Ethnicity and risks of severe COVID-19 outcomes associated with glucose-lowering medications: A cohort study
et al., Diabetes, Obesity and Metabolism, doi:10.1111/dom.14872, Sep 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
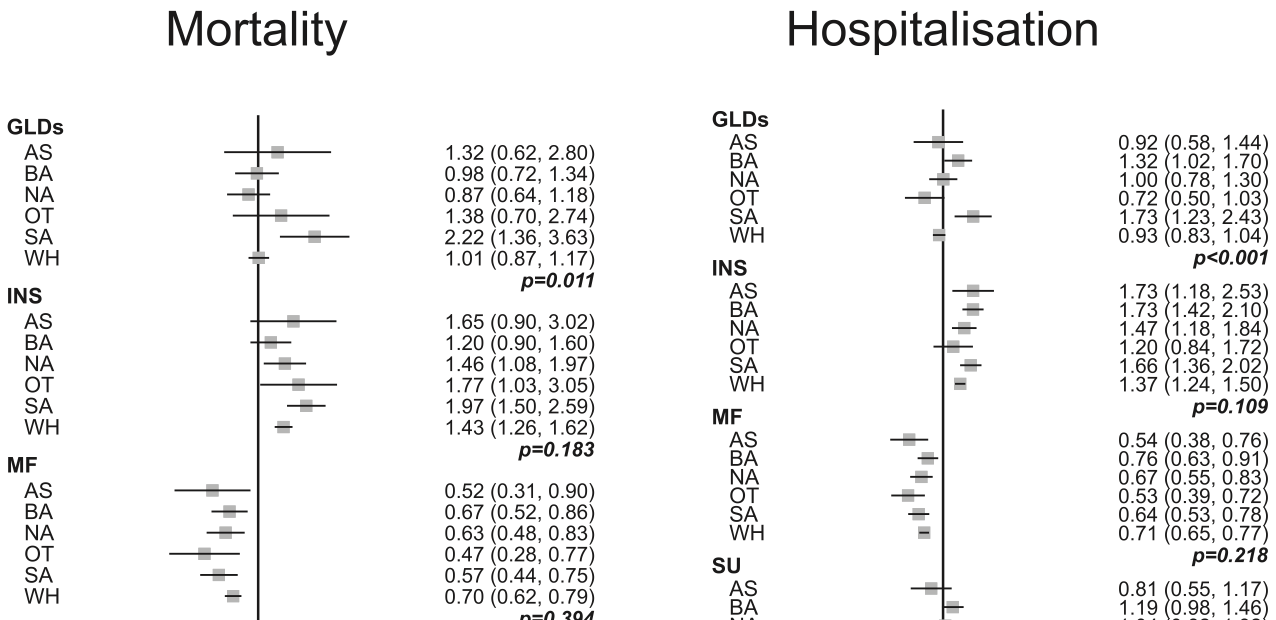
Retrospective 624,771 people with type 2 diabetes in the UK, showing lower COVID-19 mortality and hospitalization with metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 34.3% lower, RR 0.66, p < 0.001, meta analysis of 6 groups reported.
|
|
risk of hospitalization, 31.2% lower, RR 0.69, p < 0.001, meta analysis of 6 groups reported.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Zaccardi et al., 13 Sep 2022, retrospective, United Kingdom, peer-reviewed, 11 authors.
Contact: frazac@fastwebnet.it.
Abstract: Revised: 31 August 2022
Accepted: 10 September 2022
DOI: 10.1111/dom.14872
RESEARCH LETTER
Ethnicity and risks of severe COVID-19 outcomes associated
with glucose-lowering medications: A cohort study
Francesco Zaccardi PhD 1
|
Pui San Tan PhD 2
4
| Ash Kieran Clift MBBS
Baiju R. Shah PhD
2
Martina Patone PhD
| Simon J. Griffin DM 6,7
Kamlesh Khunti PhD 1
| Carol Coupland PhD 2,3
2,5
|
2
| Defne Saatci MBBS
|
| Hajira Dambha-Miller PhD 8 |
| Julia Hippisley-Cox FRCP 2
1
Leicester Real World Evidence Unit, Leicester Diabetes Centre, University of Leicester, Leicester, UK
2
Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, UK
3
Division of Primary Care, School of Medicine, University of Nottingham, Nottingham, UK
4
Department of Medicine, University of Toronto; Division of Endocrinology, Sunnybrook Health Sciences Centre, Institute for Clinical Evaluative Sciences, Toronto,
Ontario, Canada
5
Cancer Research UK Oxford Centre, University of Oxford, Oxford, UK
6
Primary Care Unit, School of Clinical Medicine, University of Cambridge, Cambridge, UK
7
MRC Epidemiology Unit, School of Clinical Medicine, University of Cambridge, Cambridge, UK
8
Primary Care Research Centre, University of Southampton, Southampton, UK
Correspondence
Francesco Zaccardi, Leicester Real World Evidence Unit, Diabetes Research Centre, Leicester General Hospital Gwendolen Road, Leicester, LE5 4PW, UK.
