The association between zinc deficiency, and clinical outcomes of COVID-19
et al., Journal of Infection, doi:10.1016/j.jinf.2023.06.021, Jun 2023
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
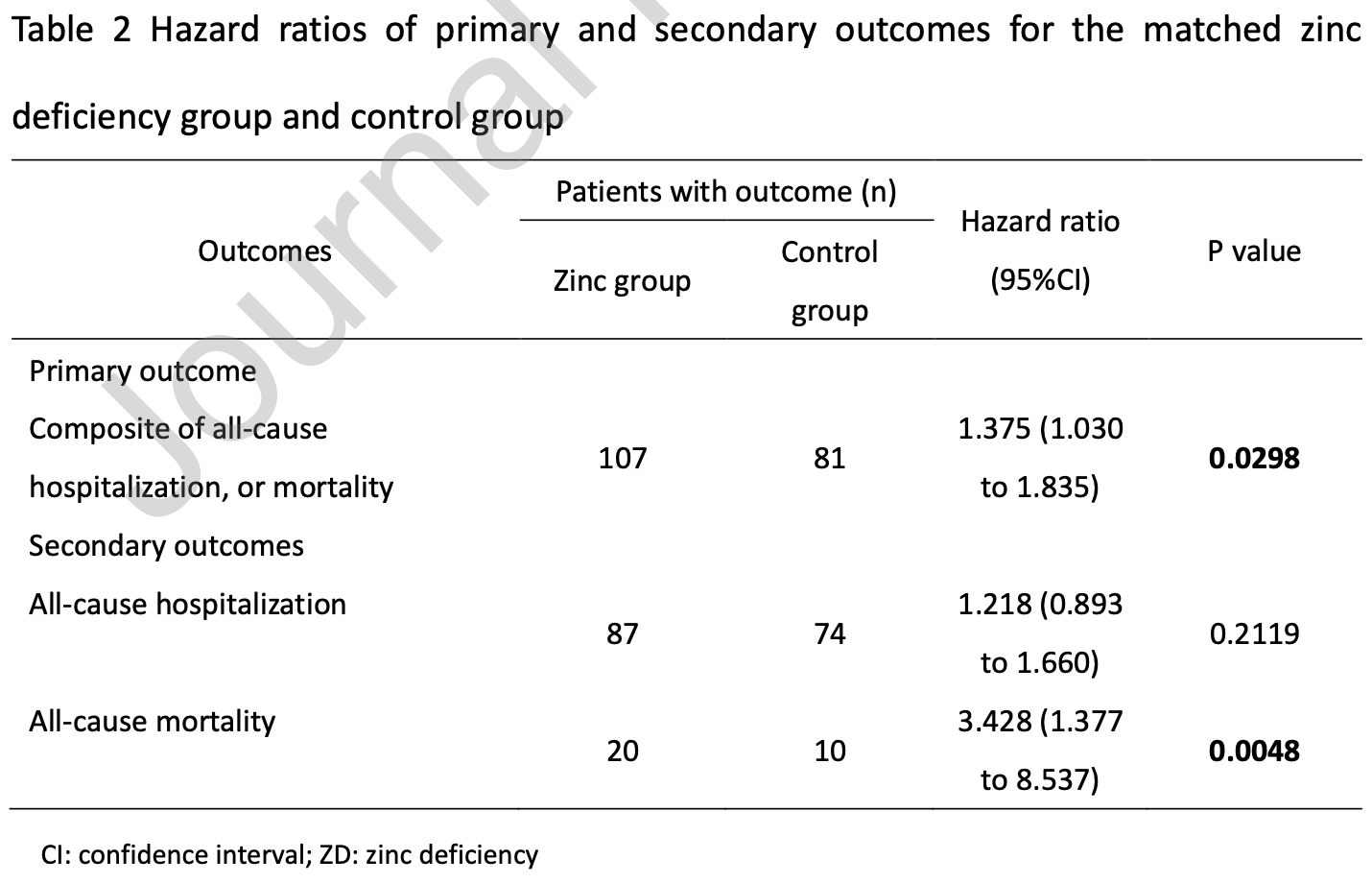
TriNetX PSM retrospective 10,935 COVID-19 patients, showing higher mortality with zinc deficiency.
