Impact of Folic acid status or its metabolites and hypoxia on COVID-19
et al., HIV Nursing, 22:2, Oct 2022
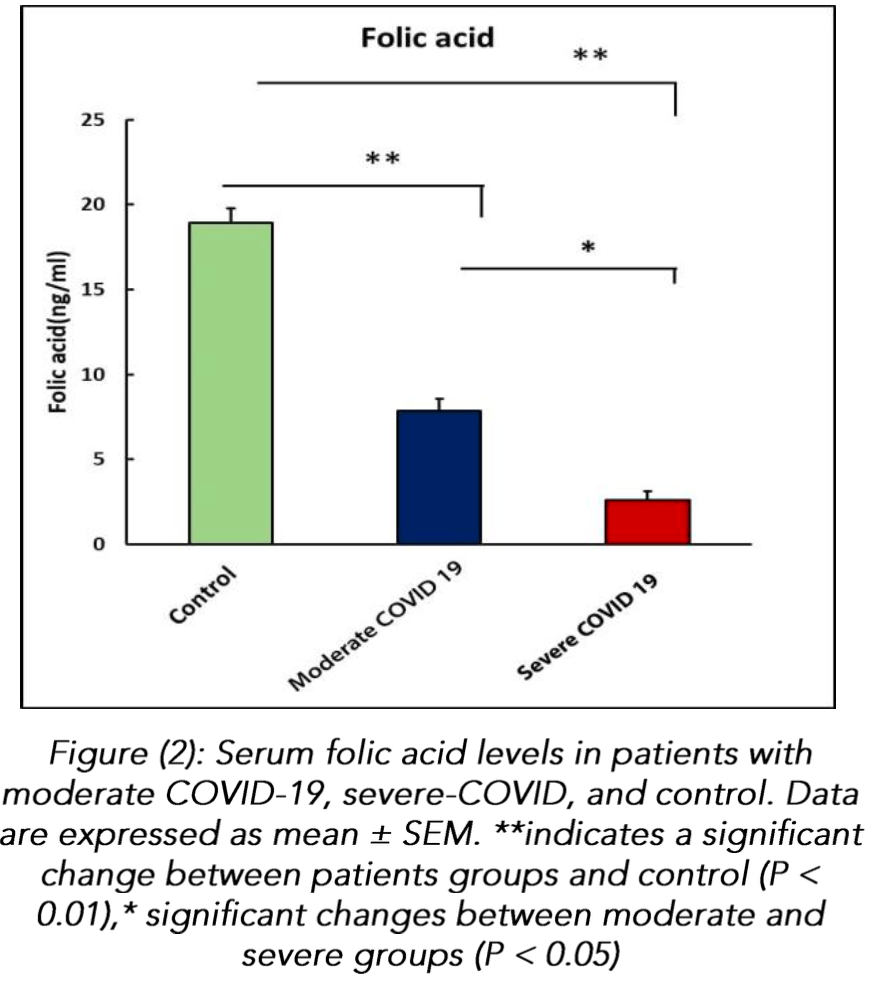
Retrospective 75 COVID-19 patients and 45 healthy controls in Iraq, showing lower folic acid levels in COVID-19 patients, and lower levels for severe vs. moderate cases.
Yas et al., 10 Oct 2022, retrospective, Iraq, peer-reviewed, 3 authors, study period September 2021 - January 2022.
Background: Folic acid is a hydro-soluble vitamin that classifies as part of the vitamin B complex. The coenzymes of folic acid are actively involved in the one-carbon metabolism. It was established that folate metabolism is involved in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).The study aimed to investigate that decreased folate levels with hypoxia may involve in patients with COVID-19 Methods: The study was performed between September 2021 to January 2022. A 75 subjects were enrolled in this study with COVID-19 (moderate =35, severe=45) with mean age (56 ± 1.6; 37 males, 38 female), and 45 subjects appeared to be normal healthy persons as the control group with mean age (41 ± 1.5; 17 males, 28 female) Folic acid levels was measured by colorimetric method. Serum 5-MTHF, HIF-1α, and TNF-α were measured by ELISA. Results: : The results clearly showed low folic acid and its derivative 5-MTHF levels in patient groups with COVID-19 compared to control (P<0.01); a great effect was shown in the severe group. The finding also declared that serum level of TNF-α and HIF-1α were significantly increased in patients with COVID-19 infection compared to control groups (p <0.01). Conclusions: The main findings may go some way towards establishing a link between folic acid status, a hypoxia and COVID-19 prevalence, with a possible association to the disease severity. Therefore, folic acid supplementation may protect against COVID-19
References
Acosta-Elias, Espinosa-Tanguma, The folate concentration and/or folic acid metabolites in plasma as factor for COVID-19 infection, Frontiers in pharmacology, doi:10.3389/fphar.2020.01062
Cascella, Rajnik, Aleem, Dulebohn, Napoli, Features, evaluation, and treatment of coronavirus (COVID-19)
Chen, Yan, Man, ? covid19?> TNFα inhibitor may be effective for severe COVID-19: learning from toxic epidermal necrolysis, Therapeutic, doi:10.1177/1753466620926800
Corman, Rabenau, Adams, Oberle, Funk et al., SARS-CoV-2 asymptomatic and symptomatic patients and risk for transfusion transmission, Transfusion
Ducker, Rabinowitz, One-carbon metabolism in health and disease, Cell metabolism, doi:10.1016/j.cmet.2016.08.009
Fisher, Hypoxemia in COVID-19 patients: An hypothesis, Medical Hypotheses, doi:10.1016/j.mehy.2020.110022
Froese, Fowler, Baumgartner, Vitamin B12, folate, and the methionine remethylation cyclebiochemistry, pathways, and regulation, Journal of inherited metabolic disease, doi:10.1002/jimd.12009
Födinger, Hörl, Sunder-Plassmann, Molecular biology of 5, 10-methylenetetrahydrofolate reductase, Journal of Nephrology
Gupta, Zhao, Evans, The stimulation of thrombosis by hypoxia, Thrombosis research, doi:10.1016/j.thromres.2019.07.013
Jahani, Dokaneheifard, Mansouri, Hypoxia: A key feature of COVID-19 launching activation of HIF-1 and cytokine storm, Journal of inflammation, doi:10.1186/s12950-020-00263-3
Karki, Sb, Samir P Eas, Death, -Αai-Γtic et al., SARS-CoV-2 Infection and Cytokine Shock Syndromes, doi:10.1016/j.cell.2020.11.025
Kempuraj, Selvakumar, Ahmed, Raikwar, Thangavel et al., COVID-19, mast cells, cytokine storm, psychological stress, and neuroinflammation, The Neuroscientist, doi:10.1177/1073858420941476
