Impact of risk for severe COVID-19 illness on physical activity during the pandemic
et al., Heart & Lung, doi:10.1016/j.hrtlng.2023.05.002, May 2023
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
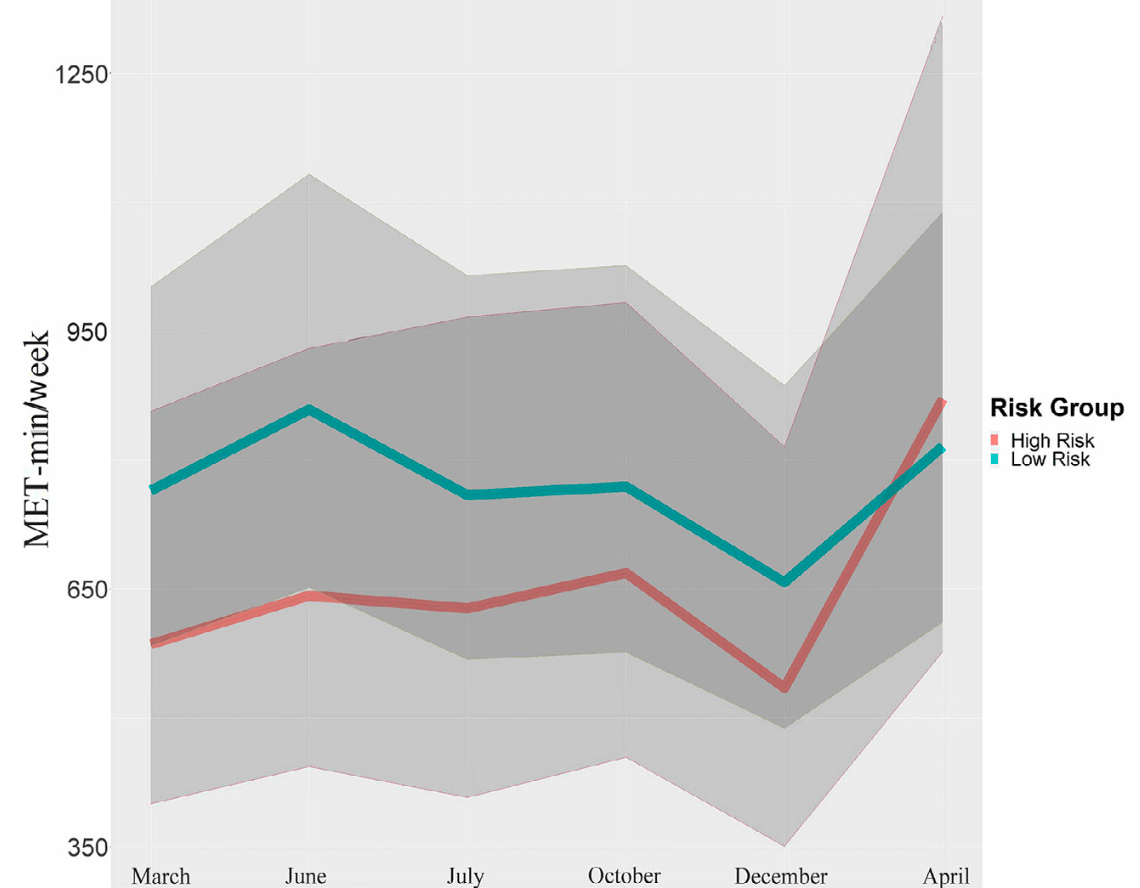
Analysis of 640 adults in the USA, showing that adults at high risk of severe COVID-19 were disproportionately more likely to be physically inactive and had lower activity levels during the early months of the pandemic.
Wierenga et al., 8 May 2023, USA, peer-reviewed, survey, mean age 42.7, 9 authors.
Contact: kwiereng@iu.edu.