|
risk of death, 70.8% lower, HR 0.29, p = 0.005, high zinc levels (≥70µg/dL) 10 of 1,447 (0.7%), low zinc levels (<70µg/dL) 20 of 1,447 (1.4%), inverted to make HR<1 favor high zinc levels (≥70µg/dL), Kaplan-Meier.
|
|
risk of death/hospitalization, 27.3% lower, HR 0.73, p = 0.03, high zinc levels (≥70µg/dL) 81 of 1,447 (5.6%), low zinc levels (<70µg/dL) 107 of 1,447 (7.4%), NNT 56, inverted to make HR<1 favor high zinc levels (≥70µg/dL), Kaplan-Meier.
|
|
risk of hospitalization, 17.9% lower, HR 0.82, p = 0.21, high zinc levels (≥70µg/dL) 74 of 1,447 (5.1%), low zinc levels (<70µg/dL) 87 of 1,447 (6.0%), NNT 111, inverted to make HR<1 favor high zinc levels (≥70µg/dL), Kaplan-Meier.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Wu et al., 29 Jun 2023, retrospective, multiple countries, peer-reviewed, 9 authors, study period 1 January, 2022 - 30 April, 2023.
Contact: m880419@mail.chimei.org.tw, nicolar930@gmail.com, rositatsai@gmail.com, andy10271@gmail.com, liu.tingkle@gmail.com, b0807246@gmail.com, 60028a@gmail.com, wayne54019@gmail.com, dtmed141@gmail.com.
The association between zinc deficiency, and clinical outcomes of COVID-19
Journal of Infection, doi:10.1016/j.jinf.2023.06.021
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest All authors declared there was no conflict of interests
Declaration of Competing Interest We have submitted our manuscript entitled, "The association between zinc deficiency, and clinical outcomes of COVID-19", to Journal of Infection for publication. We will not submit this paper to any another journal. All the authors have read the final version of the manuscript and have agreed to its content. All of the authors also declared that there was no conflict of interests.
References
Berger, Shenkin, Schweinlin, ESPEN micronutrient guideline, Clinical Nutrition
Chang, Liu, Wu, Lai, The association between corticosteroids and aspergillosis among COVID-19 patients, J Infect
Hsu, Shiau, Tsai, The effect of molnupiravir on post-acute outcome of COVID-19 survivors, J Infect
Jayawardena, Sooriyaarachchi, Chourdakis, Jeewandara, None
Jothimani, Kailasam, Danielraj, COVID-19: Poor outcomes in patients with zinc deficiency, Int J Infect Dis. Nov
Tabatabaeizadeh, Zinc supplementation and COVID-19 mortality: a metaanalysis, Eur J Med Res
Trinetx, None
Wu, Liu, Huang, Tsai, Lai, The effect of zinc on the outcome of patients with COVID-19: A systematic review and meta-analysis of randomized controlled trials, J Infect
Wu, Liu, Liu, Clinical efficacy of nirmatrelvir and ritonavir combination for treating diabetic patients with COVID-19, J Med Virol
DOI record:
{
"DOI": "10.1016/j.jinf.2023.06.021",
"ISSN": [
"0163-4453"
],
"URL": "http://dx.doi.org/10.1016/j.jinf.2023.06.021",
"alternative-id": [
"S0163445323003432"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "The association between zinc deficiency, and clinical outcomes of COVID-19"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Infection"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jinf.2023.06.021"
},
{
"label": "Content Type",
"name": "content_type",
"value": "simple-article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 Published by Elsevier Ltd on behalf of The British Infection Association."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-3290-1909",
"affiliation": [],
"authenticated-orcid": false,
"family": "Wu",
"given": "Jheng-Yan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hsu",
"given": "Wan-Hsuan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tsai",
"given": "Ya-Wen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Ting-Hui",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Po-Yu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chuang",
"given": "Min-Hsiang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chin",
"given": "Szu-En",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6334-2388",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lai",
"given": "Chih-Cheng",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3760-1945",
"affiliation": [],
"authenticated-orcid": false,
