Decreased Serum Selenium Levels of COVID-19 Patients in Comparison with Healthy Individuals
et al., Biological Trace Element Research, doi:10.1007/s12011-021-02797-w, Jul 2021
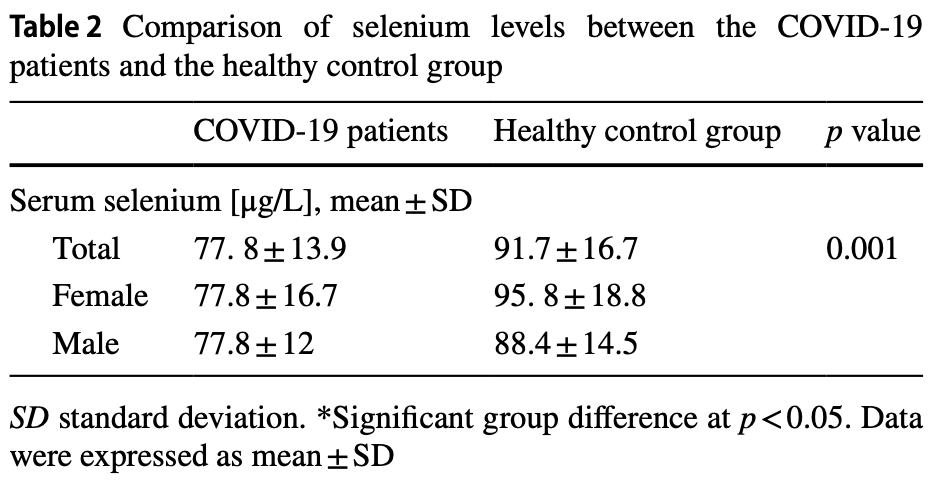
Analysis of 50 hospitalized COVID-19 patients and 50 healthy controls, showing significantly lower selenium levels in COVID-19 patients. There was no significant difference between survivors and non-survivors.
Younesian et al., 1 Jul 2021, Iran, peer-reviewed, 8 authors.
Contact: joshaghani@goums.ac.ir.
Decreased Serum Selenium Levels of COVID-19 Patients in Comparison with Healthy Individuals
Biological Trace Element Research, doi:10.1007/s12011-021-02797-w
Background Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) is the cause of the COVID-19 pandemic and is the cause of increased mortality, especially among elderly patients and those who have severe complications, such as chronic pulmonary obstruction, hypertension, diabetes, and cancer. Nutrition, especially micronutrients, plays an important role in reducing mortality and complications from COVID-19 because micronutrients strengthen our immune system and nutritional status is an important factor that affects the outcome of patients with COVID-19. Among micronutrients, selenium has an important effect on both intrinsic and acquired immunity. Host selenium deficiency affects the viral genome and increases the virulence of viruses. We have investigated the serum selenium levels in COVID-19 patients and healthy control individuals. Methods A total of 50 patients with COVID-19 infection were included in this study. During hospitalization, 13 patients died (non-survivor group) and 37 patients recovered (survivor group). We assessed the serum selenium levels in 50 COVID-19 patients and 50 healthy individuals by Agilent SpectrAA-240 Z atomic absorption spectrometer.
Results The serum selenium level was significantly lower in COVID-19 patients (77. 8 ± 13.9 μg/L) as compared to healthy control individuals (91.7 ± 16.7 μg/L), but there was no significant difference between the survivor and non-survivor groups. Also, there was no significant relationship between serum selenium levels and laboratory findings of COVID-19 patients. Conclusions These results suggest that decreased serum selenium levels may be a risk factor for the COVID-19 infection, but there was no significant relationship between selenium and severity and mortality of COVID-19 disease.
Author Contribution Ommolbanin Younesian wrote the paper. Behnaz Khodabakhshi contributed data or analysis tools. Nafiseh Abdolahi contributed data or analysis tools. Alireza Norouzi conceived and designed the analysis. Nasser Behnampour performed the analysis. Sara Hosseinzadeh collected the data. Seyedeh Somayeh Hosseini Alarzi collected the data. Hamidreza Joshaghani wrote the paper and conceived and designed the analysis.
Declarations Ethics Approval This study was approved by the Ethics Committee of Golestan University of Medical Sciences with an ethics code (IR. GOUMS.REC.1399.297). All procedures performed were in agreement with the principles of the Declaration of Helsinki (1964) and later amendments.
Consent to Participate Informed consent was obtained from all individual participants included in the study.
Consent for Publication Not applicable.