Impact of risk for severe COVID-19 illness on physical activity during the pandemic
Heart & Lung, doi:10.1016/j.hrtlng.2023.05.002
Background: Precautions to mitigate spread of COVID-19 such as the closing of exercise facilities impacted physical activity behaviors. Varied risks for severe COVID-19 may have influenced participation in regular physical activity to maintain precautions. Objective: Describe differences in the amount and intensity of physical activity between adults at high versus low risk for severe COVID-19 illness during the pandemic. We hypothesized that over 13 months, 1) highrisk adults would have greater odds of inactivity than low-risk adults, and 2) when active, high-risk adults would have lower metabolic equivalent of task minutes (MET-min) than low-risk adults. Methods: This longitudinal observational cohort study surveyed U.S. adults' demographics, health history, and physical activity beginning March 2020 using REDCap. Using self-report, health history was assessed with a modified Charlson Comorbidity Index and physical activity with the International Physical Activity Questionnaire. Repeated physical activity measurements were conducted in June, July, October, and December of 2020, and in April of 2021. Two models, a logistic model evaluating physical inactivity (hypothesis 1) and a gamma model evaluating total MET-min for physically active individuals (hypothesis 2), were used. Models were controlled for age, gender, and race. Results: The final sample consisted of 640 participants (mean age 42.7 § 15.7, 78% women, 90% white), with n = 175 categorized as high-risk and n = 465 as low-risk. The odds of inactivity for the high-risk adults were 2.8 to 4.1 times as high than for low-risk adults at baseline and 13 months. Active high-risk adults had lower MET-min levels than low-risk adults in March (28%, p = 0.001), June (29%, p = 0.002), and July of 2020 (30%, p = 0.005) only. Conclusions: Adults at high risk of severe COVID-19 illness were disproportionately more likely to be physically inactive and exhibit lower MET-min levels than adults at low risk during the early months of the COVID-19 pandemic.
References
Accessed, None
Barek, Aziz, Islam, Impact of age, sex, comorbidities and clinical symptoms on the severity of COVID-19 cases: a meta-analysis with 55 studies and 10014 cases, Heliyon, doi:10.1016/j.heliyon.2020.e05684
Boukrim, Obtel, Kasouati, Achbani, Razine, COVID-19 and confinement: effect on weight load, physical activity and eating behavior of higher education students in Southern Morocco, Ann Glob Health, doi:10.5334/aogh.3144
Cameron, Stinson, Gender (mis)measurement: guidelines for respecting gender diversity in psychological research, Soc Personal Psychol Compass, doi:10.1111/spc3.12506
Caputo, Reichert, Studies of physical activity and COVID-19 during the pandemic: a scoping review, J Phys Act Health, doi:10.1123/jpah.2020-0406
Cary, None
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis, doi:10.1016/0021-9681(87)90171-8
Corrado, Magnano, Muzii, Effects of social distancing on psychological state and physical activity routines during the COVID-19 pandemic, Sport Sci Health, doi:10.1007/s11332-020-00697-5
Craig, Marshall, International physical activity questionnaire: 12-country reliability and validity, Med Sci Sports Exerc, doi:10.1249/01.MSS.0000078924.61453.FB
Cusack, Individual, social, and environmental factors associated with active transportation commuting during the COVID-19 pandemic, J Transp Health, doi:10.1016/j.jth.2021.101089
Dennis, Cook, James, Wheater, Lindley, Relationships between health outcomes in older populations and urban green infrastructure size, quality and proximity, doi:10.1186/s12889-020-08762-x
Fernandez, How Many Gyms Survived the Devastation that Was 2020? The Global Health & Fitness Association; 2021
Flanagan, Beyl, Fearnbach, Altazan, Martin et al., The impact of COVID-19 stay-at-home orders on health behaviors in adults, Obesity, doi:10.1002/oby.23066
Harish, The syndemics of emergency: how COVID-19 demands a holistic view of public health promotion and preparedness, Am J Public Health, doi:10.2105/AJPH.2020.306116
