Risk factors of SARS-CoV-2 infection in healthcare workers: a retrospective study of a nosocomial outbreak
et al., Sleep Medicine: X, doi:10.1016/j.sleepx.2020.100028, Dec 2020
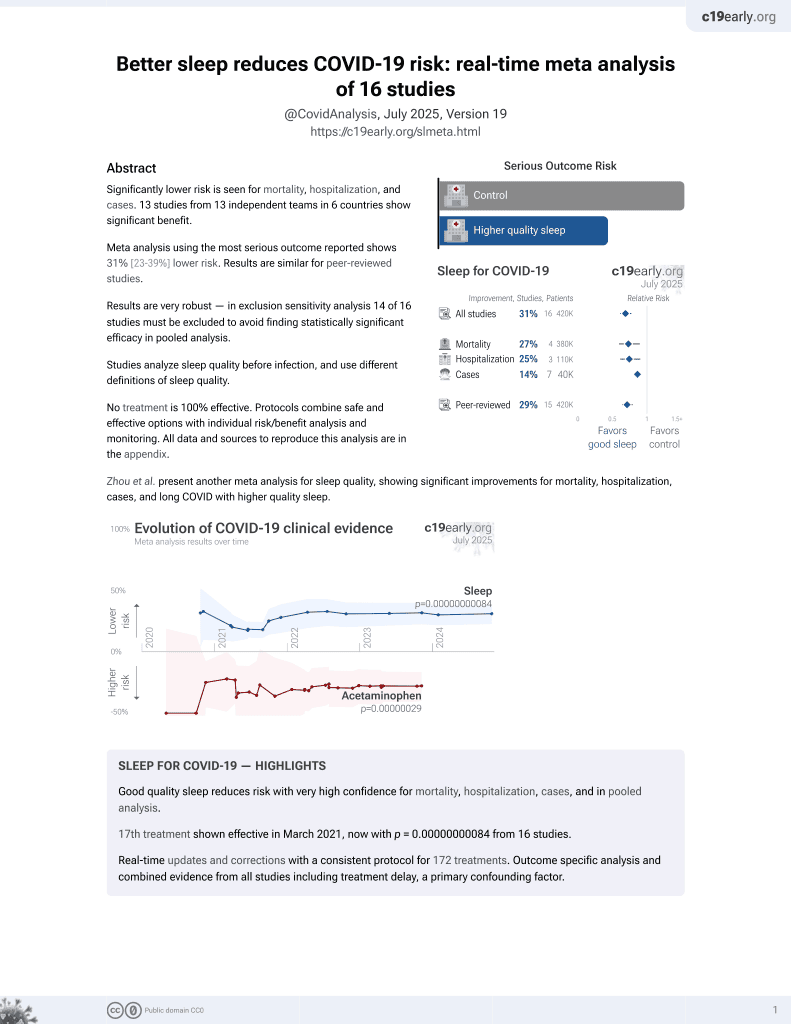
Sleep for COVID-19
18th treatment shown to reduce risk in
March 2021, now with p = 0.00000000084 from 16 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 118 healthcare workers in China, showing higher risk of COVID-19 with poor sleep quality.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
This study is excluded in meta-analysis:
results only provided with respect to continuous values.
|
risk of case, 66.3% lower, HR 0.34, p < 0.001, inverted to make HR<1 favor improved sleep, Cox proportional hazards, model 2.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Wang et al., 31 Dec 2020, retrospective, China, peer-reviewed, survey, mean age 19.0, 14 authors, study period 6 January, 2020 - 8 January, 2020.
Contact: hyzhao750@sina.com, baiyansen6@hust.edu.cn.
