Neurological Complications of COVID-19: Unraveling the Pathophysiological Underpinnings and Therapeutic Implications
et al., Viruses, doi:10.3390/v16081183, Jul 2024
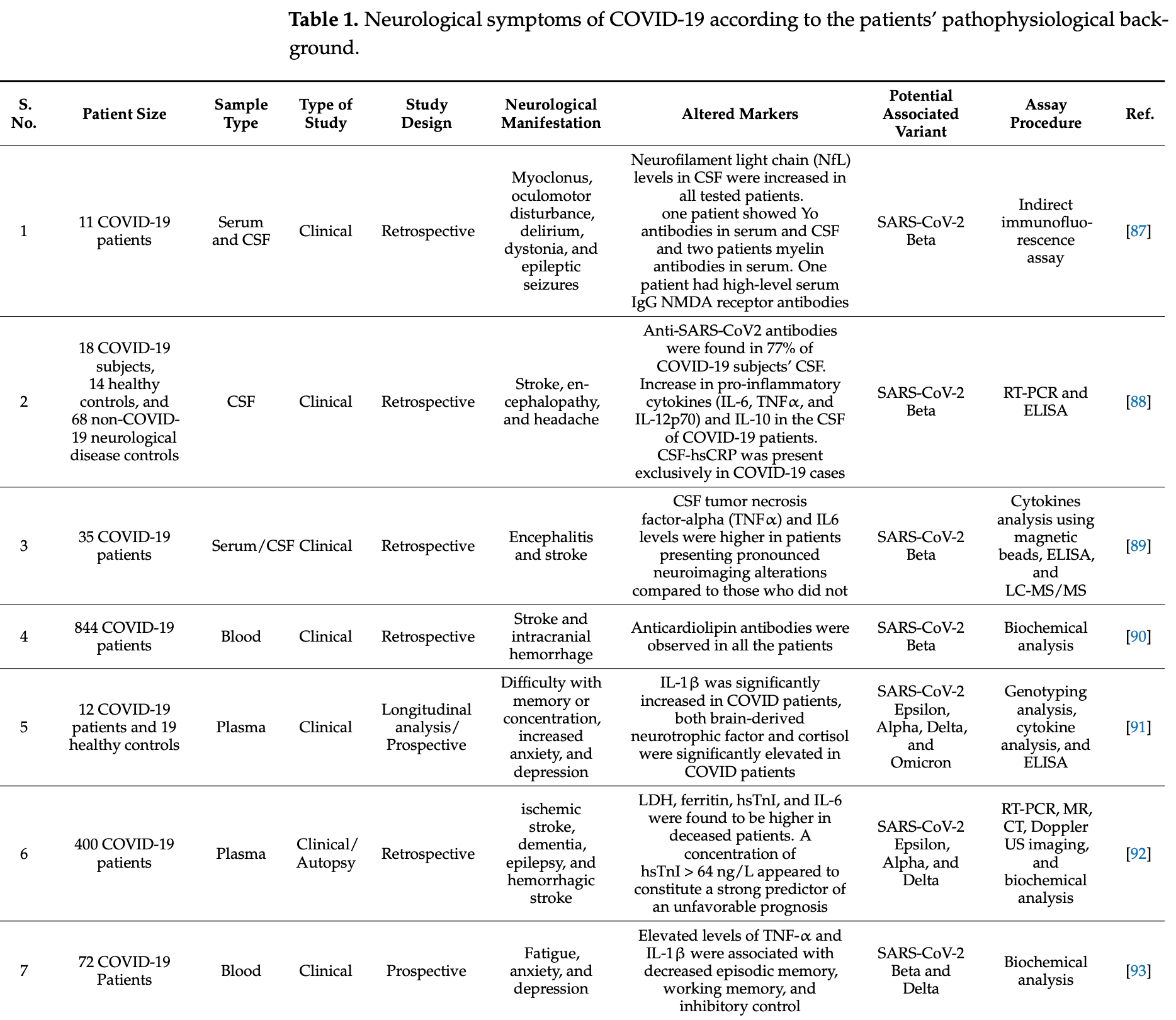
Review of the neurological complications of COVID-19 and their pathophysiological underpinnings and therapeutic implications. Authors note that SARS-CoV-2 infection can lead to a range of neurological complications such as anosmia, stroke, paralysis, cranial nerve deficits, encephalopathy, delirium, meningitis, seizures, and more. The virus may enter the nervous system via several potential routes, including the blood-brain barrier, retrograde axonal transport, the gastrointestinal tract, and infected immune cells. Different SARS-CoV-2 variants have been associated with varying incidences of neurological disorders. At the molecular level, severe COVID-19 can induce epigenetic changes resembling natural aging and trigger synapse elimination and cytokine upregulation in microglia cells.
Vashisht et al., 24 Jul 2024, peer-reviewed, 9 authors.
Contact: rkolhe@augusta.edu (corresponding author), avashisht@augusta.edu, vvashisht@augusta.edu, hsingh1@augusta.edu, pahluwalia@augusta.edu, amondal@augusta.edu, jfarmaha@augusta.edu, jawoodall@augusta.edu, colin.williams@lmunet.edu.
Neurological Complications of COVID-19: Unraveling the Pathophysiological Underpinnings and Therapeutic Implications
Viruses, doi:10.3390/v16081183
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease (COVID-19), induced a global pandemic with a diverse array of clinical manifestations. While the acute phase of the pandemic may be waning, the intricacies of COVID-19 s impact on neurological health remain a crucial area of investigation. Early recognition of the spectrum of COVID-19 symptoms, ranging from mild fever and cough to life-threatening respiratory distress and multi-organ failure, underscored the significance of neurological complications, including anosmia, seizures, stroke, disorientation, encephalopathy, and paralysis. Notably, patients requiring intensive care unit (ICU) admission due to neurological challenges or due to them exhibiting neurological abnormalities in the ICU have shown increased mortality rates. COVID-19 can lead to a range of neurological complications such as anosmia, stroke, paralysis, cranial nerve deficits, encephalopathy, delirium, meningitis, seizures, etc., in affected patients. This review elucidates the burgeoning landscape of neurological sequelae associated with SARS-CoV-2 infection and explores the underlying neurobiological mechanisms driving these diverse manifestations. A meticulous examination of potential neuroinvasion routes by SARS-CoV-2 underscores the intricate interplay between the virus and the nervous system. Moreover, we dissect the diverse neurological manifestations emphasizing the necessity of a multifaceted approach to understanding the disease's neurological footprint. In addition to elucidating the pathophysiological underpinnings, this review surveys current therapeutic modalities and delineates prospective avenues for neuro-COVID research. By integrating epidemiological, clinical, and diagnostic parameters, we endeavor to foster a comprehensive analysis of the nexus between COVID-19 and neurological health, thereby laying the groundwork for targeted therapeutic interventions and long-term management strategies.