Harris, Taylor, Minor, The REDCap consortium: building an international community of software platform partners, J Biomed Inform, doi:10.1016/j.jbi.2019.103208
Ibm Corp, IBM SPSS Statistics for Windows, Version 27
Kim, Vakula, Bolton, Which exercise interventions can most effectively improve reactive balance in older adults? A systematic review and network meta-analysis, Front Aging Neurosci, doi:10.3389/fnagi.2021.764826
Koster, Stenholm, Schrack, The Palgrave Handbook of Ageing and Physical Activity Promotion
Park, Zhong, Yang, Jeong, Lee, Impact of COVID-19 on physical activity: a rapid review, J Glob Health, doi:10.7189/jogh.12.05003
Penedo, Dahn, Exercise and well-being: a review of mental and physical health benefits associated with physical activity, Curr Opin Psychiatry
Salman, Beaney, Robb, Impact of social restrictions during the COVID-19 pandemic on the physical activity levels of adults aged 50À92 years: a baseline survey of the CHARIOT COVID-19 Rapid Response prospective cohort study, BMJ Open, doi:10.1136/bmjopen-2021-050680
Sebastião, Steffens, Nakamura, Papini, Perceptions on activity behavior during the COVID-19 pandemic "second wave" among US adults: results of a short online survey, Sport Sci Health, doi:10.1007/s11332-021-00813-z
Shao, Lai, Chen, Chen, Hung et al., Prevalence, incidence and mortality of delirium in patients with COVID-19: a systematic review and meta-analysis, Age Ageing, doi:10.1093/ageing/afab103
Smith, How Many Health Clubs, Gyms, and Studios Closed in 2021. The Global Health & Fitness Association
Stamatakis, Gale, Bauman, Ekelund, Hamer et al., Sitting time, physical activity, and risk of mortality in adults, J Am Coll Cardiol, doi:10.1016/j.jacc.2019.02.031
Stockwell, Trott, Tully, Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review, BMJ Open Sport Exerc Med, doi:10.1136/bmjsem-2020-000960
Tsao, Aday, Almarzooq, Heart Disease and Stroke Statistics-2023 update: a report from the American Heart Association, Circulation, doi:10.1161/CIR.0000000000001123
Tucker, Gilliland, The effect of season and weather on physical activity: a systematic review, Public Health, doi:10.1016/j.puhe.2007.04.009
Wierenga, Moore, Pressler, Hacker, Perkins, Associations between COVID-19 perceptions, anxiety, and depressive symptoms among adults living in the United States, Nurs Outlook, doi:10.1016/j.outlook.2021.03.020
Xu, Gu, Cai, The effects of exercise for cognitive function in older adults: a systematic review and meta-analysis of randomized controlled trials, Int J Environ Res Public Health, doi:10.3390/ijerph20021088
DOI record:
{
"DOI": "10.1016/j.hrtlng.2023.05.002",
"ISSN": [
"0147-9563"
],
"URL": "http://dx.doi.org/10.1016/j.hrtlng.2023.05.002",
"alternative-id": [
"S0147956323001176"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Impact of risk for severe COVID-19 illness on physical activity during the pandemic"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Heart & Lung"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.hrtlng.2023.05.002"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 Elsevier Inc. All rights reserved."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-2298-2602",
"affiliation": [],
"authenticated-orcid": false,
"family": "Wierenga",
"given": "Kelly L.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Perkins",
"given": "Susan M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Forster",
"given": "Anna K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alwine",
"given": "Jennifer",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ofner",
"given": "Susan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mulkey",
"given": "Malissa A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hacker",
"given": "Eileen Danaher",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pressler",
"given": "Susan J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moore",
"given": "Scott Emory",
"sequence": "additional"
}
],
"container-title": "Heart & Lung",
"container-title-short": "Heart & Lung",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"heartandlung.org",
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.com.au",
"clinicalkey.es",
"clinicalkey.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
