Proton pump inhibitor use and risk of spontaneous bacterial peritonitis in cirrhotic patients: a systematic review and meta-analysis
et al., Genetics and Molecular Research, doi:10.4238/2015.July.3.25, Dec 2015
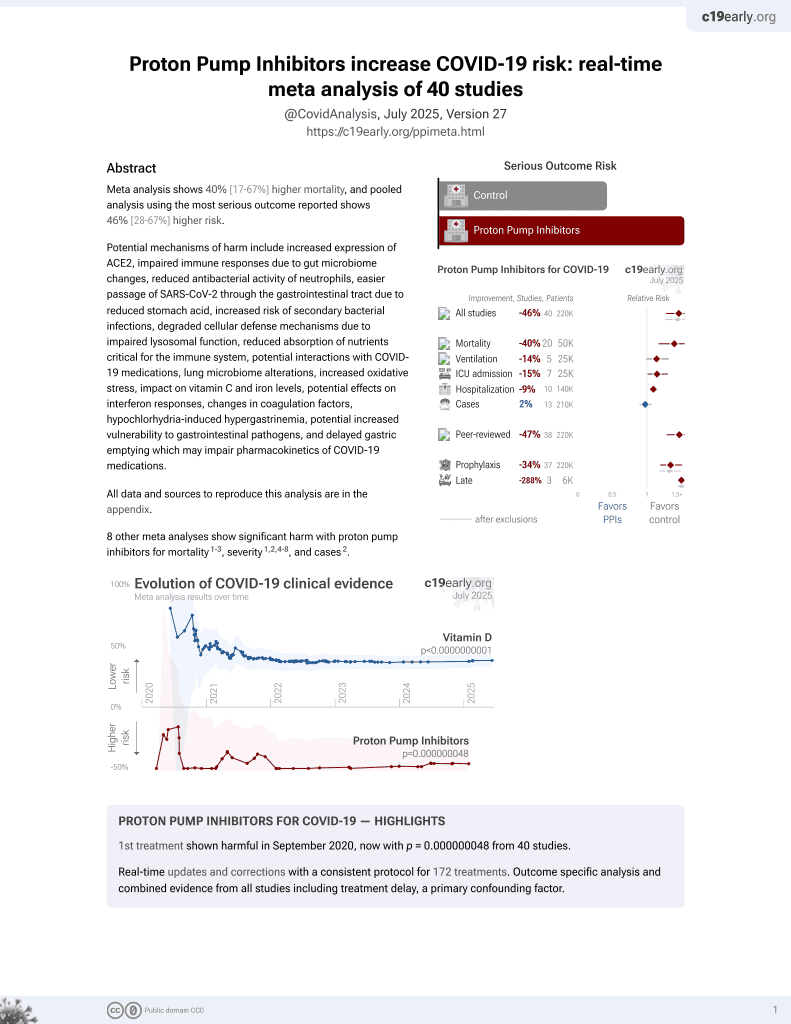
PPIs for COVID-19
1st treatment shown to increase risk in
September 2020, now with p = 0.000000048 from 40 studies.
6,400+ studies for
210+ treatments. c19early.org
|
Meta analysis of 17 observational studies with 8,204 patients showing 2-fold increased risk of spontaneous bacterial peritonitis (SBP) and overall bacterial infection with proton pump inhibitor (PPI) use in cirrhotic patients with ascites. The association remained significant in subgroup analyses of journal articles and studies reporting adjusted effect estimates.
Xu et al., 31 Dec 2015, peer-reviewed, 10 authors.
Contact: dongjh301@sina.com.