Risk factors of SARS-CoV-2 infection in healthcare workers: a retrospective study of a nosocomial outbreak
Sleep Medicine: X, doi:10.1016/j.sleepx.2020.100028
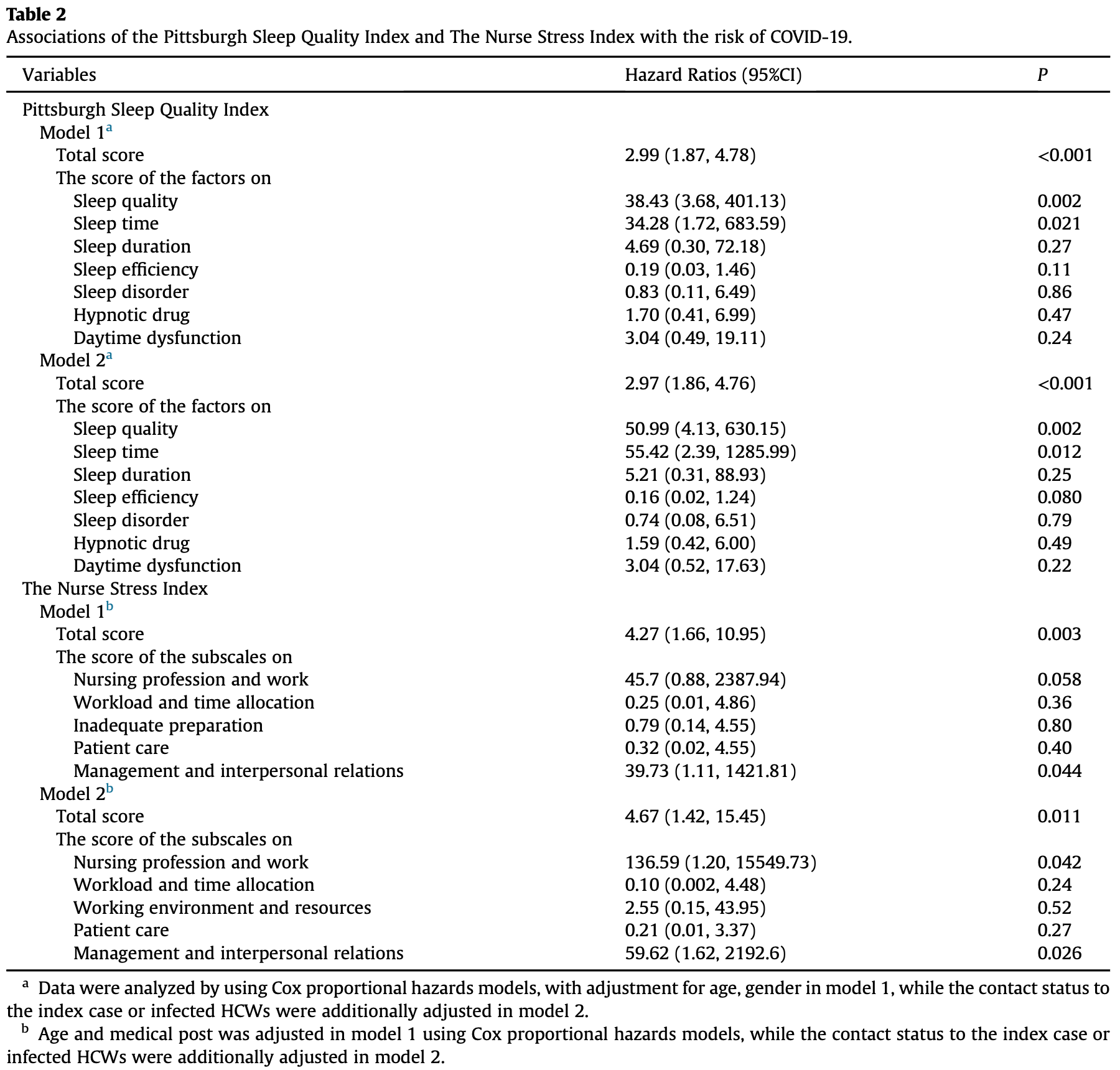
Background: Healthcare workers (HCWs) are at the forefront of fighting against the COVID-19 pandemic. However, they are at high risk of acquiring the pathogen from infected patients and transmitting to other HCWs. We aimed to investigate risk factors for nosocomial COVID-19 infection among HCWs in a non-COVID-19 hospital yard. Methods: Retrospective data collection on demographics, lifestyles, contact status with infected subjects for 118 HCWs (including 12 COVID-19 HCWs) at Union Hospital of Wuhan, China. Sleep quality and working pressure were evaluated by the Pittsburgh Sleep Quality Index (PSQI) and The Nurse Stress Index (NSI), respectively. The follow-up duration was from Dec 25, 2019, to Feb 15, 2020. Results: A high proportion of COVID-19 HCWs had engaged in night shift-work (75.0% vs. 40.6%) and felt working under pressure (66.7% vs. 32.1%) than uninfected HCWs. SARS-CoV-2 infected HCWs had significantly higher scores of PSQI and NSI than uninfected HCWs (P < 0.001). Specifically, scores of 5 factors (sleep quality, sleep time, sleep efficiency, sleep disorder, and daytime dysfunction) in PSQI were higher among infected HCWs. For NSI, its 5 subscales (nursing profession and work, workload and time allocation, working environment and resources, patient care, management and interpersonal relations) were all higher in infected than uninfected nurse. Furthermore, total scores of PSQI (HR ¼ 2.97, 95% CI ¼ 1.86À4.76; P <0.001) and NSI (HR ¼ 4.67, 95%CI ¼ 1.42À15.45; P ¼ 0.011) were both positively associated with the risk of SARS-CoV-2 infection. Conclusion: Our analysis shows that poor sleep quality and higher working pressure may increase the risk of nosocomial SARS-CoV-2 infection among HCWs.