5,
8
]
],
"date-time": "2023-05-08T07:35:32Z",
"timestamp": 1683531332000
},
"deposited": {
"date-parts": [
[
2023,
5,
15
]
],
"date-time": "2023-05-15T19:01:40Z",
"timestamp": 1684177300000
},
"funder": [
{
"DOI": "10.13039/100008113",
"doi-asserted-by": "publisher",
"name": "Indiana University Purdue University Indianapolis"
},
{
"DOI": "10.13039/100006733",
"doi-asserted-by": "publisher",
"name": "Indiana University"
}
],
"indexed": {
"date-parts": [
[
2023,
5,
16
]
],
"date-time": "2023-05-16T14:40:04Z",
"timestamp": 1684248004283
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
9
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
1
]
],
"date-time": "2023-09-01T00:00:00Z",
"timestamp": 1693526400000
}
},
{
"URL": "https://doi.org/10.15223/policy-017",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
1
]
],
"date-time": "2023-09-01T00:00:00Z",
"timestamp": 1693526400000
}
},
{
"URL": "https://doi.org/10.15223/policy-037",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
1
]
],
"date-time": "2023-09-01T00:00:00Z",
"timestamp": 1693526400000
}
},
{
"URL": "https://doi.org/10.15223/policy-012",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
1
]
],
"date-time": "2023-09-01T00:00:00Z",
"timestamp": 1693526400000
}
},
{
"URL": "https://doi.org/10.15223/policy-029",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
1
]
],
"date-time": "2023-09-01T00:00:00Z",
"timestamp": 1693526400000
}
},
{
"URL": "https://doi.org/10.15223/policy-004",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
1
]
],
"date-time": "2023-09-01T00:00:00Z",
"timestamp": 1693526400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0147956323001176?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0147956323001176?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "84-91",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
9
]
]
},
"published-print": {
"date-parts": [
[
2023,
9
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"key": "10.1016/j.hrtlng.2023.05.002_bib0001",
"series-title": "How to Protect Yourself and Others",
"year": "2022"
},
{
"key": "10.1016/j.hrtlng.2023.05.002_bib0002",
"series-title": "People With Certain Medical Conditions",
"year": "2022"
},
{
"DOI": "10.1123/jpah.2020-0406",
"article-title": "Studies of physical activity and COVID-19 during the pandemic: a scoping review",
"author": "Caputo",
"doi-asserted-by": "crossref",
"first-page": "1275",
"issue": "12",
"journal-title": "J Phys Act Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0003",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1136/bmjsem-2020-000960",
"article-title": "Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review",
"author": "Stockwell",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "BMJ Open Sport Exerc Med",
"key": "10.1016/j.hrtlng.2023.05.002_bib0004",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1007/s11332-020-00697-5",
"article-title": "Effects of social distancing on psychological state and physical activity routines during the COVID-19 pandemic",
"author": "Di Corrado",
"doi-asserted-by": "crossref",
"first-page": "619",
"issue": "4",
"journal-title": "Sport Sci Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0005",
"volume": "16",
"year": "2020"
},
{
"key": "10.1016/j.hrtlng.2023.05.002_bib0006",
"unstructured": "Fernandez KA. How Many Gyms Survived the Devastation that Was 2020? The Global Health & Fitness Association; 2021. Published August 5, 2021. Accessed January 19, 2023. https://www.ihrsa.org/improve-your-club/industry-news/how-many-gyms-survived-the-devastation-that-was-2020/."
},
{
"DOI": "10.1002/oby.23066",
"article-title": "The impact of COVID-19 stay-at-home orders on health behaviors in adults",
"author": "Flanagan",
"doi-asserted-by": "crossref",
"first-page": "438",
"issue": "2",
"journal-title": "Obesity",
"key": "10.1016/j.hrtlng.2023.05.002_bib0007",
"volume": "29",
"year": "2021"
},
{
"key": "10.1016/j.hrtlng.2023.05.002_bib0008",
"unstructured": "U.S. Department of Health and Human Services. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Published February, 2018. Accessed January 19, 2023. https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf."
