Xia",
"given": "Wenguang"
},
{
"family": "Huang",
"given": "Min"
},
{
"family": "Guo",
"given": "Zhenli"
},
{
"family": "Song",
"given": "Lin"
},
{
"family": "Yin",
"given": "Hongxiang"
},
{
"family": "Zhang",
"given": "Yangpu"
},
{
"family": "Yu",
"given": "Yongfei"
},
{
"family": "Cai",
"given": "Sijie"
},
{
"family": "Lu",
"given": "Zijian"
},
{
"family": "Rong",
"given": "Shuang"
},
{
"family": "Bao",
"given": "Wei"
}
],
"categories": [
"Coronavirus disease 2019",
"SARS-CoV-2",
"sleep",
"epidemiology"
],
"container-title": "EXCLI Journal; 20:Doc894; ISSN 1611-2156",
"copyright": "This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0).",
"id": "https://doi.org/10.17179/excli2021-3451",
"issued": {
"date-parts": [
[
2021
]
]
},
"language": "en",
"publisher": "IfADo - Leibniz Research Centre for Working Environment and Human Factors, Dortmund",
"title": "Association of sleep quality before and after SARS-CoV-2 infection with clinical outcomes in hospitalized patients with COVID-19 in China",
"type": "article-journal"
}