Proton pump inhibitor use and risk of spontaneous bacterial peritonitis in cirrhotic patients: a systematic review and meta-analysis
Genetics and Molecular Research, doi:10.4238/2015.july.3.25
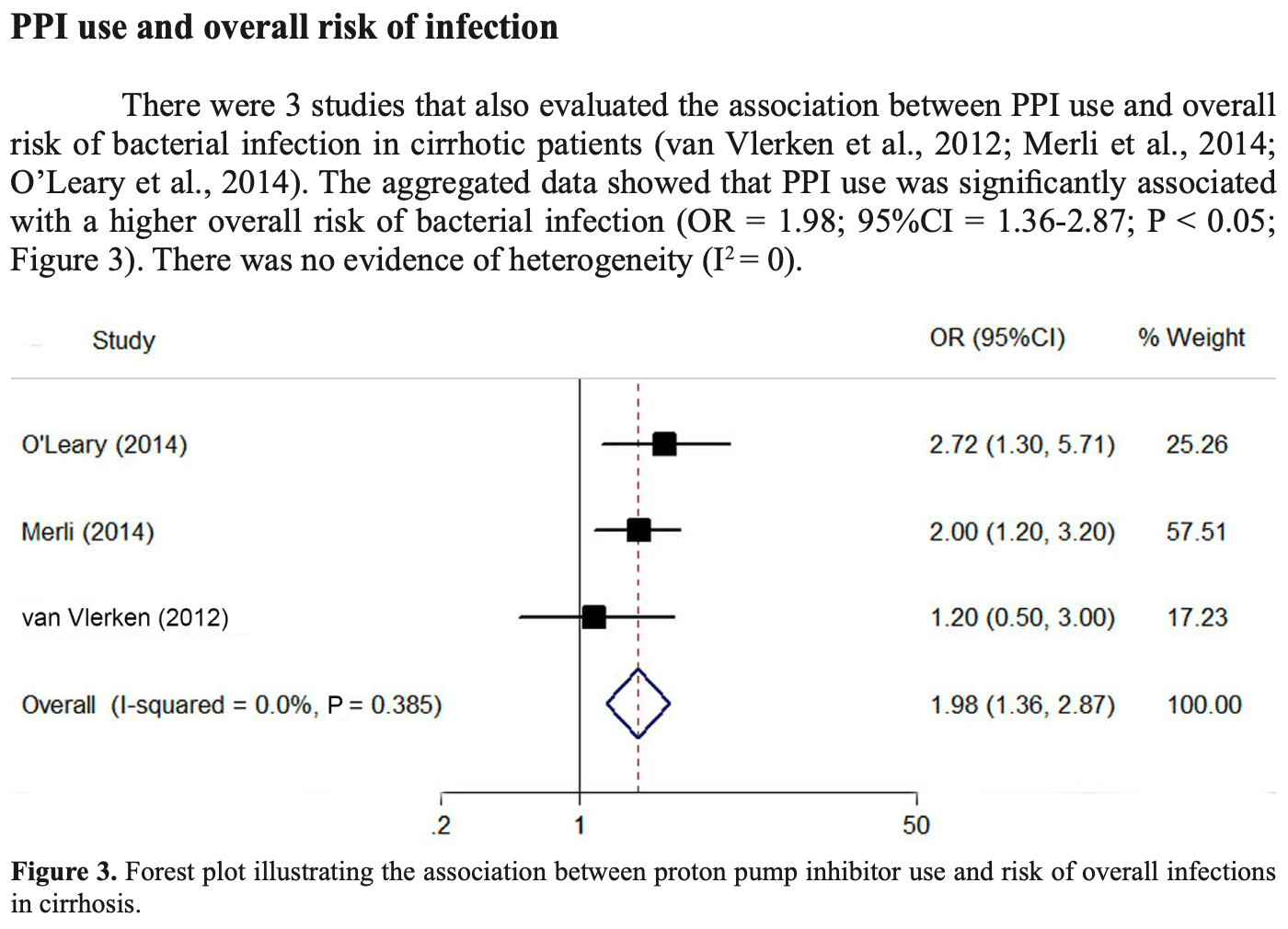
We used a meta-analysis approach to investigate the association between proton pump inhibitor (PPI) use and risk of spontaneous bacterial peritonitis (SBP) in cirrhotic patients. We searched Ovid Medline, Embase, and the Cochrane Library to identify eligible studies. We included studies that compared cirrhotic patients who did or did not use PPIs. The primary outcome was SBP, and the secondary outcome was overall bacterial infection. Results were pooled using random-effect models. This process led to identification of 12 journal articles and 5 conference abstracts. The pooled data showed that PPI use in patients with cirrhosis and ascites was significantly associated with an increased risk of SBP [odds ratio (OR) = 2.17; 95% Proton pump inhibitors in cirrhotic patients ©FUNPEC-RP www.funpecrp.com.br Genetics and Molecular Research 14 (3): 7490-7501 (2015) confidence interval (CI) = 1.46-3.23; P < 0.05; I 2 = 85.6%] and overall risk of bacterial infection (OR = 1.98; 95%CI = 1.36-2.87; P < 0.05; I 2 = 0). Subgroup analysis revealed that journal articles and studies reporting adjusted effect estimates demonstrated that PPI users had a significantly increased risk of SBP (OR = 2.13; 95%CI = 1.61-2.82; P < 0.05; I 2 = 29.4%; and OR = 1.98; 95%CI = 1.42-2.77; P < 0.05; I 2 = 67%, respectively). In conclusion, PPI use increased the risk of SBP and overall bacterial infection in patients with cirrhosis and ascites. PPIs should be administered after careful assessment of the indications in cirrhotic patients. Future well-designed prospective studies are warranted to clarify the dose relationships and to compare infection risks associated with different classes of PPIs.