Author Contributions: Conceptualization, A.V. and R.K.; Formal analysis, A.V., V.V., H.S. and P.A.; Writing-original draft preparation, A.V., V.V., H.S. and P.A.; Writing-review and editing, A.K.M., C.W., J.F. and J.W.; Supervision, R.K. All authors have read and agreed to the published version of the manuscript. Funding: This research received no external funding.
Conflicts of Interest: The authors declare no conflicts of interest. Viruses 2024, 16, 1183
References
Aggarwal, Garcia-Telles, Aggarwal, Lavie, Lippi et al., Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): Early report from the United States, Diagnosis, doi:10.1515/dx-2020-0046
Aladawi, Elfil, Abu-Esheh, Jazar, Armouti et al., Guillain Barre syndrome as a complication of COVID-19: A systematic review, Can. J. Neurol. Sci, doi:10.1017/cjn.2021.102
Aleem, Akbar Samad, Vaqar, Emerging Variants of SARS-CoV-2 and Novel Therapeutics against Coronavirus (COVID-19)
Arbour, Day, Newcombe, Talbot, Neuroinvasion by human respiratory coronaviruses, J. Virol, doi:10.1128/JVI.74.19.8913-8921.2000
Barros-Aragão, Pinto, Carregari, Rezende, Pinheiro et al., Changes in neuroinflammatory biomarkers correlate with disease severity and neuroimaging alterations in patients with COVID-19 neurological complications, Brain Behav. Immun. Health, doi:10.1016/j.bbih.2024.100805
Beacon, Su, Lakowski, Delcuve, Davie, SARS-CoV-2 multifaceted interaction with the human host. Part II: Innate immunity response, immunopathology, and epigenetics, IUBMB Life, doi:10.1002/iub.2379
Beltrán-Corbellini, Chico-García, Martínez-Poles, Rodríguez-Jorge, Natera-Villalba et al., Acute-onset smell and taste disorders in the context of COVID-19: A pilot multicentre polymerase chain reaction based case-control study, Eur. J. Neurol, doi:10.1111/ene.14273
Beretta, Cristillo, Camera, Morotti Colleoni, Pellitteri et al., Incidence and long-term functional outcome of neurologic disorders in hospitalized patients with COVID-19 infected with pre-omicron variants, Neurology, doi:10.1212/WNL.0000000000207534
Bergmann, Lane, Stohlman, Coronavirus infection of the central nervous system: Host-virus stand-off, Nat. Rev. Microbiol, doi:10.1038/nrmicro1343
Biswas, Das Sarma, Effect of microtubule disruption on neuronal spread and replication of demyelinating and nondemyelinating strains of mouse hepatitis virus in vitro, J. Virol, doi:10.1128/JVI.02545-13
Bost, Giladi, Liu, Bendjelal, Xu et al., Host-viral infection maps reveal signatures of severe COVID-19 patients, Cell, doi:10.1016/j.cell.2020.05.006
Boucher, Desforges, Duquette, Talbot, Long-term human coronavirus-myelin cross-reactive T-cell clones derived from multiple sclerosis patients, Clin. Immunol, doi:10.1016/j.clim.2007.02.002
Bryce, Grimes, Pujadas, Ahuja, Beasley et al., Pathophysiology of SARS-CoV-2: Targeting of endothelial cells renders a complex disease with thrombotic microangiopathy and aberrant immune response. The Mount Sinai COVID-19 autopsy experience, medRxiv, doi:10.1101/2020.05.18.20099960
Cabirac, Soike, Butunoi, Hoel, Johnson et al., Coronavirus JHM OMP1 pathogenesis in owl monkey CNS and coronavirus infection of owl monkey CNS via peripheral routes
Cantuti-Castelvetri, Ojha, Pedro, Djannatian, Franz et al., Neuropilin-1 facilitates SARS-CoV-2 cell entry and provides a possible pathway into the central nervous system, bioRxiv, doi:10.1101/2020.06.07.137802
Chakraborty, Bhattacharya, Sharma, Present variants of concern and variants of interest of severe acute respiratory syndrome coronavirus 2: Their significant mutations in S-glycoprotein, infectivity, re-infectivity, immune escape and vaccines activity, Rev. Med. Virol, doi:10.1002/rmv.2270
Chen, Wang, Yu, Howard, French et al., The spatial and cell-type distribution of SARS-CoV-2 receptor ACE2 in the human and mouse brains, Front. Neurol, doi:10.3389/fneur.2020.573095
Chen, Wu, Chen, Yan, Yang et al., Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study, BMJ, doi:10.1136/bmj.m1091
Crow, Olferiev, Kirou, Type I interferons in autoimmune disease, Annu. Rev. Pathol. Mech. Dis, doi:10.1146/annurev-pathol-020117-043952
Cuenca-Zaldivar, Monroy Acevedo, Fernández-Carnero, Sánchez-Romero, Villafañe et al., Effects of a Multicomponent Exercise Program on Improving Frailty in Post-COVID-19 Older Adults after Intensive Care Units: A Single-Group Retrospective Cohort Study, Biology, doi:10.3390/biology11071084
De Melo, Perraud, Alvarez, Vieites-Prado, Kim et al., Neuroinvasion and anosmia are independent phenomena upon infection with SARS-CoV-2 and its variants, Nat. Commun, doi:10.1038/s41467-023-40228-7
Ding, He, Zhang, Huang, Che et al., Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: Implications for pathogenesis and virus transmission pathways, J. Pathol. A J. Pathol. Soc. Great Br. Irel, doi:10.1002/path.1560
Engelhardt, Vajkoczy, Weller, The movers and shapers in immune privilege of the CNS, Nat. Immunol, doi:10.1038/ni.3666
Erickson, Banks, Neuroimmune axes of the blood-brain barriers and blood-brain interfaces: Bases for physiological regulation, disease states, and pharmacological interventions, Pharmacol. Rev, doi:10.1124/pr.117.014647
Escalard, Maïer, Redjem, Delvoye, Hébert et al., Treatment of acute ischemic stroke due to large vessel occlusion with COVID-19: Experience from Paris, Stroke, doi:10.1161/STROKEAHA.120.030574
Favas, Dev, Chaurasia, Chakravarty, Mishra et al., Neurological manifestations of COVID-19: A systematic review and meta-analysis of proportions, Neurol. Sci, doi:10.1007/s10072-020-04801-y
Feng, Diao, Wang, Wang, Wang et al., SARS-CoV-2) directly decimates human spleens and lymph nodes, doi:10.1101/2020.03.27.20045427
Fenrich, Mrdenovic, Balog, Tomic, Zjalic et al., SARS-CoV-2 dissemination through peripheral nerves explains multiple organ injury, Front. Cell. Neurosci, doi:10.3389/fncel.2020.00229
Fierz, Multiple sclerosis: An example of pathogenic viral interaction?, Virol. J, doi:10.1186/s12985-017-0719-3
Franke, Ferse, Kreye, Reincke, Sanchez-Sendin et al., High frequency of cerebrospinal fluid autoantibodies in COVID-19 patients with neurological symptoms, Brain Behav. Immun, doi:10.1016/j.bbi.2020.12.022