Competing Interests The authors declare no competing interests. Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Avery, Hoffmann, Selenium, selenoproteins, and immunity, Nutrients, doi:10.3390/nu10091203
Bae, Kim, Mini-review on the roles of vitamin C, vitamin D, and selenium in the immune system against COVID-19, Molecules, doi:10.3390/molecules25225346
Beck, Handy, Levander, Host nutritional status: the neglected virulence factor, Trends Microbiol, doi:10.1016/j.tim.2004.07.007
Beck, Levander, Handy, Selenium deficiency and viral infection, J Nutr, doi:10.1093/jn/133.5.1463S
Bermano, Méplan, Mercer, Hesketh, Selenium and viral infection: are there lessons for COVID-19?, Br J Nutr, doi:10.1017/S0007114520003128
Carrasco-Hernandez, Jácome, Vidal, De León, Are RNA viruses candidate agents for the next global pandemic? A review, ILAR J, doi:10.1093/ilar/ilx026
Chang, Pathogenesis of ebola viral haemorrhagic fever: TTP-like syndrome associated with hepatic coagulopathy based on "two activation theory of the endothelium, J Prev Infect Control, doi:10.21767/2471-9668.100029
Chowdhury, Role and effects of micronutrients supplementation in immune system and SARS-Cov-2
Conti, Ronconi, Caraffa, Gallenga, Ross et al., Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies, J Biol Regul Homeost Agents, doi:10.23812/CONTI-E
Eisenmann, Miller, The effect of selenium compounds (selenite, selenate, ebselen) on the production of thromboxane and prostacyclin by the human term placenta in vitro, Toxicol Appl Pharmacol, doi:10.1006/taap.1995.1204
Gladyshev, Arnér, Berry, Brigelius-Flohé, Bruford et al., Selenoprotein gene nomenclature, J Biol Chem, doi:10.1074/jbc.M116.756155
Guan, Liang, -H, Zhao, Liang et al., Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis, Eur Respir J, doi:10.1183/13993003.00547-2020
Hashemian, Murphy, Etemadi, Poustchi, Brockman et al., Toenail mineral concentration and risk of esophageal squamous cell carcinoma, results from the Golestan Cohort Study, Cancer Med, doi:10.1002/cam4.1247
Hiffler, Rakotoambinina, Selenium and RNA virus interactions: Potential implications for SARS-CoV-2 infection (COVID-19), Front Nutr, doi:10.3389/fnut.2020.00164.eCollection2020
Hoffmann, Berry, The influence of selenium on immune responses, Mol Nutr Food Res, doi:10.1002/mnfr.200700330
Huang, Jiao, Xu, Han, Jiao et al., Dietary selenium supplementation alleviates immune toxicity in the hearts of chickens with lead-added drinking water, Avian Pathol, doi:10.1080/03079457.2019.1572102
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.08.018
Jacobson, Lockitch, Direct determination of selenium in serum by graphite-furnace atomic absorption spectrometry with deuterium background correction and a reduced palladium modifier: age-specific reference ranges, Clin Chem, doi:10.1093/clinchem/34.4.709
Jaspers, Zhang, Brighton, Carson, Styblo et al., Selenium deficiency alters epithelial cell morphology and responses to influenza, Free Radical Biol Med, doi:10.1016/j.freeradbiomed.2007.03.017
Keshavarzi, Moore, Najmeddin, Rahmani, The role of selenium and selected trace elements in the etiology of esophageal cancer in high risk Golestan province of Iran, Sci Total Environ, doi:10.1016/j.scitotenv.2012.04.033
Kieliszek, Lipinski, Selenium supplementation in the prevention of coronavirus infections (COVID-19), Med Hypotheses, doi:10.1016/j.mehy.2020.109878
Klok, Kruip, Van Der Meer, Arbous, Gommers et al., Incidence of thrombotic complications in critically ill ICU patients with COVID-19, Thromb Res, doi:10.1016/j.thromres.2020.04.013
Kuwano, Kawashima, Arai S, Antiviral effect of TNF-α and IFN-γ secreted from a CD8+ influenza virus-specific CTL clone, Viral Immunol, doi:10.1089/vim.1993.6.1
Lu, Zhao, Li, Niu, Yang et al., Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding, Lancet, doi:10.1016/S0140-6736(20)30251-8
Mahmoodpoor, Hamishehkar, Shadvar, Ostadi, Sanaie et al., The effect of intravenous selenium on oxidative stress in critically ill patients with acute respiratory distress syndrome, Immunol Invest, doi:10.1080/08820139.2018.1496098
Majeed, Nagabhushanam, Gowda, Mundkur, An Exploratory study of selenium status in normal subjects and COVID-19 patients in south Indian population: case for adequate selenium status: selenium status in COVID-19 patients, doi:10.1016/j.nut.2020.111053
Martitz, Becker, Renko, Stoedter, Hybsier et al., Gene-specific regulation of hepatic selenoprotein expression by interleukin-6, Metallomics, doi:10.1039/c5mt00211g