Email: frazac@fastwebnet.it
Funding information
National Insitute for Health and Care Research (NIHR), Grant/Award Number: COV0130 /MR/V027778/1; UK Research and Innovation; Academic Clinical Lecturer;
Leicester Biomedical Research Centre (BRC), Grant/Award Number: NIHR200171; Applied Research Collaboration East Midlands (ARC EM); Cancer Research UK
Oxford Centre, and the Oxford Wellcome Institutional, Grant/Award Number: 204826/Z/16/Z; National Institute for Health Research, Oxford, John Fell Oxford
University Press Research Fund, Cancer Research UK, Grant/Award Number: C5255/A18085; Clinical Research Fellowship from Cancer Research UK, Grant/Award
Number: C2195/A31310; MRC Epidemiology Unit programme, Grant/Award Number: MC_UU_12015/4
1
|
I N T RO DU CT I O N
[metformin (MF), sodium-glucose cotransporter-2 inhibitors (SGLT-2i),
sulphonylurea].5
During the early phases of the COVID-19 pandemic, diabetes became
Alongside the role of diabetes, multiple large observational stud-
associated with a poorer prognosis,1 with an approximately three-fold
ies also showed higher risks of COVID-19-related hospitalization,
increased risk of a COVID-19 death in those with diabetes compared
intensive care unit admission and death in people from ethnic minor-
with those without.2,3 In an effort to understand this association,
ity populations.6,7
there was an increasing interest in the role of glucose-lowering medi-
As type 2 diabetes is more prevalent in ethnic minority
cations on the risk of COVID-19 outcomes, given their pharmacologi-
populations—particularly South Asians—determining the risk of COVID-
cal differences and potential direct effect on shared immunometabolic
19 outcomes in relation to different glucose-lowering therapies has impli-
pathways4: the available evidence would suggest small absolute
cations for both patients and health care professionals.8 We therefore
increased rates of COVID-19 mortality with some dipeptidyl pepti-
designed a cohort study within the QResearch UK nationwide..
DOI record:
{
"DOI": "10.1111/dom.14872",
"ISSN": [
"1462-8902",
"1463-1326"
],
"URL": "http://dx.doi.org/10.1111/dom.14872",
"alternative-id": [
"10.1111/dom.14872"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2022-06-15"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2022-09-10"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2022-09-29"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-2636-6487",
"affiliation": [
{
"name": "Leicester Real World Evidence Unit, Leicester Diabetes Centre University of Leicester Leicester UK"
}
],
"authenticated-orcid": false,
"family": "Zaccardi",
"given": "Francesco",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Nuffield Department of Primary Care Health Sciences University of Oxford Oxford UK"
}
],
"family": "Tan",
"given": "Pui San",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nuffield Department of Primary Care Health Sciences University of Oxford Oxford UK"
},
{
"name": "Division of Primary Care, School of Medicine University of Nottingham Nottingham UK"
}
],
"family": "Coupland",
"given": "Carol",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3598-3628",
"affiliation": [
{
"name": "Department of Medicine, University of Toronto; Division of Endocrinology, Sunnybrook Health Sciences Centre Institute for Clinical Evaluative Sciences Toronto Ontario Canada"
}
],
"authenticated-orcid": false,
"family": "Shah",
"given": "Baiju R.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nuffield Department of Primary Care Health Sciences University of Oxford Oxford UK"
},
{
"name": "Cancer Research UK Oxford Centre University of Oxford Oxford UK"
}
],
"family": "Clift",
"given": "Ash Kieran",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nuffield Department of Primary Care Health Sciences University of Oxford Oxford UK"
}
],
"family": "Saatci",
"given": "Defne",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nuffield Department of Primary Care Health Sciences University of Oxford Oxford UK"
}
],
"family": "Patone",
"given": "Martina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Primary Care Unit, School of Clinical Medicine University of Cambridge Cambridge UK"
},
{
"name": "MRC Epidemiology Unit, School of Clinical Medicine University of Cambridge Cambridge UK"
}
],
"family": "Griffin",
"given": "Simon J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Primary Care Research Centre University of Southampton Southampton UK"