Frontera, Simon, Bridging Knowledge Gaps in the Diagnosis and Management of Neuropsychiatric Sequelae of COVID-19, JAMA Psychiatry, doi:10.1001/jamapsychiatry.2022.1616
Gaebler, Wang, Lorenzi, Muecksch, Finkin et al., Evolution of antibody immunity to SARS-CoV-2, Nature, doi:10.1038/s41586-021-03207-w
Ganji, Reddy, Impact of COVID-19 on mitochondrial-based immunity in aging and age-related diseases, Front. Aging Neurosci, doi:10.3389/fnagi.2020.614650
Ggarcia, Barreras, Lewis, Pinilla, Sokoll et al., Cerebrospinal fluid in COVID-19 neurological complications: No cytokine storm or neuroinflammation, medRxiv, doi:10.1101/2021.01.10.20249014
Glezer, Rivest, Oncostatin M is a novel glucocorticoid-dependent neuroinflammatory factor that enhances oligodendrocyte precursor cell activity in demyelinated sites, Brain Behav. Immun, doi:10.1016/j.bbi.2010.01.005
Gowrisankar, Clark, Angiotensin II regulation of angiotensin-converting enzymes in spontaneously hypertensive rat primary astrocyte cultures, J. Neurochem, doi:10.1111/jnc.13641
Gu, Gong, Zhang, Zheng, Gao et al., Multiple organ infection and the pathogenesis of SARS, J. Exp. Med, doi:10.1084/jem.20050828
Haber, Sejvar, Mikaeloff, Destefano, Vaccines and guillain-barre syndrome, Drug Saf, doi:10.2165/00002018-200932040-00005
Hamming, Timens, Bulthuis, Lely, Navis et al., Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, J. Pathol. A J. Pathol. Soc. Great Br. Irel, doi:10.1002/path.1570
He, Mäe, Sun, Muhl, Nahar et al., Pericytespecific vascular expression of SARS-CoV-2 receptor ACE2-implications for microvascular inflammation and hypercoagulopathy in COVID-19 patients, bioRxiv, doi:10.1101/2020.05.11.088500
Helms, Kremer, Merdji, Clere-Jehl, Schenck et al., Neurologic features in severe SARS-CoV-2 infection, N. Engl. J. Med, doi:10.1056/NEJMc2008597
Jacomy, Fragoso, Almazan, Mushynski, Talbot, Human coronavirus OC43 infection induces chronic encephalitis leading to disabilities in BALB/C mice, Virology, doi:10.1016/j.virol.2006.01.049
Kantonen, Mahzabin, Mäyränpää, Tynninen, Paetau et al., Neuropathologic features of four autopsied COVID-19 patients, Brain Pathol, doi:10.1111/bpa.12889
Kaur, Ling, The circumventricular organs, Histol. Histopathol
Kim, Heo, Kim, Song, Park et al., Neurological complications during treatment of Middle East respiratory syndrome, J. Clin. Neurol, doi:10.3988/jcn.2017.13.3.227
Kim, Kwon, Kam, Panicker, Karuppagounder et al., Transneuronal propagation of pathologic α-synuclein from the gut to the brain models Parkinson's disease, Neuron, doi:10.1016/j.neuron.2019.05.035
Lechien, Chiesa-Estomba, De Siati, Horoi, Le Bon et al., Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study, Eur. Arch. Oto-Rhino Laryngol, doi:10.1007/s00405-020-05965-1
Li, Bai, Hirano, Hayashida, Taniguchi et al., Neurotropic virus tracing suggests a membranous-coating-mediated mechanism for transsynaptic communication, J. Comp. Neurol, doi:10.1002/cne.23171
Li, Li, Wang, Zhou, Chang et al., Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study, Stroke Vasc. Neurol, doi:10.1136/svn-2020-000431
Li, Liu, Yang, Han, Mi et al., Neurological manifestations of patients with COVID-19: Potential routes of SARS-CoV-2 neuroinvasion from the periphery to the brain, Front. Med, doi:10.1007/s11684-020-0786-5
Liotta, Batra, Clark, Shlobin, Hoffman et al., Frequent neurologic manifestations and encephalopathy-associated morbidity in COVID-19 patients, Ann. Clin. Transl. Neurol, doi:10.1002/acn3.51210
Liu, Jin, Xiao, Zhong, Li, Inhibition of CD147 improves oligodendrogenesis and promotes white matter integrity and functional recovery in mice after ischemic stroke, Brain Behav. Immun, doi:10.1016/j.bbi.2019.07.027
Mao, Jin, Wang, Hu, Chen et al., Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China, JAMA Neurol, doi:10.1001/jamaneurol.2020.1127
Massion, Howa, Zhu, Kim, Halasa et al., Sex differences in COVID-19 symptom severity and trajectories among ambulatory adults, Influenza Other Respir. Viruses, doi:10.1111/irv.13235
Matsuda, Park, Sunden, Kimura, Ochiai et al., The vagus nerve is one route of transneural invasion for intranasally inoculated influenza a virus in mice, Vet. Pathol, doi:10.1354/vp.41-2-101
Mavrikaki, Lee, Solomon, Slack, Severe COVID-19 induces molecular signatures of aging in the human brain, Nat. Aging, doi:10.1038/s43587-022-00321-w
Merad, Martin, Pathological inflammation in patients with COVID-19: A key role for monocytes and macrophages, Nat. Rev. Immunol, doi:10.1038/s41577-020-0331-4
Mesci, Macia, Saleh, Martin-Sancho, Yin et al., Sofosbuvir protects human brain organoids against SARS-CoV-2, bioRxiv, doi:10.1101/2020.05.30.125856
Moein, Hashemian, Mansourafshar, Khorram-Tousi, Tabarsi et al., Smell dysfunction: A biomarker for COVID-19, Int. Forum Allergy Rhinol, doi:10.1002/alr.22587
Moriguchi, Harii, Goto, Harada, Sugawara et al., A first case of meningitis/encephalitis associated with SARS-Coronavirus-2, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.03.062
Nampoothiri, Sauve, Ternier, Fernandois, Coelho et al., The hypothalamus as a hub for putative SARS-CoV-2 brain infection, bioRxiv, doi:10.1101/2020.06.08.139329
Nyberg, Ferguson, Nash, Webster, Flaxman et al., Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B. 1.1. 529) and delta (B. 1.617. 2) variants in England: A cohort study, Lancet, doi:10.1016/S0140-6736(22)00462-7
O'brien, Forleo-Neto, Sarkar, Isa, Hou et al., Effect of subcutaneous casirivimab and imdevimab antibody combination vs placebo on development of symptomatic COVID-19 in early asymptomatic SARS-CoV-2 infection: A randomized clinical trial, JAMA, doi:10.1001/jama.2021.24939
Oxley, Mocco, Majidi, Kellner, Shoirah et al., Large-vessel stroke as a presenting feature of COVID-19 in the young, N. Engl. J. Med, doi:10.1056/NEJMc2009787
Paniz-Mondolfi, Bryce, Grimes, Gordon, Reidy et al., Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), J. Med. Virol, doi:10.1002/jmv.25915
Papatsiros, Stylianaki, Papakonstantinou, Papaioannou, Christodoulopoulos, Case report of transmissible gastroenteritis coronavirus infection associated with small intestine and brain lesions in piglets, Viral Immunol, doi:10.1089/vim.2018.0095