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium deficiency is associated with mortality risk from COVID-19, Nutrients, doi:10.3390/nu12072098
Muscogiuri, Barrea, Savastano, Colao, Nutritional recommendations for CoVID-19 quarantine, Eur J Clin Nutr, doi:10.1038/s41430-020-0635-2
Nouraie, Pourshams, Kamangar, Sotoudeh, Derakhshan et al., Ecologic study of serum selenium and upper gastrointestinal cancers in Iran, World J Gastroenterol: WJG, doi:10.3748/wjg.v10.i17.2544
Opal, Girard, Ely, The immunopathogenesis of sepsis in elderly patients, Clinical infectious diseases, doi:10.1086/432007
Pourbagheri-Sigaroodi, Bashash, Fateh, Abolghasemi, Laboratory findings in COVID-19 diagnosis and prognosis, Clin Chim Acta, doi:10.1016/j.cca.2020.08.019
Roy, Kiremidjian-Schumacher, Wishe, Cohen, Stotzky, Supplementation with selenium and human immune cell functions. II. Effect on cytotoxic lymphocytes and natural killer cells, Biol Trace Elem Res, doi:10.1007/BF02917222
Sakr, Reinhart, Bloos, Marx, Russwurm et al., Time course and relationship between plasma selenium concentrations, systemic inflammatory response, sepsis, and multiorgan failure, Br J Anaesth, doi:10.1093/bja/aem091
Seale, Torres, Berry, Pitts, A role for selenium-dependent GPX1 in SARS-CoV-2 virulence, Am J Clin Nutr, doi:10.1093/ajcn/nqaa177
Shang, Dong, Ren, Tian, Li et al., The value of clinical parameters in predicting the severity of COVID-19, J Med Virol, doi:10.1002/jmv.26031
Song, Li, Xie, Hou, You, Cytokine storm induced by SARS-CoV-2, Clin Chim Acta, doi:10.1016/j.cca.2020.06.017
Takahashi, Ellingson, Wong, Israelow, Lucas et al., Sex differences in immune responses that underlie COVID-19 disease outcomes, Nature, doi:10.1038/s41586-020-2700-3
Tseng, Ho, Hsu, Lin, Li et al., Selenium is inversely associated with interleukin-6 in the elderly, J Nutr Health Aging, doi:10.1007/s12603-012-0376-6
Viezeliene, Beekhof, Gremmer, Rodovicius, Sadauskiene et al., Selective induction of IL-6 by aluminum-induced oxidative stress can be prevented by selenium, J Trace Elem Med Biol, doi:10.1016/j.jtemb.2012.11.001
Wan, Yi, Fan, Lv, Zhang et al., Characteristics of lymphocyte subsets and cytokines in peripheral blood of 123 hospitalized patients with 2019 novel coronavirus pneumonia, MedRxiv, doi:10.1101/2020.02.10.20021832
Wang, Li, Lu, Huang, Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis, Aging, doi:10.18632/aging.103000
Whitton, Immunopathology during coxsackievirus infection, doi:10.1007/s00281-002-0100-4
Williamson, Walker, Bhaskaran, Bacon, Bates et al., None
Yatmaz, Seow, Gualano, Wong, Stambas et al., Glutathione peroxidase-1 reduces influenza A virus-induced lung inflammation, Am J Respir Cell Mol Biol, doi:10.1165/rcmb.2011-0345OC
Younesian, Younesian, Hosseinzadehjoshaghani, Association of selenium and risk of esophageal cancer: a review, Med Lab J, doi:10.29252/mlj.14.1.1
Yu, Sun, Nan, Zhu, Protection from H1N1 influenza virus infections in mice by supplementation with selenium: a comparison with selenium-deficient mice, Biol Trace Elem Res, doi:10.1007/s12011-010-8726-x
Zhang, Taylor, Bennett, Saad, Rayman, Association between regional selenium status and reported outcome of COVID-19 cases in China, Am J Clin Nutr, doi:10.1093/ajcn/nqaa095
Zheng, Gao, Wang, Song, Liu et al., Functional exhaustion of antiviral lymphocytes in COVID-19 patients, Cell Mol Immunol, doi:10.1038/s41423-020-0402-2
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.1007/s12011-021-02797-w",
"ISSN": [
"0163-4984",
"1559-0720"
],
"URL": "http://dx.doi.org/10.1007/s12011-021-02797-w",
"alternative-id": [
"2797"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "31 March 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "16 June 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "1 July 2021"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics Approval",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "This study was approved by the Ethics Committee of Golestan University of Medical Sciences with an ethics code (IR.GOUMS.REC.1399.297). All procedures performed were in agreement with the principles of the Declaration of Helsinki (1964) and later amendments."
},
{
"group": {
"label": "Consent to Participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Informed consent was obtained from all individual participants included in the study."
},
{
"group": {
"label": "Consent for Publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "Not applicable."