}
],
"family": "Dambha‐Miller",
"given": "Hajira",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2343-7099",
"affiliation": [
{
"name": "Leicester Real World Evidence Unit, Leicester Diabetes Centre University of Leicester Leicester UK"
}
],
"authenticated-orcid": false,
"family": "Khunti",
"given": "Kamlesh",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nuffield Department of Primary Care Health Sciences University of Oxford Oxford UK"
}
],
"family": "Hippisley‐Cox",
"given": "Julia",
"sequence": "additional"
}
],
"container-title": "Diabetes, Obesity and Metabolism",
"container-title-short": "Diabetes Obesity Metabolism",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2022,
9,
13
]
],
"date-time": "2022-09-13T15:59:34Z",
"timestamp": 1663084774000
},
"deposited": {
"date-parts": [
[
2022,
9,
30
]
],
"date-time": "2022-09-30T06:29:04Z",
"timestamp": 1664519344000
},
"funder": [
{
"DOI": "10.13039/100014013",
"doi-asserted-by": "publisher",
"name": "UK Research and Innovation"
}
],
"indexed": {
"date-parts": [
[
2022,
10,
1
]
],
"date-time": "2022-10-01T05:22:20Z",
"timestamp": 1664601740466
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
9,
29
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
9,
29
]
],
"date-time": "2022-09-29T00:00:00Z",
"timestamp": 1664409600000
}
},
{
"URL": "http://doi.wiley.com/10.1002/tdm_license_1.1",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
9,
29
]
],
"date-time": "2022-09-29T00:00:00Z",
"timestamp": 1664409600000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1111/dom.14872",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/full-xml/10.1111/dom.14872",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1111/dom.14872",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"prefix": "10.1111",
"published": {
"date-parts": [
[
2022,
9,
29
]
]
},
"published-online": {
"date-parts": [
[
2022,
9,
29
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1111/dom.14124",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_2_1"
},
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_3_1"
},
{
"DOI": "10.1111/dom.14105",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_4_1"
},
{
"DOI": "10.1016/j.cmet.2021.01.016",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_5_1"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_6_1"
},
{
"DOI": "10.1007/s10654-021-00765-1",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_7_1"
},
{
"DOI": "10.1016/S0140-6736(21)00634-6",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_8_1"
},
{
"DOI": "10.1111/dme.13895",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_9_1"
},
{
"DOI": "10.1016/S2213-8587(20)30152-2",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_10_1"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_11_1"
},
{
"DOI": "10.3389/fendo.2021.794382",
"article-title": "A randomized clinical trial of Linagliptin vs. standard of Care in Patients Hospitalized with Diabetes and COVID‐19",
"author": "Abuhasira R",
"doi-asserted-by": "crossref",
"first-page": "794382",
"journal-title": "Front Endocrinol (Lausanne)",
"key": "e_1_2_11_12_1",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(21)00180-7",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_13_1"
},
{
"DOI": "10.1136/bmj.o298",
"article-title": "What do we know about covid vaccines and preventing transmission?",
"author": "Stokel‐Walker C",
"doi-asserted-by": "crossref",
"first-page": "o298",
"journal-title": "BMJ",
"key": "e_1_2_11_14_1",
"volume": "376",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0212117",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_15_1"
},
{
"DOI": "10.1111/dom.12824",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_16_1"
},
{
"DOI": "10.1111/dom.12849",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_17_1"
},
{
"DOI": "10.1111/dom.14008",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_18_1"
},
{
"DOI": "10.1111/dom.12101",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_19_1"
},
{
"DOI": "10.1111/dom.12670",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_20_1"
}
],
"reference-count": 19,
"references-count": 19,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1111/dom.14872"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": "Ethnicity and risks of severe\n <scp>COVID</scp>\n ‐19 outcomes associated with glucose‐lowering medications: A cohort study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy"
}