Kumar, Choi, Hypoxia inducible factor pathway and physiological adaptation: a cell survival pathway? Mediators of inflammation, doi:10.1155/2015/584758
Li, Xu, Yu, Wang, Tao et al., Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan, Journal of Allergy and Clinical Immunology, doi:10.1016/j.jaci.2020.04.006
Mcelvaney, Mcevoy, Mcelvaney, Carroll, Murphy et al., Characterization of the inflammatory response to severe COVID-19 illness. American journal of respiratory and critical care medicine, doi:10.1164/rccm.202005-1583OC
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., COVID-19: Consider cytokine storm syndromes and immunosuppression The, Lancet
Meisel, Efros, Bleier, Halevi, Segal et al., Folate levels in patients hospitalized with coronavirus disease 2019, Nutrients, doi:10.3390/nu13030812
Mittal, Manjunath, Ranjan, Kaushik, Kumar et al., COVID-19 pandemic: Insights into structure, function, and hACE2 receptor recognition by SARS-CoV-2, PLoS pathogens, doi:10.1371/journal.ppat.1008762
Ntyonga-Pono, COVID-19 infection and oxidative stress: an under-explored approach for prevention and treatment? The Pan African, Medical Journal
Nägele, Haubner, Tanner, Ruschitzka, Flammer et al., Potential role for tissue factor in the pathogenesis of hypercoagulability associated with in COVID-19, Journal of thrombosis and thrombolysis, doi:10.1007/s11239-020-02172-x
Rabaan, Sh, Muhammad, Khan, Sule et al., Role of inflammatory cytokines in COVID-19 patients: a review on molecular mechanisms, immune functions, immunopathology and immunomodulatory drugs to counter cytokine storm, Vaccines, doi:10.3390/vaccines9050436
Sadeghi-Haddad-Zavareh, Bayani, Shokri, Ebrahimpour, Babazadeh et al., C-reactive protein as a prognostic indicator in COVID-19 patients
Shimabukuro-Vornhagen, Gödel, Subklewe, Stemmler, Schlößer et al., Cytokine release syndrome. Journal for immunotherapy of cancer, doi:10.1186/s40425-018-0343-9
Shirvani, Nouri, Sakhinia, Babaloo, Mohammadzaeh et al., The molecular and clinical evidence of vitamin D signaling as a modulator of the immune system: Role in Behçet's disease, Immunology Letters, doi:10.1016/j.imlet.2019.03.017
Smith, Robbins, Ratcliffe, Yufei, Mingli et al., Utility of the neutrophil-to-lymphocyte ratio and C-reactive protein level for coronavirus disease 2019 (COVID-19), Scandinavian journal of clinical and laboratory investigation, doi:10.1080/00365513.2020.1803587
Wang, Ye, Ye, Li, Gao et al., Up-regulation of IL-6 and TNF-α induced by SARS-coronavirus spike protein in murine macrophages via NF-κB pathway, Virus research, doi:10.1016/j.virusres.2007.02.007
Ye, Chen, Li, Lan, Ji et al., Dynamic changes of D-dimer and neutrophil-lymphocyte count ratio as prognostic biomarkers in COVID-19, Respiratory research, doi:10.1186/s12931-020-01428-7
Zhang, Guo, Kim, Shah, Zhang et al., SARS-CoV-2 hijacks folate and one-carbon metabolism for viral replication, Nature communications, doi:10.1038/s41467-021-21903-z
Zhang, Wu, Zhao, Liu, Zhou et al., Role of HIF-1α in the regulation ACE and ACE2 expression in hypoxic human pulmonary artery smooth muscle cells, American Journal of Physiology-Lung Cellular and Molecular Physiology, doi:10.1152/ajplung.90415.2008
Zhang, Yan, Fan, Liu, Liu et al., None
Zhu, Ea, HIF-1 α promotes SARS-CoV-2 infection and aggravates in fl ammatory responses to COVID-19, Signal Transduct Target, doi:10.1038/s41392-021-
Zhu, Rhee, Cheng, Waliany, Chang et al., Cardiovascular complications in patients with COVID-19: consequences of viral toxicities and host immune response, Current cardiology reports, doi:10.1007/s11886-020-01292-3