},
{
"group": {
"label": "Competing Interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 5,
"value": "The authors declare no competing interests."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"affiliation": [],
"family": "Younesian",
"given": "Ommolbanin",
"sequence": "first"
},
{
"affiliation": [],
"family": "Khodabakhshi",
"given": "Behnaz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abdolahi",
"given": "Nafiseh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Norouzi",
"given": "Alireza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Behnampour",
"given": "Nasser",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hosseinzadeh",
"given": "Sara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alarzi",
"given": "Seyedeh Somayeh Hosseini",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Joshaghani",
"given": "Hamidreza",
"sequence": "additional"
}
],
"container-title": "Biological Trace Element Research",
"container-title-short": "Biol Trace Elem Res",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
7,
1
]
],
"date-time": "2021-07-01T02:09:51Z",
"timestamp": 1625105391000
},
"deposited": {
"date-parts": [
[
2022,
2,
18
]
],
"date-time": "2022-02-18T00:12:29Z",
"timestamp": 1645143149000
},
"funder": [
{
"DOI": "10.13039/501100008091",
"doi-asserted-by": "publisher",
"name": "Golestan University of Medical Sciences"
}
],
"indexed": {
"date-parts": [
[
2023,
3,
9
]
],
"date-time": "2023-03-09T11:16:06Z",
"timestamp": 1678360566768
},
"is-referenced-by-count": 18,
"issue": "4",
"issued": {
"date-parts": [
[
2021,
7,
1
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2022,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
1
]
],
"date-time": "2021-07-01T00:00:00Z",
"timestamp": 1625097600000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
1
]
],
"date-time": "2021-07-01T00:00:00Z",
"timestamp": 1625097600000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s12011-021-02797-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s12011-021-02797-w/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s12011-021-02797-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "1562-1567",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2021,
7,
1
]
]
},
"published-online": {
"date-parts": [
[
2021,
7,
1
]
]
},
"published-print": {
"date-parts": [
[
2022,
4
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1183/13993003.00547-2020",
"author": "W-j Guan",
"doi-asserted-by": "publisher",
"first-page": "2000547",
"issue": "5",
"journal-title": "Eur Respir J",
"key": "2797_CR1",
"unstructured": "Guan W-j, Liang W-h, Zhao Y, Liang H-r, Chen Z-s, Li Y-m, Liu X-q, Chen R-c, Tang C-l, Wang T (2020) Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J 55(5):2000547. https://doi.org/10.1183/13993003.00547-2020",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.18632/aging.103000",
"author": "B Wang",
"doi-asserted-by": "publisher",
"first-page": "6049",
"issue": "7",
"journal-title": "Aging (Albany NY)",
"key": "2797_CR2",
"unstructured": "Wang B, Li R, Lu Z, Huang Y (2020) Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY) 12(7):6049. https://doi.org/10.18632/aging.103000",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1093/ilar/ilx026",
"author": "R Carrasco-Hernandez",
"doi-asserted-by": "publisher",
"first-page": "343",
"issue": "3",
"journal-title": "ILAR J",
"key": "2797_CR3",
"unstructured": "Carrasco-Hernandez R, Jácome R, López Vidal Y, Ponce de León S (2017) Are RNA viruses candidate agents for the next global pandemic? A review. ILAR J 58(3):343–358. https://doi.org/10.1093/ilar/ilx026",
"volume": "58",
"year": "2017"
},
{
"DOI": "10.1016/S0140-6736(20)30251-8",
"author": "R Lu",
"doi-asserted-by": "publisher",
"first-page": "565",
"issue": "10224",
"journal-title": "Lancet",
"key": "2797_CR4",
"unstructured": "Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N (2020) Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395(10224):565–574. https://doi.org/10.1016/S0140-6736(20)30251-8",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1007/s00281-002-0100-4",
"doi-asserted-by": "publisher",
"key": "2797_CR5",
"unstructured": "Whitton JL (2002) Immunopathology during coxsackievirus infection. In: Seminars in Immunopathology. vol 2. Springer Science & Business Media, pp 201–213. https://doi.org/10.1007/s00281-002-0100-4"
},
{
"DOI": "10.21767/2471-9668.100029",
"doi-asserted-by": "publisher",
"key": "2797_CR6",
"unstructured": "Chang J (2017) Pathogenesis of ebola viral haemorrhagic fever: TTP-like syndrome associated with hepatic coagulopathy based on “two activation theory of the endothelium.” J Prev Infect Control 3:1–7. https://doi.org/10.21767/2471-9668.100029"
},
{
"DOI": "10.1016/j.cca.2020.06.017",
"author": "P Song",
"doi-asserted-by": "publisher",
"first-page": "280",
"journal-title": "Clin Chim Acta",
"key": "2797_CR7",