References
Aditi, Crippin, Abhishek, Role of proton pump inhibitors in the development of spontaneous bacterial peritonitis amongst cirrhotics; a retrospective cohort study, Gastroenterology
Bajaj, Zadvornova, Heuman, Hafeezullah, Association of proton pump inhibitor therapy with spontaneous bacterial peritonitis in cirrhotic patients with ascites, Am. J. Gastroenterol
Bulsiewicz, Scherer, Feinglass, Howden, Proton pump inhibitor (PPI) use is independently associated with spontaneous bacterial peritonitis (SBP) in cirrhotics with ascites, Gastroenterology
Campbell, Obstein, Reddy, Yang, Association between proton pump inhibitor use and spontaneous bacterial peritonitis, Dig. Dis. Sci
Chang, Chen, Hc, Yeh, Small intestine dysmotility and bacterial overgrowth in cirrhotic patients with spontaneous bacterial peritonitis, Hepatology
Choi, Lee, Kim, Lee, Association between acid suppressive therapy and spontaneous bacterial peritonitis in cirrhotic patients with ascites, Scand. J. Gastroenterol
Davies, Crombie, Tavakoli, When can odds ratios mislead?, BMJ
De Vos, Vroey, Garcia, Roy, Role of proton pump inhibitors in the occurrence and the prognosis of spontaneous bacterial peritonitis in cirrhotic patients with ascites, Liver Int
Deshpande, Pasupuleti, Thota, Pant, Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis, J. Gastroenterol. Hepatol
Egger, Smith, Schneider, Minder, Bias in meta-analysis detected by a simple, graphical test, BMJ
Garcia-Martinez, Francés, Zapater, Giménez, Use of proton pump inhibitors decrease cellular oxidative burst in patients with decompensated cirrhosis, J. Gastroenterol. Hepatol
Garcia-Tsao, Sanyal, Grace, Carey, Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis, Hepatology
Ginès, Cárdenas, Arroyo, Rodés, Management of cirrhosis and ascites, N. Engl. J. Med
Goel, Deshpande, Lopez, Hall, Increased rate of spontaneous bacterial peritonitis among cirrhotic patients receiving pharmacologic acid suppression, Clin. Gastroenterol. Hepatol
Herzig, Howell, Ngo, Marcantonio, Acid-suppressive medication use and the risk for hospitalacquired pneumonia, JAMA
Higgins, Thompson, Deeks, Altman, Measuring inconsistency in meta-analyses, BMJ
Jacobs, Adame, Attaluri, Valestin, Dysmotility and proton pump inhibitor use are independent risk factors for small intestinal bacterial and/or fungal overgrowth, Aliment. Pharmacol. Ther
Kalaitzakis, Björnsson, Inadequate use of proton-pump inhibitors in patients with liver cirrhosis, Eur. J. Gastroenterol. Hepatol
Kwon, Koh, Kim, Jung, Mortality associated with proton pump inhibitors in cirrhotic patients with spontaneous bacterial peritonitis, J. Gastroenterol. Hepatol
Leontiadis, Sharma, Howden, Proton pump inhibitor treatment for acute peptic ulcer bleeding, Cochrane Database Syst. Rev
Linsky, Gupta, Lawler, Fonda, Proton pump inhibitors and risk for recurrent Clostridium difficile Proton pump inhibitors in cirrhotic patients ©FUNPEC-RP www.funpecrp.com, br Genetics and Molecular Research
Liver, EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis, J. Hepatol
Mandorfer, Bota, Schwabl, Bucsics, Proton pump inhibitor treatment is neither associated with spontaneous bacterial peritonitis development nor with mortality in cirrhotic patients with ascites, J. Hepatol
Merli, Lucidi, Gregorio, Giannelli, The chronic use of beta-blockers and proton pump inhibitors may affect the rate of bacterial infections in cirrhosis, Liver Int
Min, Lim, Min, Gwak, Proton pump inhibitor use significantly increases the risk of spontaneous bacterial peritonitis in 1965 patients with cirrhosis and ascites: a propensity score matched cohort study, Aliment. Pharmacol. Ther
Miura, Tanaka, Yamamoto, Adachi, Proton pump inhibitor use is associated with spontaneous bacterial peritonitis in patients with liver cirrhosis, Intern. Med