Paterson, Brown, Benjamin, Nortley, Wiethoff et al., The emerging spectrum of COVID-19 neurology: Clinical, radiological and laboratory findings, Brain, doi:10.1093/brain/awaa240
Pei, Wang, Zhang, Luo, Zhou, Association of frailty status with adverse clinical outcomes in patients with COVID-19: Protocol for a systematic review and dose-response meta-analysis, BMJ Open, doi:10.1136/bmjopen-2020-046980
Proust, Queval, Harvey, Adams, Bennett et al., Differential effects of SARS-CoV-2 variants on central nervous system cells and blood-brain barrier functions, J. Neuroinflamm, doi:10.1186/s12974-023-02861-3
Puntambekar, Hinton, Yin, Savarin, Bergmann et al., Interleukin-10 is a critical regulator of white matter lesion containment following viral induced demyelination, Glia, doi:10.1002/glia.22880
Ramani, Müller, Ostermann, Gabriel, Abida-Islam et al., SARS-CoV-2 targets neurons of 3D human brain organoids, EMBO J, doi:10.15252/embj.2020106230
Reichard, Kashani, Boire, Constantopoulos, Guo et al., Neuropathology of COVID-19: A spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology, Acta Neuropathol, doi:10.1007/s00401-020-02166-2
Rogers, Chesney, Oliver, Pollak, Mcguire et al., Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic, Lancet Psychiatry, doi:10.1016/S2215-0366(20)30203-0
Rothstein, Oldridge, Schwennesen, Do, Cucchiara, Acute cerebrovascular events in hospitalized COVID-19 patients, Stroke, doi:10.1161/STROKEAHA.120.030995
Samudyata, Oliveira, Malwade, Rufino De Sousa, Goparaju et al., SARS-CoV-2 promotes microglial synapse elimination in human brain organoids, Mol. Psychiatry, doi:10.1038/s41380-022-01786-2
Sanchis-Gomar, Lavie, Perez-Quilis, Henry, Lippi, Angiotensin-converting enzyme 2 and antihypertensives (angiotensin receptor blockers and angiotensin-converting enzyme inhibitors) in coronavirus disease 2019, Mayo Clin. Proc, doi:10.1016/j.mayocp.2020.03.026
Schaller, Hirschbühl, Burkhardt, Braun, Trepel et al., Postmortem examination of patients with COVID-19, JAMA, doi:10.1001/jama.2020.8907
Scheepers, Everatt, Amoako, Mnguni, Ismail et al., The continuous evolution of SARS-CoV-2 in South Africa: A new lineage with rapid accumulation of mutations of concern and global detection, medRxiv, doi:10.1101/2021.08.20.21262342
Siow, Lee, Zhang, Saffari, Ng, Encephalitis as neurological complication of COVID-19: A systematic review and meta-analysis of incidence, outcomes, and predictors, Eur. J. Neurol, doi:10.1111/ene.14913
Solomon, Normandin, Bhattacharyya, Mukerji, Keller et al., Neuropathological features of COVID-19, N. Engl. J. Med, doi:10.1056/NEJMc2019373
Song, Zhang, Israelow, Lu-Culligan, Sprado et al., Neuroinvasive potential of SARS-CoV-2 revealed in a human brain, J. Exp. Med, doi:10.1084/jem.20202135
Spinato, Fabbris, Polesel, Cazzador, Borsetto et al., Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection, JAMA, doi:10.1001/jama.2020.6771
Srikantha, Mohajeri, The possible role of the microbiota-gut-brain-axis in autism spectrum disorder, Int. J. Mol. Sci, doi:10.3390/ijms20092115
Streinu-Cercel, Săndulescu, Preotescu, Kim, Kim et al., -controlled trial in outpatients with mild-to-moderate coronavirus disease 2019
Sudo, Pinto, Barros-Aragão, Bramati, Marins et al., Cognitive, behavioral, neuroimaging and inflammatory biomarkers after hospitalization for COVID-19 in Brazil, Brain Behav. Immun, doi:10.1016/j.bbi.2023.10.020
Sundar, Shah, Merchant, Asole, Acute ataxia and myoclonus in COVID-19: A case series, Ann. Indian Acad. Neurol, doi:10.4103/aian.AIAN_1296_20
Synowiec, Szczepa Ński, Barreto-Duran, Lie, Pyrc, Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): A systemic infection, Clin. Microbiol. Rev, doi:10.1128/CMR.00133-20
Słyk, Domitrz, Neurological manifestations of SARS-CoV-2-A systematic review, Neurol. I Neurochir. Pol, doi:10.5603/PJNNS.a2020.0050
Tang, Kido, Shi, Mccafferty, Ford et al., Blood markers show neural consequences of longCOVID-19, Cells, doi:10.3390/cells13060478
Teuwen, Geldhof, Pasut, Carmeliet, COVID-19: The vasculature unleashed, Nat. Rev. Immunol, doi:10.1038/s41577-020-0343-0
Tsai, Hsieh, Chao, Chen, Lin et al., Neuromuscular disorders in severe acute respiratory syndrome, Arch. Neurol, doi:10.1001/archneur.61.11.1669
Ttaquet, Sillett, Zhu, Mendel, Camplisson et al., Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: An analysis of 2-year retrospective cohort studies including 1,284,437 patients, Lancet Psychiatry, doi:10.1016/S2215-0366(22)00260-7
Varghese, John, Manesh, Karthik, Abraham, Clinical management of COVID-19, Indian J. Med. Res, doi:10.4103/ijmr.IJMR_957_20
Vashisht, Ahluwalia, Mondal, Singh, Sahajpal et al., Immune Factors Drive Expression of SARS-CoV-2 Receptor Genes Amid Sexual Disparity, Viruses, doi:10.3390/v15030657
Wang, Chen, Zhou, Lian, Zhang et al., SARS-CoV-2 invades host cells via a novel route: CD147-spike protein, bioRxiv, doi:10.1101/2020.03.14.988345
Wang, Mandigo, Yim, Meyers, Lavine, Stroke and mechanical thrombectomy in patients with COVID-19: Technical observations and patient characteristics, J. Neurointerventional Surg, doi:10.1136/neurintsurg-2020-016220
Wang, Xu, Gao, Lu, Han et al., Detection of SARS-CoV-2 in different types of clinical specimens, JAMA, doi:10.1001/jama.2020.3786
Wang, Xu, Musich, Lin, Mitochondrial dysfunction in neurodegenerative diseases and the potential countermeasure, CNS Neurosci. Ther, doi:10.1111/cns.13116
Williams, Martins, Shah, Hill, Coiras et al., Cytokine Deficiencies in Patients with Long-COVID, J. Clin. Cell. Immunol
Wu, Guo, Tang, Hong, Zhou et al., Prolonged presence of SARS-CoV-2 viral RNA in fecal samples, Lancet Gastroenterol. Hepatol, doi:10.1016/S2468-1253(20)30083-2
Yang, Zheng, Gou, Pu, Chen et al., Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.03.017
Zheng, Fan, Yu, Feng, Lou et al., Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: Retrospective cohort study, BMJ, doi:10.1136/bmj.m1443
Zieli Ńska-Turek, Turek, Lyson, Gajewski, Dorobek, Inflammatory proteins as strong predictors of death in COVID-19 patients with coexisting neurological diseases, medRxiv, doi:10.1101/2024.02.27.24303438
Zuckerkandl, Linus, Evolutionary divergence and convergence in proteins