},
{
"DOI": "10.1016/j.jacc.2019.02.031",
"article-title": "Sitting time, physical activity, and risk of mortality in adults",
"author": "Stamatakis",
"doi-asserted-by": "crossref",
"first-page": "2062",
"issue": "16",
"journal-title": "J Am Coll Cardiol",
"key": "10.1016/j.hrtlng.2023.05.002_bib0009",
"volume": "73",
"year": "2019"
},
{
"DOI": "10.1161/CIR.0000000000001123",
"article-title": "Heart Disease and Stroke Statistics-2023 update: a report from the American Heart Association",
"author": "Tsao",
"doi-asserted-by": "crossref",
"first-page": "e93",
"issue": "8",
"journal-title": "Circulation",
"key": "10.1016/j.hrtlng.2023.05.002_bib0010",
"volume": "147",
"year": "2023"
},
{
"DOI": "10.3390/ijerph20021088",
"article-title": "The effects of exercise for cognitive function in older adults: a systematic review and meta-analysis of randomized controlled trials",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "1088",
"issue": "2",
"journal-title": "Int J Environ Res Public Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0011",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.3389/fnagi.2021.764826",
"article-title": "Which exercise interventions can most effectively improve reactive balance in older adults? A systematic review and network meta-analysis",
"author": "Kim",
"doi-asserted-by": "crossref",
"journal-title": "Front Aging Neurosci",
"key": "10.1016/j.hrtlng.2023.05.002_bib0012",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.2105/AJPH.2020.306116",
"article-title": "The syndemics of emergency: how COVID-19 demands a holistic view of public health promotion and preparedness",
"author": "Harish",
"doi-asserted-by": "crossref",
"first-page": "353",
"issue": "3",
"journal-title": "Am J Public Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0013",
"volume": "111",
"year": "2021"
},
{
"DOI": "10.1007/978-3-319-71291-8_3",
"article-title": "The benefits of physical activity for older people",
"author": "Koster",
"doi-asserted-by": "crossref",
"first-page": "43",
"issue": "2",
"journal-title": "The Palgrave Handbook of Ageing and Physical Activity Promotion",
"key": "10.1016/j.hrtlng.2023.05.002_bib0014",
"volume": "18",
"year": "2018"
},
{
"DOI": "10.1097/00001504-200503000-00013",
"article-title": "Exercise and well-being: a review of mental and physical health benefits associated with physical activity",
"author": "Penedo",
"doi-asserted-by": "crossref",
"first-page": "189",
"issue": "2",
"journal-title": "Curr Opin Psychiatry",
"key": "10.1016/j.hrtlng.2023.05.002_bib0015",
"volume": "18",
"year": "2005"
},
{
"key": "10.1016/j.hrtlng.2023.05.002_bib0016",
"series-title": "CDC Museum COVID-19 Timeline",
"year": "2022"
},
{
"DOI": "10.1016/j.outlook.2021.03.020",
"article-title": "Associations between COVID-19 perceptions, anxiety, and depressive symptoms among adults living in the United States",
"author": "Wierenga",
"doi-asserted-by": "crossref",
"first-page": "755",
"issue": "5",
"journal-title": "Nurs Outlook",
"key": "10.1016/j.hrtlng.2023.05.002_bib0017",
"volume": "69",
"year": "2021"
},
{
"DOI": "10.1111/spc3.12506",
"article-title": "Gender (mis)measurement: guidelines for respecting gender diversity in psychological research",
"author": "Cameron",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "Soc Personal Psychol Compass",
"key": "10.1016/j.hrtlng.2023.05.002_bib0018",
"volume": "13",
"year": "2019"
},
{
"DOI": "10.1016/j.jbi.2019.103208",
"article-title": "The REDCap consortium: building an international community of software platform partners",
"author": "Harris",
"doi-asserted-by": "crossref",
"journal-title": "J Biomed Inform",
"key": "10.1016/j.hrtlng.2023.05.002_bib0019",
"volume": "95",
"year": "2019"
},
{
"DOI": "10.1249/01.MSS.0000078924.61453.FB",
"article-title": "International physical activity questionnaire: 12-country reliability and validity",
"author": "Craig",
"doi-asserted-by": "crossref",
"first-page": "1381",
"issue": "8",
"journal-title": "Med Sci Sports Exerc",
"key": "10.1016/j.hrtlng.2023.05.002_bib0020",
"volume": "35",
"year": "2003"
},
{
"key": "10.1016/j.hrtlng.2023.05.002_bib0021",
"series-title": "Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19: Information for Healthcare Professionals. Underlying Medical Conditions",
"year": "2020"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"article-title": "A new method of classifying prognostic comorbidity in longitudinal studies: development and validation",
"author": "Charlson",
"doi-asserted-by": "crossref",
"first-page": "373",
"issue": "5",
"journal-title": "J Chronic Dis",
"key": "10.1016/j.hrtlng.2023.05.002_bib0022",
"volume": "40",
"year": "1987"
},
{
"key": "10.1016/j.hrtlng.2023.05.002_bib0023",
"unstructured": "IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp"
},
{
"key": "10.1016/j.hrtlng.2023.05.002_bib0024",
"unstructured": "SAS Institute Inc. Released 2013. SAS, Version 9.4. Cary, NC: SAS Institute Inc"
},
{
"key": "10.1016/j.hrtlng.2023.05.002_bib0025",
"unstructured": "U.S. Department of Homeland Security Cybersecurity & Infrasturcture Sercurity Agency. Guidance on the Essential Critical Infrastructure Workforce: Ensuring Community and National Resilience in COVID-19 Response, Version 3.0. Published April 17, 2020. Accessed January 19, 2023.https://www.cisa.gov/sites/default/files/publications/Version_3.0_CISA_Guidance_on_Essential_Critical_Infrastructure_Workers_1.pdf."