Ethics approval and consent to participate This study was approved by the institutional ethics board of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (No. 20200029), and all participants provided their informed consent.
Consent for publication Consent for publication had been obtained from all studied participants.
Credit author statement Xuan Wang; Conceptualization, Methodology, Software, Data curation, Writing -original draft, Xiaobing Jiang; Supervision,
Conflict of interest The authors declare that they have no competing interests. The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleepx.2020.100028.
Appendix A. Supplementary data Supplementary data to this article can be found online at https://doi.org/10.1016/j.sleepx.2020.100028.
References
Bardhan, Heaton, Davis, A cross sectional study evaluating psychosocial job stress and health risk in emergency department nurses, Int J Environ Res Publ Health, doi:10.3390/ijerph16183243
Bartoszko, Farooqi, Alhazzani, Medical masks vs N95 respirators for preventing COVID-19 in healthcare workers: a systematic review and meta-analysis of randomized trials, Influenza Other Respir Viruses, doi:10.1111/irv.12745
Besedovsky, Lange, Haack, The sleep-immune crosstalk in health and disease, Physiol Rev, doi:10.1152/physrev.00010.2018
Buysse, Reynolds 3rd, Monk, The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research, Psychiatr Res, doi:10.1016/0165-1781(89)90047-4
Chen, Liang, Li, Mental health care for medical staff in China during the COVID-19 outbreak, Lancet Psychiatry, doi:10.1016/s2215-0366(20)30078-x
Gold, Covid-19: adverse mental health outcomes for healthcare workers, BMJ, doi:10.1136/bmj.m1815
Huang, Huo, Ruan, Optimal control of environmental cleaning and antibiotic prescription in an epidemiological model of methicillin-resistant Staphylococcus aureus infections in hospitals, Math Biosci, doi:10.1016/j.mbs.2019.01.013
Jr, The adverse effects of psychological stress on immunoregulatory balance: applications to human inflammatory diseases, Immunol Allergy Clin, doi:10.1016/j.iac.2010.09.013
Lancet, COVID-19: protecting health-care workers, Lancet, doi:10.1016/s0140-6736(20)30644-9
Mullen, Mengozzi, Hanschmann, How the redox state regulates immunity, Free Radic Biol Med, doi:10.1016/j.freeradbiomed.2019.12.022
Pamela, James, The nursing stress scale: development of an instrument, J Behav Assess, doi:10.1007/BF01321348
Prather, Leung, Association of insufficient sleep with respiratory infection among adults in the United States, JAMA Intern Med, doi:10.1001/jamainternmed.2016.0787
Ran, Chen, Wang, Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China, Clin Infect Dis, doi:10.1093/cid/ciaa287
Salgado, Farr, Hall, Influenza in the acute hospital setting, Lancet Infect Dis, doi:10.1016/s1473-3099(02)00221-9
Shen, Zou, Zhong, Psychological stress of ICU nurses in the time of COVID-19, Crit Care, doi:10.1186/s13054-020-02926-2
Skowronski, Astell, Brunham, Severe acute respiratory syndrome (SARS): a year in review, Annu Rev Med, doi:10.1146/annurev.med.56.091103.134135
Wang, Jiang, Huang, None, Sleep Medicine: X
Wang, Xie, Xu, Sleep disturbances among medical workers during the outbreak of COVID-2019, Occup Med, doi:10.1093/occmed/kqaa074
Wang, Zhou, He, Nosocomial outbreak of 2019 novel coronavirus pneumonia in Wuhan, China, Eur Respir J, doi:10.1183/13993003.00544-2020
DOI record:
{
"DOI": "10.1016/j.sleepx.2020.100028",
"ISSN": [
"2590-1427"
],
"URL": "http://dx.doi.org/10.1016/j.sleepx.2020.100028",
"alternative-id": [
"S2590142720300173"
],
"article-number": "100028",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Risk factors of SARS-CoV-2 infection in healthcare workers: a retrospective study of a nosocomial outbreak"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Sleep Medicine: X"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.sleepx.2020.100028"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2020 The Authors. Published by Elsevier B.V."