DOI record:
{
"DOI": "10.3390/v16081183",
"ISSN": [
"1999-4915"
],
"URL": "http://dx.doi.org/10.3390/v16081183",
"abstract": "<jats:p>Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease (COVID-19), induced a global pandemic with a diverse array of clinical manifestations. While the acute phase of the pandemic may be waning, the intricacies of COVID-19′s impact on neurological health remain a crucial area of investigation. Early recognition of the spectrum of COVID-19 symptoms, ranging from mild fever and cough to life-threatening respiratory distress and multi-organ failure, underscored the significance of neurological complications, including anosmia, seizures, stroke, disorientation, encephalopathy, and paralysis. Notably, patients requiring intensive care unit (ICU) admission due to neurological challenges or due to them exhibiting neurological abnormalities in the ICU have shown increased mortality rates. COVID-19 can lead to a range of neurological complications such as anosmia, stroke, paralysis, cranial nerve deficits, encephalopathy, delirium, meningitis, seizures, etc., in affected patients. This review elucidates the burgeoning landscape of neurological sequelae associated with SARS-CoV-2 infection and explores the underlying neurobiological mechanisms driving these diverse manifestations. A meticulous examination of potential neuroinvasion routes by SARS-CoV-2 underscores the intricate interplay between the virus and the nervous system. Moreover, we dissect the diverse neurological manifestations emphasizing the necessity of a multifaceted approach to understanding the disease’s neurological footprint. In addition to elucidating the pathophysiological underpinnings, this review surveys current therapeutic modalities and delineates prospective avenues for neuro-COVID research. By integrating epidemiological, clinical, and diagnostic parameters, we endeavor to foster a comprehensive analysis of the nexus between COVID-19 and neurological health, thereby laying the groundwork for targeted therapeutic interventions and long-term management strategies.</jats:p>",
"alternative-id": [
"v16081183"
],
"author": [
{
"affiliation": [
{
"name": "Department of Pathology, Medical College of Georgia, Augusta University, Augusta, GA 30912, USA"
}
],
"family": "Vashisht",
"given": "Ashutosh",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Pathology, Medical College of Georgia, Augusta University, Augusta, GA 30912, USA"
}
],
"family": "Vashisht",
"given": "Vishakha",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pathology, Medical College of Georgia, Augusta University, Augusta, GA 30912, USA"
}
],
"family": "Singh",
"given": "Harmanpreet",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0060-6152",
"affiliation": [
{
"name": "Department of Pathology, Medical College of Georgia, Augusta University, Augusta, GA 30912, USA"
}
],
"authenticated-orcid": false,
"family": "Ahluwalia",
"given": "Pankaj",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3826-9489",
"affiliation": [
{
"name": "Department of Pathology, Medical College of Georgia, Augusta University, Augusta, GA 30912, USA"
}
],
"authenticated-orcid": false,
"family": "Mondal",
"given": "Ashis K.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Lincoln Memorial DeBusk College of Osteopathic Medicine, Lincoln Memorial University, Knoxville, TN 37902, USA"
}
],
"family": "Williams",
"given": "Colin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8072-7637",
"affiliation": [
{
"name": "Department of Pathology, Medical College of Georgia, Augusta University, Augusta, GA 30912, USA"
}
],
"authenticated-orcid": false,
"family": "Farmaha",
"given": "Jaspreet",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pathology, Medical College of Georgia, Augusta University, Augusta, GA 30912, USA"
}
],
"family": "Woodall",
"given": "Jana",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8283-2403",
"affiliation": [
{
"name": "Department of Pathology, Medical College of Georgia, Augusta University, Augusta, GA 30912, USA"
}
],
"authenticated-orcid": false,
"family": "Kolhe",
"given": "Ravindra",
"sequence": "additional"
}
],
"container-title": "Viruses",
"container-title-short": "Viruses",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
7,
24
]
],
"date-time": "2024-07-24T12:47:17Z",
"timestamp": 1721825237000
},
"deposited": {
"date-parts": [
[
2024,
7,
24
]
],
"date-time": "2024-07-24T13:06:20Z",
"timestamp": 1721826380000
},
"indexed": {
"date-parts": [
[
2024,
7,
25
]
],
"date-time": "2024-07-25T00:32:18Z",
"timestamp": 1721867538808
},
"is-referenced-by-count": 0,
"issue": "8",
"issued": {
"date-parts": [
[
2024,
7,
24
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2024,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
7,
24
]
],
"date-time": "2024-07-24T00:00:00Z",
"timestamp": 1721779200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1999-4915/16/8/1183/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1183",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
7,
24
]
]
},
"published-online": {
"date-parts": [
[
2024,
7,
24
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1128/CMR.00133-20",
"article-title": "Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): A systemic infection",
"author": "Synowiec",
"doi-asserted-by": "crossref",
"first-page": "e00133-20",
"journal-title": "Clin. Microbiol. Rev.",
"key": "ref_1",
"volume": "34",
"year": "2021"
},
{
"DOI": "10.1002/rmv.2270",
"article-title": "Present variants of concern and variants of interest of severe acute respiratory syndrome coronavirus 2: Their significant mutations in S-glycoprotein, infectivity, re-infectivity, immune escape and vaccines activity",
"author": "Chakraborty",
"doi-asserted-by": "crossref",
"first-page": "e2270",
"journal-title": "Rev. Med. Virol.",
"key": "ref_2",
"volume": "32",
"year": "2021"
},
{
"key": "ref_3",
"unstructured": "Scheepers, C., Everatt, J., Amoako, D.G., Mnguni, A., Ismail, A., Mahlangu, B., Wibmer, C.K., Wilkinson, E., Tegally, H., and San, J.E. (2021). The continuous evolution of SARS-CoV-2 in South Africa: A new lineage with rapid accumulation of mutations of concern and global detection. medRxiv."