"unstructured": "Song P, Li W, Xie J, Hou Y, You C (2020) Cytokine storm induced by SARS-CoV-2. Clin Chim Acta 509:280–287. https://doi.org/10.1016/j.cca.2020.06.017",
"volume": "509",
"year": "2020"
},
{
"DOI": "10.1038/s41430-020-0635-2",
"author": "G Muscogiuri",
"doi-asserted-by": "publisher",
"first-page": "850",
"issue": "6",
"journal-title": "Eur J Clin Nutr",
"key": "2797_CR8",
"unstructured": "Muscogiuri G, Barrea L, Savastano S, Colao A (2020) Nutritional recommendations for CoVID-19 quarantine. Eur J Clin Nutr 74(6):850–851. https://doi.org/10.1038/s41430-020-0635-2",
"volume": "74",
"year": "2020"
},
{
"author": "AI Chowdhury",
"first-page": "47",
"journal-title": "Asian J Immunol",
"key": "2797_CR9",
"unstructured": "Chowdhury AI (2020) Role and effects of micronutrients supplementation in immune system and SARS-Cov-2 (COVID-19). Asian J Immunol 4:47–55",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1002/mnfr.200700330",
"author": "PR Hoffmann",
"doi-asserted-by": "publisher",
"first-page": "1273",
"issue": "11",
"journal-title": "Mol Nutr Food Res",
"key": "2797_CR10",
"unstructured": "Hoffmann PR, Berry MJ (2008) The influence of selenium on immune responses. Mol Nutr Food Res 52(11):1273–1280. https://doi.org/10.1002/mnfr.200700330",
"volume": "52",
"year": "2008"
},
{
"DOI": "10.1016/j.tim.2004.07.007",
"author": "MA Beck",
"doi-asserted-by": "publisher",
"first-page": "417",
"issue": "9",
"journal-title": "Trends Microbiol",
"key": "2797_CR11",
"unstructured": "Beck MA, Handy J, Levander OA (2004) Host nutritional status: the neglected virulence factor. Trends Microbiol 12(9):417–423. https://doi.org/10.1016/j.tim.2004.07.007",
"volume": "12",
"year": "2004"
},
{
"DOI": "10.1017/S0007114520003128",
"author": "G Bermano",
"doi-asserted-by": "publisher",
"first-page": "618",
"issue": "6",
"journal-title": "Br J Nutr",
"key": "2797_CR12",
"unstructured": "Bermano G, Méplan C, Mercer DK, Hesketh JE (2021) Selenium and viral infection: are there lessons for COVID-19? Br J Nutr 125(6):618–627. https://doi.org/10.1017/S0007114520003128",
"volume": "125",
"year": "2021"
},
{
"DOI": "10.3389/fnut.2020.00164.eCollection2020",
"author": "L Hiffler",
"doi-asserted-by": "publisher",
"first-page": "164",
"journal-title": "Front Nutr",
"key": "2797_CR13",
"unstructured": "Hiffler L, Rakotoambinina B (2020) Selenium and RNA virus interactions: Potential implications for SARS-CoV-2 infection (COVID-19). Front Nutr 7:164. https://doi.org/10.3389/fnut.2020.00164.eCollection2020",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.mehy.2020.109878",
"author": "M Kieliszek",
"doi-asserted-by": "publisher",
"journal-title": "Med Hypotheses",
"key": "2797_CR14",
"unstructured": "Kieliszek M, Lipinski B (2020) Selenium supplementation in the prevention of coronavirus infections (COVID-19). Med Hypotheses 143:109878. https://doi.org/10.1016/j.mehy.2020.109878",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.1093/clinchem/34.4.709",
"author": "B Jacobson",
"doi-asserted-by": "publisher",
"first-page": "709",
"issue": "4",
"journal-title": "Clin Chem",
"key": "2797_CR15",
"unstructured": "Jacobson B, Lockitch G (1988) Direct determination of selenium in serum by graphite-furnace atomic absorption spectrometry with deuterium background correction and a reduced palladium modifier: age-specific reference ranges. Clin Chem 34(4):709–714. https://doi.org/10.1093/clinchem/34.4.709",
"volume": "34",
"year": "1988"
},
{
"DOI": "10.3390/nu12072098",
"author": "A Moghaddam",
"doi-asserted-by": "publisher",
"first-page": "2098",
"issue": "7",
"journal-title": "Nutrients",
"key": "2797_CR16",
"unstructured": "Moghaddam A, Heller RA, Sun Q, Seelig J, Cherkezov A, Seibert L, Hackler J, Seemann P, Diegmann J, Pilz M (2020) Selenium deficiency is associated with mortality risk from COVID-19. Nutrients 12(7):2098. https://doi.org/10.3390/nu12072098",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1093/ajcn/nqaa095",
"author": "J Zhang",
"doi-asserted-by": "publisher",
"first-page": "1297",
"issue": "6",
"journal-title": "Am J Clin Nutr",
"key": "2797_CR17",
"unstructured": "Zhang J, Taylor EW, Bennett K, Saad R, Rayman MP (2020) Association between regional selenium status and reported outcome of COVID-19 cases in China. Am J Clin Nutr 111(6):1297–1299. https://doi.org/10.1093/ajcn/nqaa095",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"author": "JH Im",
"doi-asserted-by": "publisher",
"first-page": "390",
"journal-title": "Int J Infect Dis",
"key": "2797_CR18",
"unstructured": "Im JH, Je YS, Baek J, Chung MH, Kwon HY, Lee JS (2020) Nutritional status of patients with COVID-19. Int J Infect Dis 100:390–393. https://doi.org/10.1016/j.ijid.2020.08.018",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1016/j.nut.2020.111053",
"author": "M Majeed",
"doi-asserted-by": "publisher",
"journal-title": "Nutrition (Burbank, Los Angeles County, Calif)",
"key": "2797_CR19",