},
{
"DOI": "10.1093/ageing/afab103",
"article-title": "Prevalence, incidence and mortality of delirium in patients with COVID-19: a systematic review and meta-analysis",
"author": "Shao",
"doi-asserted-by": "crossref",
"first-page": "1445",
"issue": "5",
"journal-title": "Age Ageing",
"key": "10.1016/j.hrtlng.2023.05.002_bib0026",
"volume": "50",
"year": "2021"
},
{
"DOI": "10.1016/j.heliyon.2020.e05684",
"article-title": "Impact of age, sex, comorbidities and clinical symptoms on the severity of COVID-19 cases: a meta-analysis with 55 studies and 10014 cases",
"author": "Barek",
"doi-asserted-by": "crossref",
"issue": "12",
"journal-title": "Heliyon",
"key": "10.1016/j.hrtlng.2023.05.002_bib0027",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.5334/aogh.3144",
"article-title": "COVID-19 and confinement: effect on weight load, physical activity and eating behavior of higher education students in Southern Morocco",
"author": "Boukrim",
"doi-asserted-by": "crossref",
"first-page": "7",
"issue": "1",
"journal-title": "Ann Glob Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0028",
"volume": "87",
"year": "2021"
},
{
"DOI": "10.1016/j.jth.2021.101089",
"article-title": "Individual, social, and environmental factors associated with active transportation commuting during the COVID-19 pandemic",
"author": "Cusack",
"doi-asserted-by": "crossref",
"journal-title": "J Transp Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0029",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1136/bmjopen-2021-050680",
"article-title": "Impact of social restrictions during the COVID-19 pandemic on the physical activity levels of adults aged 50–92 years: a baseline survey of the CHARIOT COVID-19 Rapid Response prospective cohort study",
"author": "Salman",
"doi-asserted-by": "crossref",
"issue": "8",
"journal-title": "BMJ Open",
"key": "10.1016/j.hrtlng.2023.05.002_bib0030",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.7189/jogh.12.05003",
"article-title": "Impact of COVID-19 on physical activity: a rapid review",
"author": "Park",
"doi-asserted-by": "crossref",
"first-page": "05003",
"journal-title": "J Glob Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0031",
"volume": "12",
"year": "2022"
},
{
"author": "Smith",
"key": "10.1016/j.hrtlng.2023.05.002_bib0032",
"series-title": "How Many Health Clubs, Gyms, and Studios Closed in 2021",
"year": "2022"
},
{
"DOI": "10.1007/s11332-021-00813-z",
"article-title": "Perceptions on activity behavior during the COVID-19 pandemic “second wave” among US adults: results of a short online survey",
"author": "Sebastião",
"doi-asserted-by": "crossref",
"first-page": "267",
"issue": "1",
"journal-title": "Sport Sci Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0033",
"volume": "18",
"year": "2022"
},
{
"DOI": "10.1016/j.puhe.2007.04.009",
"article-title": "The effect of season and weather on physical activity: a systematic review",
"author": "Tucker",
"doi-asserted-by": "crossref",
"first-page": "909",
"issue": "12",
"journal-title": "Public Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0034",
"volume": "121",
"year": "2007"
},
{
"DOI": "10.1186/s12889-020-08762-x",
"article-title": "Relationships between health outcomes in older populations and urban green infrastructure size, quality and proximity",
"author": "Dennis",
"doi-asserted-by": "crossref",
"first-page": "1",
"issue": "1",
"journal-title": "BMC Public Health",
"key": "10.1016/j.hrtlng.2023.05.002_bib0035",
"volume": "20",
"year": "2020"
}
],
"reference-count": 35,
"references-count": 35,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0147956323001176"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cardiology and Cardiovascular Medicine",
"Critical Care and Intensive Care Medicine",
"Pulmonary and Respiratory Medicine"
],
"subtitle": [],
"title": "Impact of risk for severe COVID-19 illness on physical activity during the pandemic",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "61"
}