},
{
"DOI": "10.1001/jamaneurol.2020.1127",
"article-title": "Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China",
"author": "Mao",
"doi-asserted-by": "crossref",
"first-page": "683",
"journal-title": "JAMA Neurol.",
"key": "ref_4",
"volume": "77",
"year": "2020"
},
{
"DOI": "10.1007/s11684-020-0786-5",
"article-title": "Neurological manifestations of patients with COVID-19: Potential routes of SARS-CoV-2 neuroinvasion from the periphery to the brain",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Front. Med.",
"key": "ref_5",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1091",
"article-title": "Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "m1091",
"journal-title": "BMJ",
"key": "ref_6",
"volume": "368",
"year": "2020"
},
{
"DOI": "10.1001/jamapsychiatry.2022.1616",
"article-title": "Bridging Knowledge Gaps in the Diagnosis and Management of Neuropsychiatric Sequelae of COVID-19",
"author": "Frontera",
"doi-asserted-by": "crossref",
"first-page": "811",
"journal-title": "JAMA Psychiatry",
"key": "ref_7",
"volume": "79",
"year": "2022"
},
{
"DOI": "10.1016/S2215-0366(20)30203-0",
"article-title": "Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic",
"author": "Rogers",
"doi-asserted-by": "crossref",
"first-page": "611",
"journal-title": "Lancet Psychiatry",
"key": "ref_8",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.5603/PJNNS.a2020.0050",
"article-title": "Neurological manifestations of SARS-CoV-2—A systematic review",
"author": "Domitrz",
"doi-asserted-by": "crossref",
"first-page": "378",
"journal-title": "Neurol. I Neurochir. Pol.",
"key": "ref_9",
"volume": "54",
"year": "2020"
},
{
"DOI": "10.1101/2020.05.11.088500",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "He, L., Mäe, M.A., Sun, Y., Muhl, L., Nahar, K., Liébanas, E.V., Fagerlund, M.J., Oldner, A., Liu, J., and Genové, G. (2020). Pericyte-specific vascular expression of SARS-CoV-2 receptor ACE2–implications for microvascular inflammation and hypercoagulopathy in COVID-19 patients. bioRxiv."
},
{
"DOI": "10.3389/fneur.2020.573095",
"doi-asserted-by": "crossref",
"key": "ref_11",
"unstructured": "Chen, R., Wang, K., Yu, J., Howard, D., French, L., Chen, Z., Wen, C., and Xu, Z. (2021). The spatial and cell-type distribution of SARS-CoV-2 receptor ACE2 in the human and mouse brains. Front. Neurol., 11."
},
{
"DOI": "10.1101/2020.03.14.988345",
"doi-asserted-by": "crossref",
"key": "ref_12",
"unstructured": "Wang, K., Chen, W., Zhou, Y.S., Lian, J.Q., Zhang, Z., Du, P., Gong, L., Zhang, Y., Cui, H.Y., and Geng, J.J. (2020). SARS-CoV-2 invades host cells via a novel route: CD147-spike protein. bioRxiv."
},
{
"DOI": "10.1101/2020.06.07.137802",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Cantuti-Castelvetri, L., Ojha, R., Pedro, L.D., Djannatian, M., Franz, J., Kuivanen, S., Kallio, K., Kaya, T., Anastasina, M., and Smura, T. (2020). Neuropilin-1 facilitates SARS-CoV-2 cell entry and provides a possible pathway into the central nervous system. bioRxiv."
},
{
"DOI": "10.1002/jmv.25915",
"article-title": "Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)",
"author": "Bryce",
"doi-asserted-by": "crossref",
"first-page": "699",
"journal-title": "J. Med. Virol.",
"key": "ref_14",
"volume": "92",
"year": "2020"
},
{
"article-title": "Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: Implications for pathogenesis and virus transmission pathways",
"author": "Ding",
"first-page": "622",
"journal-title": "J. Pathol. A J. Pathol. Soc. Great Br. Irel.",
"key": "ref_15",
"volume": "203",
"year": "2004"
},
{
"DOI": "10.1084/jem.20050828",
"article-title": "Multiple organ infection and the pathogenesis of SARS",
"author": "Gu",
"doi-asserted-by": "crossref",
"first-page": "415",
"journal-title": "J. Exp. Med.",
"key": "ref_16",
"volume": "202",
"year": "2005"
},
{
"DOI": "10.1111/jnc.13641",
"article-title": "Angiotensin II regulation of angiotensin-converting enzymes in spontaneously hypertensive rat primary astrocyte cultures",
"author": "Gowrisankar",
"doi-asserted-by": "crossref",
"first-page": "74",
"journal-title": "J. Neurochem.",
"key": "ref_17",
"volume": "138",
"year": "2016"
},
{
"article-title": "Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis",
"author": "Hamming",
"first-page": "631",
"journal-title": "J. Pathol. A J. Pathol. Soc. Great Br. Irel.",
"key": "ref_18",
"volume": "203",
"year": "2004"
},
{
"DOI": "10.1101/2020.05.30.125856",
"doi-asserted-by": "crossref",
"key": "ref_19",
"unstructured": "Mesci, P., Macia, A., Saleh, A., Martin-Sancho, L., Yin, X., Snethlage, C., Avansini, S., Chanda, S.K., and Muotri, A. (2020). Sofosbuvir protects human brain organoids against SARS-CoV-2. bioRxiv."