"family": "Liu",
"given": "Mei-Yuan",
"sequence": "additional"
}
],
"container-title": "Journal of Infection",
"container-title-short": "Journal of Infection",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"journalofinfection.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
6,
29
]
],
"date-time": "2023-06-29T15:47:07Z",
"timestamp": 1688053627000
},
"deposited": {
"date-parts": [
[
2023,
6,
29
]
],
"date-time": "2023-06-29T15:47:12Z",
"timestamp": 1688053632000
},
"indexed": {
"date-parts": [
[
2023,
6,
30
]
],
"date-time": "2023-06-30T04:42:50Z",
"timestamp": 1688100170724
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
6
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
1
]
],
"date-time": "2023-06-01T00:00:00Z",
"timestamp": 1685577600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0163445323003432?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0163445323003432?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
6
]
]
},
"published-print": {
"date-parts": [
[
2023,
6
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/j.jinf.2023.01.023",
"article-title": "The effect of zinc on the outcome of patients with COVID-19: A systematic review and meta-analysis of randomized controlled trials",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "e142",
"issue": "5",
"journal-title": "J Infect",
"key": "10.1016/j.jinf.2023.06.021_bib1",
"volume": "86",
"year": "2023"
},
{
"DOI": "10.1186/s40001-022-00694-z",
"article-title": "Zinc supplementation and COVID-19 mortality: a meta-analysis",
"author": "Tabatabaeizadeh",
"doi-asserted-by": "crossref",
"first-page": "70",
"issue": "1",
"journal-title": "Eur J Med Res",
"key": "10.1016/j.jinf.2023.06.021_bib2",
"volume": "27",
"year": "2022"
},
{
"key": "10.1016/j.jinf.2023.06.021_bib3",
"unstructured": "TriNetX. Available at: 〈https://trinetx.com/〉. Accessed June 22, 2023."
},
{
"DOI": "10.1016/j.jinf.2023.03.016",
"article-title": "The effect of molnupiravir on post-acute outcome of COVID-19 survivors",
"author": "Hsu",
"doi-asserted-by": "crossref",
"journal-title": "J Infect",
"key": "10.1016/j.jinf.2023.06.021_bib4",
"year": "2023"
},
{
"DOI": "10.1016/j.ijid.2020.09.014",
"article-title": "COVID-19: Poor outcomes in patients with zinc deficiency",
"author": "Jothimani",
"doi-asserted-by": "crossref",
"first-page": "343",
"journal-title": "Int J Infect Dis",
"key": "10.1016/j.jinf.2023.06.021_bib5",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2023.01.034",
"article-title": "The association between corticosteroids and aspergillosis among COVID-19 patients",
"author": "Chang",
"doi-asserted-by": "crossref",
"first-page": "394",
"issue": "4",
"journal-title": "J Infect",
"key": "10.1016/j.jinf.2023.06.021_bib6",
"volume": "86",
"year": "2023"
},
{
"DOI": "10.1002/jmv.28866",
"article-title": "Clinical efficacy of nirmatrelvir and ritonavir combination for treating diabetic patients with COVID-19",
"author": "Wu",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "J Med Virol",
"key": "10.1016/j.jinf.2023.06.021_bib7",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.1016/j.clnu.2022.02.015",
"article-title": "ESPEN micronutrient guideline",
"author": "Berger",
"doi-asserted-by": "crossref",
"first-page": "1357",
"issue": "6",
"journal-title": "Clinical Nutrition",
"key": "10.1016/j.jinf.2023.06.021_bib8",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.1016/j.dsx.2020.04.015",
"article-title": "Enhancing immunity in viral infections, with special emphasis on COVID-19: A review",
"author": "Jayawardena",
"doi-asserted-by": "crossref",
"first-page": "367",
"issue": "4",
"journal-title": "Diabetes Metab Syndr. Jul-",
"key": "10.1016/j.jinf.2023.06.021_bib9",
"volume": "14",
"year": "2020"
}
],
"reference-count": 9,
"references-count": 9,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0163445323003432"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Microbiology (medical)"
],
"subtitle": [],
"title": "The association between zinc deficiency, and clinical outcomes of COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}