"unstructured": "Majeed M, Nagabhushanam K, Gowda S, Mundkur L (2020) An Exploratory study of selenium status in normal subjects and COVID-19 patients in south Indian population: case for adequate selenium status: selenium status in COVID-19 patients. Nutrition (Burbank, Los Angeles County, Calif) 82:111053. https://doi.org/10.1016/j.nut.2020.111053",
"volume": "82",
"year": "2020"
},
{
"DOI": "10.1016/j.scitotenv.2012.04.033",
"author": "B Keshavarzi",
"doi-asserted-by": "publisher",
"first-page": "89",
"journal-title": "Sci Total Environ",
"key": "2797_CR20",
"unstructured": "Keshavarzi B, Moore F, Najmeddin A, Rahmani F (2012) The role of selenium and selected trace elements in the etiology of esophageal cancer in high risk Golestan province of Iran. Sci Total Environ 433:89–97. https://doi.org/10.1016/j.scitotenv.2012.04.033",
"volume": "433",
"year": "2012"
},
{
"DOI": "10.1002/cam4.1247",
"author": "M Hashemian",
"doi-asserted-by": "publisher",
"first-page": "3052",
"issue": "12",
"journal-title": "Cancer Med",
"key": "2797_CR21",
"unstructured": "Hashemian M, Murphy G, Etemadi A, Poustchi H, Brockman JD, Kamangar F, Pourshams A, Khoshnia M, Gharavi A, Dawsey SM (2017) Toenail mineral concentration and risk of esophageal squamous cell carcinoma, results from the Golestan Cohort Study. Cancer Med 6(12):3052–3059. https://doi.org/10.1002/cam4.1247",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.3748/wjg.v10.i17.2544",
"author": "M Nouraie",
"doi-asserted-by": "publisher",
"first-page": "2544",
"issue": "17",
"journal-title": "World J Gastroenterol: WJG",
"key": "2797_CR22",
"unstructured": "Nouraie M, Pourshams A, Kamangar F, Sotoudeh M, Derakhshan MH, Akbari MR, Fakheri H, Zahedi MJ, Caldwell K, Abnet CC (2004) Ecologic study of serum selenium and upper gastrointestinal cancers in Iran. World J Gastroenterol: WJG 10(17):2544. https://doi.org/10.3748/wjg.v10.i17.2544",
"volume": "10",
"year": "2004"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"author": "EJ Williamson",
"doi-asserted-by": "publisher",
"first-page": "430",
"issue": "7821",
"journal-title": "Nature",
"key": "2797_CR23",
"unstructured": "Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P (2020) Factors associated with COVID-19-related death using OpenSAFELY. Nature 584(7821):430–436. https://doi.org/10.1038/s41586-020-2521-4",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2700-3",
"author": "T Takahashi",
"doi-asserted-by": "publisher",
"first-page": "315",
"issue": "7837",
"journal-title": "Nature",
"key": "2797_CR24",
"unstructured": "Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, Silva J, Mao T, Oh JE, Tokuyama M (2020) Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature 588(7837):315–320. https://doi.org/10.1038/s41586-020-2700-3",
"volume": "588",
"year": "2020"
},
{
"DOI": "10.1086/432007",
"author": "SM Opal",
"doi-asserted-by": "publisher",
"first-page": "S504",
"issue": "Supplement_7",
"journal-title": "Clinical infectious diseases",
"key": "2797_CR25",
"unstructured": "Opal SM, Girard TD, Ely EW (2005) The immunopathogenesis of sepsis in elderly patients. Clinical infectious diseases 41(Supplement_7):S504–S512. https://doi.org/10.1086/432007",
"volume": "41",
"year": "2005"
},
{
"DOI": "10.1074/jbc.M116.756155",
"author": "VN Gladyshev",
"doi-asserted-by": "publisher",
"first-page": "24036",
"issue": "46",
"journal-title": "J Biol Chem",
"key": "2797_CR26",
"unstructured": "Gladyshev VN, Arnér ES, Berry MJ, Brigelius-Flohé R, Bruford EA, Burk RF, Carlson BA, Castellano S, Chavatte L, Conrad M (2016) Selenoprotein gene nomenclature. J Biol Chem 291(46):24036–24040. https://doi.org/10.1074/jbc.M116.756155",
"volume": "291",
"year": "2016"
},
{
"DOI": "10.29252/mlj.14.1.1",
"author": "O Younesian",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Med Lab J",
"key": "2797_CR27",
"unstructured": "Younesian O, Younesian S, HosseinzadehJoshaghani SHR (2020) Association of selenium and risk of esophageal cancer: a review. Med Lab J 14:1–9. https://doi.org/10.29252/mlj.14.1.1",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.3390/nu10091203",
"author": "JC Avery",
"doi-asserted-by": "publisher",
"first-page": "1203",
"issue": "9",
"journal-title": "Nutrients",
"key": "2797_CR28",
"unstructured": "Avery JC, Hoffmann PR (2018) Selenium, selenoproteins, and immunity. Nutrients 10(9):1203. https://doi.org/10.3390/nu10091203",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1093/ajcn/nqaa177",
"author": "LA Seale",
"doi-asserted-by": "publisher",
"first-page": "447",
"issue": "2",
"journal-title": "Am J Clin Nutr",
"key": "2797_CR29",
"unstructured": "Seale LA, Torres DJ, Berry MJ, Pitts MW (2020) A role for selenium-dependent GPX1 in SARS-CoV-2 virulence. Am J Clin Nutr 112(2):447–448. https://doi.org/10.1093/ajcn/nqaa177",
"volume": "112",
"year": "2020"
},
{
"DOI": "10.1093/jn/133.5.1463S",
"author": "MA Beck",
"doi-asserted-by": "publisher",
"first-page": "1463S",
"issue": "5",