},
{
"DOI": "10.15252/embj.2020106230",
"article-title": "SARS-CoV-2 targets neurons of 3D human brain organoids",
"author": "Ramani",
"doi-asserted-by": "crossref",
"first-page": "e106230",
"journal-title": "EMBO J.",
"key": "ref_20",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1084/jem.20202135",
"article-title": "Neuroinvasive potential of SARS-CoV-2 revealed in a human brain",
"author": "Song",
"doi-asserted-by": "crossref",
"first-page": "e20202135",
"journal-title": "J. Exp. Med.",
"key": "ref_21",
"volume": "218",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.03.062",
"article-title": "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2",
"author": "Moriguchi",
"doi-asserted-by": "crossref",
"first-page": "55",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_22",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.8907",
"article-title": "Postmortem examination of patients with COVID-19",
"author": "Schaller",
"doi-asserted-by": "crossref",
"first-page": "2518",
"journal-title": "JAMA",
"key": "ref_23",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1007/978-1-4615-2996-5_53",
"doi-asserted-by": "crossref",
"key": "ref_24",
"unstructured": "Cabirac, G.F., Soike, K.F., Butunoi, C., Hoel, K., Johnson, S., Cai, G.Y., and Murray, R.S. (1994). Coronavirus JHM OMP1 pathogenesis in owl monkey CNS and coronavirus infection of owl monkey CNS via peripheral routes. Coronaviruses, Springer."
},
{
"article-title": "Detection of SARS-CoV-2 in different types of clinical specimens",
"author": "Wang",
"first-page": "1843",
"journal-title": "JAMA",
"key": "ref_25",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1443",
"article-title": "Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: Retrospective cohort study",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "m1443",
"journal-title": "BMJ",
"key": "ref_26",
"volume": "369",
"year": "2020"
},
{
"key": "ref_27",
"unstructured": "Bryce, C., Grimes, Z., Pujadas, E., Ahuja, S., Beasley, M.B., Albrecht, R., Hernandez, T., Stock, A., Zhao, Z., and Rasheed, M.A. (2020). Pathophysiology of SARS-CoV-2: Targeting of endothelial cells renders a complex disease with thrombotic microangiopathy and aberrant immune response. The Mount Sinai COVID-19 autopsy experience. medRxiv."
},
{
"DOI": "10.1124/pr.117.014647",
"article-title": "Neuroimmune axes of the blood–brain barriers and blood–brain interfaces: Bases for physiological regulation, disease states, and pharmacological interventions",
"author": "Erickson",
"doi-asserted-by": "crossref",
"first-page": "278",
"journal-title": "Pharmacol. Rev.",
"key": "ref_28",
"volume": "70",
"year": "2018"
},
{
"DOI": "10.1038/s41577-020-0343-0",
"article-title": "COVID-19: The vasculature unleashed",
"author": "Teuwen",
"doi-asserted-by": "crossref",
"first-page": "389",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref_29",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1111/bpa.12889",
"article-title": "Neuropathologic features of four autopsied COVID-19 patients",
"author": "Kantonen",
"doi-asserted-by": "crossref",
"first-page": "1012",
"journal-title": "Brain Pathol.",
"key": "ref_30",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1007/s00401-020-02166-2",
"article-title": "Neuropathology of COVID-19: A spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology",
"author": "Reichard",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Acta Neuropathol.",
"key": "ref_31",
"volume": "140",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2019373",
"article-title": "Neuropathological features of COVID-19",
"author": "Solomon",
"doi-asserted-by": "crossref",
"first-page": "989",
"journal-title": "N. Engl. J. Med.",
"key": "ref_32",
"volume": "383",
"year": "2020"
},
{
"article-title": "The circumventricular organs",
"author": "Kaur",
"first-page": "879",
"journal-title": "Histol. Histopathol.",
"key": "ref_33",
"volume": "32",
"year": "2017"
},
{
"DOI": "10.1101/2020.06.08.139329",
"doi-asserted-by": "crossref",
"key": "ref_34",
"unstructured": "Nampoothiri, S., Sauve, F., Ternier, G., Fernandois, D., Coelho, C., Imbernon, M., Deligia, E., Perbet, R., Florent, V., and Baroncini, M. (2020). The hypothalamus as a hub for putative SARS-CoV-2 brain infection. bioRxiv."
},
{
"DOI": "10.1038/nrmicro1343",
"article-title": "Coronavirus infection of the central nervous system: Host–virus stand-off",
"author": "Bergmann",
"doi-asserted-by": "crossref",
"first-page": "121",
"journal-title": "Nat. Rev. Microbiol.",
"key": "ref_35",
"volume": "4",
"year": "2006"
},
{
"DOI": "10.1038/ni.3666",
"article-title": "The movers and shapers in immune privilege of the CNS",
"author": "Engelhardt",
"doi-asserted-by": "crossref",
"first-page": "123",
"journal-title": "Nat. Immunol.",
"key": "ref_36",
"volume": "18",
"year": "2017"
},
{
"DOI": "10.1038/s41577-020-0331-4",
"article-title": "Pathological inflammation in patients with COVID-19: A key role for monocytes and macrophages",
"author": "Merad",
"doi-asserted-by": "crossref",
"first-page": "355",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref_37",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1101/2020.03.27.20045427",
"doi-asserted-by": "crossref",
"key": "ref_38",
"unstructured": "Feng, Z., Diao, B., Wang, R., Wang, G., Wang, C., Tan, Y., Liu, L., Wang, C., Liu, Y., and Liu, Y. (2020). The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) directly decimates human spleens and lymph nodes. medRxiv."