}
],
"author": [
{
"affiliation": [],
"family": "Wang",
"given": "Xuan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Jiang",
"given": "Xiaobing",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Qimin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Han",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gurarie",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ndeffo-Mbah",
"given": "Martial",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fan",
"given": "Fei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fu",
"given": "Peng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Horn",
"given": "Mary Ann",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4100-2366",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mondal",
"given": "Anirban",
"sequence": "additional"
},
{
"affiliation": [],
"family": "King",
"given": "Charles",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xu",
"given": "Shuai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhao",
"given": "Hongyang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bai",
"given": "Yansen",
"sequence": "additional"
}
],
"container-title": "Sleep Medicine: X",
"container-title-short": "Sleep Medicine: X",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2020,
10,
14
]
],
"date-time": "2020-10-14T07:34:53Z",
"timestamp": 1602660893000
},
"deposited": {
"date-parts": [
[
2020,
12,
18
]
],
"date-time": "2020-12-18T21:26:29Z",
"timestamp": 1608326789000
},
"funder": [
{
"DOI": "10.13039/501100012226",
"award": [
"2020kfyXGYJ010"
],
"doi-asserted-by": "publisher",
"name": "Fundamental Research Funds for the Central Universities"
},
{
"award": [
"DEB-2028631"
],
"name": "National Science Foundation RAPID"
},
{
"award": [
"DEB-2028632"
],
"name": "National Science Foundation RAPID"
}
],
"indexed": {
"date-parts": [
[
2022,
11,
11
]
],
"date-time": "2022-11-11T15:30:03Z",
"timestamp": 1668180603853
},
"is-referenced-by-count": 19,
"issued": {
"date-parts": [
[
2020,
12
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
12,
1
]
],
"date-time": "2020-12-01T00:00:00Z",
"timestamp": 1606780800000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
10,
9
]
],
"date-time": "2020-10-09T00:00:00Z",
"timestamp": 1602201600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2590142720300173?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2590142720300173?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "100028",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2020,
12
]
]
},
"published-print": {
"date-parts": [
[
2020,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/S1473-3099(02)00221-9",
"article-title": "Influenza in the acute hospital setting",
"author": "Salgado",
"doi-asserted-by": "crossref",
"first-page": "145",
"journal-title": "Lancet Infect Dis",
"key": "10.1016/j.sleepx.2020.100028_bib1",
"volume": "2",
"year": "2002"
},
{
"DOI": "10.1146/annurev.med.56.091103.134135",
"article-title": "Severe acute respiratory syndrome (SARS): a year in review",
"author": "Skowronski",
"doi-asserted-by": "crossref",
"first-page": "357",
"journal-title": "Annu Rev Med",
"key": "10.1016/j.sleepx.2020.100028_bib2",
"volume": "56",
"year": "2005"
},
{
"DOI": "10.1016/j.mbs.2019.01.013",
"article-title": "Optimal control of environmental cleaning and antibiotic prescription in an epidemiological model of methicillin-resistant Staphylococcus aureus infections in hospitals",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "13",
"journal-title": "Math Biosci",
"key": "10.1016/j.sleepx.2020.100028_bib3",
"volume": "311",
"year": "2019"
},
{
"article-title": "The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China",
"first-page": "145",
"journal-title": "Zhonghua Liuxingbingxue Zazhi",
"key": "10.1016/j.sleepx.2020.100028_bib4",
"volume": "41",
"year": "2020"
},
{
"article-title": "Nosocomial outbreak of 2019 novel coronavirus pneumonia in Wuhan, China",
"author": "Wang",
"journal-title": "Eur Respir J",
"key": "10.1016/j.sleepx.2020.100028_bib5",
"year": "2020"
},
{
"article-title": "COVID-19: protecting health-care workers",
"author": "The Lancet",
"first-page": "922",
"journal-title": "Lancet",
"key": "10.1016/j.sleepx.2020.100028_bib6",
"volume": "395",
"year": "2020"
},
{
"key": "10.1016/j.sleepx.2020.100028_bib7",
"series-title": "Spain reports 462 more deaths in one day",