Moher, Liberati, Tetzlaff, Altman, Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement, PLoS Med
Northup, Argo, Berg, Chronic proton pump inhibitor use is strongly associated with hepatorenal syndrome and spontaneous bacterial peritonitis in cirrhosis patients, Hepatology
O'leary, Reddy, Wong, Kamath, Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis, Clin. Gastroenterol. Hepatol
Ratelle, Perreault, Villeneuve, Tremblay, Association between proton pump inhibitor use and spontaneous bacterial peritonitis in cirrhotic patients with ascites, Can. J. Gastroenterol. Hepatol
Ratuapli, Ellington, Neill, Umar, Proton pump inhibitor therapy use does not predispose to small intestinal bacterial overgrowth, Am. J. Gastroenterol
Siple, Morey, Gutman, Weinberg, Proton pump inhibitor use and association with spontaneous bacterial peritonitis in patients with cirrhosis and ascites, Ann. Pharmacother
Terg, Casciato, Garbe, Cartier, Proton pump inhibitor therapy does not increase the incidence of bacterial infection in decompensated cirrhotic patients. A nationwide multicenter, prospective study, Hepatology
Trikudanathan, Israel, Cappa, Sullivan, Association between proton pump inhibitors and spontaneous bacterial peritonitis in cirrhotic patients -a systematic review and meta-analysis, Int. J. Clin. Pract
Van Vlerken, Huisman, Van Hoek, Renooij, Bacterial infections in cirrhosis: role of proton pump inhibitors and intestinal permeability, Eur. J. Clin. Invest
Wells, Shea, Connell, Peterson, The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses
Zedtwitz-Liebenstein, Wenisch, Patruta, Parschalk, Omeprazole treatment diminishes intra-and extracellular neutrophil reactive oxygen production and bactericidal activity, Crit. Care Med
DOI record:
{
"DOI": "10.4238/2015.july.3.25",
"ISSN": [
"1676-5680"
],
"URL": "http://dx.doi.org/10.4238/2015.July.3.25",
"author": [
{
"affiliation": [],
"family": "Xu",
"given": "H.B.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Wang",
"given": "H.D.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "C.H.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ye",
"given": "S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dong",
"given": "M.S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xia",
"given": "Q.J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "A.Q.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pan",
"given": "K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ge",
"given": "X.L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dong",
"given": "J.H.",
"sequence": "additional"
}
],
"container-title": "Genetics and Molecular Research",
"container-title-short": "Genet. Mol. Res.",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2015,
7,
6
]
],
"date-time": "2015-07-06T10:01:04Z",
"timestamp": 1436176864000
},
"deposited": {
"date-parts": [
[
2019,
2,
1
]
],
"date-time": "2019-02-01T08:53:22Z",
"timestamp": 1549011202000
},
"indexed": {
"date-parts": [
[
2024,
9,
10
]
],
"date-time": "2024-09-10T19:48:46Z",
"timestamp": 1725997726544
},
"is-referenced-by-count": 72,
"issue": "3",
"issued": {
"date-parts": [
[
2015
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2015
]
]
}
},
"link": [
{
"URL": "http://www.funpecrp.com.br/gmr/year2015/vol14-3/pdf/gmr5624.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "2758",
"original-title": [],
"page": "7490-7501",
"prefix": "10.4238",
"published": {
"date-parts": [
[
2015
]
]
},
"published-online": {
"date-parts": [
[
2015
]
]
},
"publisher": "Genetics and Molecular Research",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://www.funpecrp.com.br/gmr/year2015/vol14-3/pdf/gmr5624.pdf"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Proton pump inhibitor use and risk of spontaneous bacterial peritonitis in cirrhotic patients: a systematic review and meta-analysis",
"type": "journal-article",
"volume": "14"
}