"journal-title": "J Nutr",
"key": "2797_CR30",
"unstructured": "Beck MA, Levander OA, Handy J (2003) Selenium deficiency and viral infection. J Nutr 133(5):1463S-1467S. https://doi.org/10.1093/jn/133.5.1463S",
"volume": "133",
"year": "2003"
},
{
"DOI": "10.1165/rcmb.2011-0345OC",
"author": "S Yatmaz",
"doi-asserted-by": "publisher",
"first-page": "17",
"issue": "1",
"journal-title": "Am J Respir Cell Mol Biol",
"key": "2797_CR31",
"unstructured": "Yatmaz S, Seow HJ, Gualano RC, Wong ZX, Stambas J, Selemidis S, Crack PJ, Bozinovski S, Anderson GP, Vlahos R (2013) Glutathione peroxidase-1 reduces influenza A virus–induced lung inflammation. Am J Respir Cell Mol Biol 48(1):17–26. https://doi.org/10.1165/rcmb.2011-0345OC",
"volume": "48",
"year": "2013"
},
{
"DOI": "10.1038/s41423-020-0402-2",
"author": "M Zheng",
"doi-asserted-by": "publisher",
"first-page": "533",
"issue": "5",
"journal-title": "Cell Mol Immunol",
"key": "2797_CR32",
"unstructured": "Zheng M, Gao Y, Wang G, Song G, Liu S, Sun D, Xu Y, Tian Z (2020) Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol 17(5):533–535. https://doi.org/10.1038/s41423-020-0402-2",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1080/03079457.2019.1572102",
"author": "H Huang",
"doi-asserted-by": "publisher",
"first-page": "230",
"issue": "3",
"journal-title": "Avian Pathol",
"key": "2797_CR33",
"unstructured": "Huang H, Jiao X, Xu Y, Han Q, Jiao W, Liu Y, Li S, Teng X (2019) Dietary selenium supplementation alleviates immune toxicity in the hearts of chickens with lead-added drinking water. Avian Pathol 48(3):230–237. https://doi.org/10.1080/03079457.2019.1572102",
"volume": "48",
"year": "2019"
},
{
"DOI": "10.1007/BF02917222",
"author": "M Roy",
"doi-asserted-by": "publisher",
"first-page": "115",
"journal-title": "Biol Trace Elem Res",
"key": "2797_CR34",
"unstructured": "Roy M, Kiremidjian-Schumacher L, Wishe H, Cohen M, Stotzky G (1994) Supplementation with selenium and human immune cell functions. II. Effect on cytotoxic lymphocytes and natural killer cells. Biol Trace Elem Res 41:115–127. https://doi.org/10.1007/BF02917222",
"volume": "41",
"year": "1994"
},
{
"DOI": "10.1089/vim.1993.6.1",
"author": "K Kuwano",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Viral Immunol",
"key": "2797_CR35",
"unstructured": "Kuwano K, Kawashima T, ARAI S, (1993) Antiviral effect of TNF-α and IFN-γ secreted from a CD8+ influenza virus-specific CTL clone. Viral Immunol 6(1):1–11. https://doi.org/10.1089/vim.1993.6.1",
"volume": "6",
"year": "1993"
},
{
"DOI": "10.1007/s12011-010-8726-x",
"author": "L Yu",
"doi-asserted-by": "publisher",
"first-page": "254",
"issue": "1",
"journal-title": "Biol Trace Elem Res",
"key": "2797_CR36",
"unstructured": "Yu L, Sun L, Nan Y, Zhu L-Y (2011) Protection from H1N1 influenza virus infections in mice by supplementation with selenium: a comparison with selenium-deficient mice. Biol Trace Elem Res 141(1):254–261. https://doi.org/10.1007/s12011-010-8726-x",
"volume": "141",
"year": "2011"
},
{
"DOI": "10.23812/CONTI-E",
"author": "P Conti",
"doi-asserted-by": "publisher",
"first-page": "327",
"issue": "2",
"journal-title": "J Biol Regul Homeost Agents",
"key": "2797_CR37",
"unstructured": "Conti P, Ronconi G, Caraffa A, Gallenga C, Ross R, Frydas I, Kritas S (2020) Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents 34(2):327–331. https://doi.org/10.23812/CONTI-E",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1101/2020.02.10.20021832",
"author": "S Wan",
"doi-asserted-by": "publisher",
"journal-title": "MedRxiv",
"key": "2797_CR38",
"unstructured": "Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, Lang C, Xiao Q, Xiao K, Yi Z (2020) Characteristics of lymphocyte subsets and cytokines in peripheral blood of 123 hospitalized patients with 2019 novel coronavirus pneumonia (NCP). MedRxiv. https://doi.org/10.1101/2020.02.10.20021832",
"year": "2020"
},
{
"DOI": "10.1007/s12603-012-0376-6",
"author": "C-K Tseng",
"doi-asserted-by": "publisher",
"first-page": "280",
"issue": "3",
"journal-title": "J Nutr Health Aging",
"key": "2797_CR39",
"unstructured": "Tseng C-K, Ho C-T, Hsu H-S, Lin C-H, Li C-I, Li T-C, Liu C-S, Lin C-C, Lin W-Y (2013) Selenium is inversely associated with interleukin-6 in the elderly. J Nutr Health Aging 17(3):280–284. https://doi.org/10.1007/s12603-012-0376-6",
"volume": "17",
"year": "2013"
},
{
"DOI": "10.1016/j.freeradbiomed.2007.03.017",
"author": "I Jaspers",
"doi-asserted-by": "publisher",
"first-page": "1826",
"issue": "12",
"journal-title": "Free Radical Biol Med",
"key": "2797_CR40",
"unstructured": "Jaspers I, Zhang W, Brighton L, Carson J, Styblo M, Beck M (2007) Selenium deficiency alters epithelial cell morphology and responses to influenza. Free Radical Biol Med 42(12):1826–1837. https://doi.org/10.1016/j.freeradbiomed.2007.03.017",
"volume": "42",
"year": "2007"
},
{
"DOI": "10.1016/j.jtemb.2012.11.001",
"author": "D Viezeliene",