"year": "2020"
},
{
"DOI": "10.1016/S2215-0366(20)30078-X",
"article-title": "Mental health care for medical staff in China during the COVID-19 outbreak",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "e15",
"journal-title": "Lancet Psychiatry",
"key": "10.1016/j.sleepx.2020.100028_bib8",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/0165-1781(89)90047-4",
"article-title": "The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research",
"author": "Buysse",
"doi-asserted-by": "crossref",
"first-page": "193",
"journal-title": "Psychiatr Res",
"key": "10.1016/j.sleepx.2020.100028_bib9",
"volume": "28",
"year": "1989"
},
{
"article-title": "The nursing stress scale: development of an instrument",
"author": "Pamela",
"first-page": "11",
"journal-title": "J Behav Assess",
"key": "10.1016/j.sleepx.2020.100028_bib10",
"volume": "3",
"year": "1981"
},
{
"DOI": "10.1093/occmed/kqaa074",
"article-title": "Sleep disturbances among medical workers during the outbreak of COVID-2019",
"author": "Wang",
"doi-asserted-by": "crossref",
"journal-title": "Occup Med (Lond)",
"key": "10.1016/j.sleepx.2020.100028_bib11",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2016.0787",
"article-title": "Association of insufficient sleep with respiratory infection among adults in the United States",
"author": "Prather",
"doi-asserted-by": "crossref",
"first-page": "850",
"journal-title": "JAMA Intern Med",
"key": "10.1016/j.sleepx.2020.100028_bib12",
"volume": "176",
"year": "2016"
},
{
"DOI": "10.1152/physrev.00010.2018",
"article-title": "The sleep-immune crosstalk in health and disease",
"author": "Besedovsky",
"doi-asserted-by": "crossref",
"first-page": "1325",
"journal-title": "Physiol Rev",
"key": "10.1016/j.sleepx.2020.100028_bib13",
"volume": "99",
"year": "2019"
},
{
"DOI": "10.1093/cid/ciaa287",
"article-title": "Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China",
"author": "Ran",
"doi-asserted-by": "crossref",
"journal-title": "Clin Infect Dis",
"key": "10.1016/j.sleepx.2020.100028_bib14",
"year": "2020"
},
{
"DOI": "10.3390/ijerph16183243",
"article-title": "A cross sectional study evaluating psychosocial job stress and health risk in emergency department nurses",
"author": "Bardhan",
"doi-asserted-by": "crossref",
"journal-title": "Int J Environ Res Publ Health",
"key": "10.1016/j.sleepx.2020.100028_bib15",
"volume": "16",
"year": "2019"
},
{
"article-title": "How the redox state regulates immunity",
"author": "Mullen",
"journal-title": "Free Radic Biol Med",
"key": "10.1016/j.sleepx.2020.100028_bib16",
"year": "2019"
},
{
"DOI": "10.1136/bmj.m1815",
"article-title": "Covid-19: adverse mental health outcomes for healthcare workers",
"author": "Gold",
"doi-asserted-by": "crossref",
"first-page": "m1815",
"journal-title": "BMJ",
"key": "10.1016/j.sleepx.2020.100028_bib17",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1016/j.iac.2010.09.013",
"article-title": "The adverse effects of psychological stress on immunoregulatory balance: applications to human inflammatory diseases",
"author": "Marshall",
"doi-asserted-by": "crossref",
"first-page": "133",
"journal-title": "Immunol Allergy Clin",
"key": "10.1016/j.sleepx.2020.100028_bib18",
"volume": "31",
"year": "2011"
},
{
"DOI": "10.1111/irv.12745",
"article-title": "Medical masks vs N95 respirators for preventing COVID-19 in healthcare workers: a systematic review and meta-analysis of randomized trials",
"author": "Bartoszko",
"doi-asserted-by": "crossref",
"journal-title": "Influenza Other Respir Viruses",
"key": "10.1016/j.sleepx.2020.100028_bib19",
"year": "2020"
},
{
"DOI": "10.1186/s13054-020-02926-2",
"article-title": "Psychological stress of ICU nurses in the time of COVID-19",
"author": "Shen",
"doi-asserted-by": "crossref",
"first-page": "200",
"journal-title": "Crit Care",
"key": "10.1016/j.sleepx.2020.100028_bib20",
"volume": "24",
"year": "2020"
}
],
"reference-count": 20,
"references-count": 20,
"relation": {
"has-preprint": [
{
"asserted-by": "object",
"id": "10.1101/2020.03.29.20047159",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2590142720300173"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Risk factors of SARS-CoV-2 infection in healthcare workers: a retrospective study of a nosocomial outbreak",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "2"
}