"doi-asserted-by": "publisher",
"first-page": "226",
"issue": "3",
"journal-title": "J Trace Elem Med Biol",
"key": "2797_CR41",
"unstructured": "Viezeliene D, Beekhof P, Gremmer E, Rodovicius H, Sadauskiene I, Jansen E, Ivanov L (2013) Selective induction of IL-6 by aluminum-induced oxidative stress can be prevented by selenium. J Trace Elem Med Biol 27(3):226–229. https://doi.org/10.1016/j.jtemb.2012.11.001",
"volume": "27",
"year": "2013"
},
{
"DOI": "10.1039/c5mt00211g",
"author": "J Martitz",
"doi-asserted-by": "publisher",
"first-page": "1515",
"issue": "11",
"journal-title": "Metallomics",
"key": "2797_CR42",
"unstructured": "Martitz J, Becker N, Renko K, Stoedter M, Hybsier S, Schomburg L (2015) Gene-specific regulation of hepatic selenoprotein expression by interleukin-6. Metallomics 7(11):1515–1521. https://doi.org/10.1039/c5mt00211g",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.1080/08820139.2018.1496098",
"author": "A Mahmoodpoor",
"doi-asserted-by": "publisher",
"first-page": "147",
"issue": "2",
"journal-title": "Immunol Invest",
"key": "2797_CR43",
"unstructured": "Mahmoodpoor A, Hamishehkar H, Shadvar K, Ostadi Z, Sanaie S, Saghaleini SH, Nader ND (2019) The effect of intravenous selenium on oxidative stress in critically ill patients with acute respiratory distress syndrome. Immunol Invest 48(2):147–159. https://doi.org/10.1080/08820139.2018.1496098",
"volume": "48",
"year": "2019"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"author": "F Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"issue": "10229",
"journal-title": "Lancet",
"key": "2797_CR44",
"unstructured": "Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229):1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2020.04.013",
"author": "F Klok",
"doi-asserted-by": "publisher",
"first-page": "145",
"journal-title": "Thromb Res",
"key": "2797_CR45",
"unstructured": "Klok F, Kruip M, Van der Meer N, Arbous M, Gommers D, Kant K, Kaptein F, van Paassen J, Stals M, Huisman M (2020) Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 191:145–147. https://doi.org/10.1016/j.thromres.2020.04.013",
"volume": "191",
"year": "2020"
},
{
"DOI": "10.1006/taap.1995.1204",
"author": "CJ Eisenmann",
"doi-asserted-by": "publisher",
"first-page": "18",
"issue": "1",
"journal-title": "Toxicol Appl Pharmacol",
"key": "2797_CR46",
"unstructured": "Eisenmann CJ, Miller RK (1995) The effect of selenium compounds (selenite, selenate, ebselen) on the production of thromboxane and prostacyclin by the human term placenta in vitro. Toxicol Appl Pharmacol 135(1):18–24. https://doi.org/10.1006/taap.1995.1204",
"volume": "135",
"year": "1995"
},
{
"DOI": "10.3390/molecules25225346",
"author": "M Bae",
"doi-asserted-by": "publisher",
"first-page": "5346",
"issue": "22",
"journal-title": "Molecules",
"key": "2797_CR47",
"unstructured": "Bae M, Kim H (2020) Mini-review on the roles of vitamin C, vitamin D, and selenium in the immune system against COVID-19. Molecules 25(22):5346. https://doi.org/10.3390/molecules25225346",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1016/j.cca.2020.08.019",
"author": "A Pourbagheri-Sigaroodi",
"doi-asserted-by": "publisher",
"first-page": "475",
"journal-title": "Clin Chim Acta",
"key": "2797_CR48",
"unstructured": "Pourbagheri-Sigaroodi A, Bashash D, Fateh F, Abolghasemi H (2020) Laboratory findings in COVID-19 diagnosis and prognosis. Clin Chim Acta 510:475–482. https://doi.org/10.1016/j.cca.2020.08.019",
"volume": "510",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26031",
"author": "W Shang",
"doi-asserted-by": "publisher",
"first-page": "2188",
"issue": "10",
"journal-title": "J Med Virol",
"key": "2797_CR49",
"unstructured": "Shang W, Dong J, Ren Y, Tian M, Li W, Hu J, Li Y (2020) The value of clinical parameters in predicting the severity of COVID-19. J Med Virol 92(10):2188–2192. https://doi.org/10.1002/jmv.26031",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1093/bja/aem091",
"author": "Y Sakr",
"doi-asserted-by": "publisher",
"first-page": "775",
"issue": "6",
"journal-title": "Br J Anaesth",
"key": "2797_CR50",
"unstructured": "Sakr Y, Reinhart K, Bloos F, Marx G, Russwurm S, Bauer M, Brunkhorst F (2007) Time course and relationship between plasma selenium concentrations, systemic inflammatory response, sepsis, and multiorgan failure. Br J Anaesth 98(6):775–784. https://doi.org/10.1093/bja/aem091",
"volume": "98",
"year": "2007"
}
],
"reference-count": 50,
"references-count": 50,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s12011-021-02797-w"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Biochemistry (medical)",
"Inorganic Chemistry",
"Clinical Biochemistry",
"General Medicine",
"Biochemistry",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Decreased Serum Selenium Levels of COVID-19 Patients in Comparison with Healthy Individuals",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "200"
}