},
{
"DOI": "10.1016/j.cell.2020.05.006",
"article-title": "Host-viral infection maps reveal signatures of severe COVID-19 patients",
"author": "Bost",
"doi-asserted-by": "crossref",
"first-page": "1475",
"journal-title": "Cell",
"key": "ref_39",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1002/cne.23171",
"article-title": "Neurotropic virus tracing suggests a membranous-coating-mediated mechanism for transsynaptic communication",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "203",
"journal-title": "J. Comp. Neurol.",
"key": "ref_40",
"volume": "521",
"year": "2013"
},
{
"DOI": "10.1128/JVI.02545-13",
"article-title": "Effect of microtubule disruption on neuronal spread and replication of demyelinating and nondemyelinating strains of mouse hepatitis virus in vitro",
"author": "Biswas",
"doi-asserted-by": "crossref",
"first-page": "3043",
"journal-title": "J. Virol.",
"key": "ref_41",
"volume": "88",
"year": "2014"
},
{
"DOI": "10.1354/vp.41-2-101",
"article-title": "The vagus nerve is one route of transneural invasion for intranasally inoculated influenza a virus in mice",
"author": "Matsuda",
"doi-asserted-by": "crossref",
"first-page": "101",
"journal-title": "Vet. Pathol.",
"key": "ref_42",
"volume": "41",
"year": "2004"
},
{
"DOI": "10.3389/fncel.2020.00229",
"doi-asserted-by": "crossref",
"key": "ref_43",
"unstructured": "Fenrich, M., Mrdenovic, S., Balog, M., Tomic, S., Zjalic, M., Roncevic, A., Mandic, D., Debeljak, Z., and Heffer, M. (2020). SARS-CoV-2 dissemination through peripheral nerves explains multiple organ injury. Front. Cell. Neurosci., 14."
},
{
"DOI": "10.1089/vim.2018.0095",
"article-title": "Case report of transmissible gastroenteritis coronavirus infection associated with small intestine and brain lesions in piglets",
"author": "Papatsiros",
"doi-asserted-by": "crossref",
"first-page": "63",
"journal-title": "Viral Immunol.",
"key": "ref_44",
"volume": "32",
"year": "2019"
},
{
"DOI": "10.1016/j.mayocp.2020.03.026",
"article-title": "Angiotensin-converting enzyme 2 and antihypertensives (angiotensin receptor blockers and angiotensin-converting enzyme inhibitors) in coronavirus disease 2019",
"author": "Lavie",
"doi-asserted-by": "crossref",
"first-page": "1222",
"journal-title": "Mayo Clin. Proc.",
"key": "ref_45",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1016/B978-1-4832-2734-4.50017-6",
"doi-asserted-by": "crossref",
"key": "ref_46",
"unstructured": "Zuckerkandl, E., and Linus, P. (1965). Evolutionary divergence and convergence in proteins. Evolving Genes and Proteins, Academic Press."
},
{
"DOI": "10.1002/iub.2379",
"article-title": "SARS-CoV-2 multifaceted interaction with the human host. Part II: Innate immunity response, immunopathology, and epigenetics",
"author": "Beacon",
"doi-asserted-by": "crossref",
"first-page": "2331",
"journal-title": "IUBMB Life",
"key": "ref_47",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.4103/aian.AIAN_1296_20",
"article-title": "Acute ataxia and myoclonus in COVID-19: A case series",
"author": "Sundar",
"doi-asserted-by": "crossref",
"first-page": "807",
"journal-title": "Ann. Indian Acad. Neurol.",
"key": "ref_48",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1056/NEJMc2008597",
"article-title": "Neurologic features in severe SARS-CoV-2 infection",
"author": "Helms",
"doi-asserted-by": "crossref",
"first-page": "2268",
"journal-title": "N. Engl. J. Med.",
"key": "ref_49",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1002/acn3.51210",
"article-title": "Frequent neurologic manifestations and encephalopathy-associated morbidity in COVID-19 patients",
"author": "Liotta",
"doi-asserted-by": "crossref",
"first-page": "2221",
"journal-title": "Ann. Clin. Transl. Neurol.",
"key": "ref_50",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/S2468-1253(20)30083-2",
"article-title": "Prolonged presence of SARS-CoV-2 viral RNA in fecal samples",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "434",
"journal-title": "Lancet Gastroenterol. Hepatol.",
"key": "ref_51",
"volume": "5",
"year": "2020"
},
{
"key": "ref_52",
"unstructured": "Aleem, A., Akbar Samad, A.B., and Vaqar, S. (2023). Emerging Variants of SARS-CoV-2 and Novel Therapeutics against Coronavirus (COVID-19). StatPearls, StatPearls Publishing."
},
{
"DOI": "10.1212/WNL.0000000000207534",
"article-title": "Incidence and long-term functional outcome of neurologic disorders in hospitalized patients with COVID-19 infected with pre-omicron variants",
"author": "Beretta",
"doi-asserted-by": "crossref",
"first-page": "e892",
"journal-title": "Neurology",
"key": "ref_53",
"volume": "101",
"year": "2023"
},
{
"DOI": "10.1038/s41467-023-40228-7",
"article-title": "Neuroinvasion and anosmia are independent phenomena upon infection with SARS-CoV-2 and its variants",
"author": "Perraud",
"doi-asserted-by": "crossref",
"first-page": "4485",
"journal-title": "Nat. Commun.",
"key": "ref_54",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1016/S2215-0366(22)00260-7",
"article-title": "Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: An analysis of 2-year retrospective cohort studies including 1,284,437 patients",
"author": "TTaquet",
"doi-asserted-by": "crossref",
"first-page": "815",
"journal-title": "Lancet Psychiatry",
"key": "ref_55",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1186/s12974-023-02861-3",
"article-title": "Differential effects of SARS-CoV-2 variants on central nervous system cells and blood–brain barrier functions",
"author": "Proust",
"doi-asserted-by": "crossref",
"first-page": "184",
"journal-title": "J. Neuroinflamm.",
"key": "ref_56",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.1016/S0140-6736(22)00462-7",
"article-title": "Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B. 1.1. 529) and delta (B. 1.617. 2) variants in England: A cohort study",
"author": "Nyberg",
"doi-asserted-by": "crossref",
"first-page": "1303",
"journal-title": "Lancet",
"key": "ref_57",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.1093/brain/awaa240",
"article-title": "The emerging spectrum of COVID-19 neurology: Clinical, radiological and laboratory findings",
"author": "Paterson",
"doi-asserted-by": "crossref",
"first-page": "3104",
"journal-title": "Brain",
"key": "ref_58",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.1007/s00405-020-05965-1",
"article-title": "Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study",
"author": "Lechien",
"doi-asserted-by": "crossref",
"first-page": "2251",
"journal-title": "Eur. Arch. Oto-Rhino Laryngol.",
"key": "ref_59",
"volume": "277",
"year": "2020"
},
{
"DOI": "10.1515/dx-2020-0046",
"article-title": "Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): Early report from the United States",
"author": "Aggarwal",
"doi-asserted-by": "crossref",
"first-page": "91",
"journal-title": "Diagnosis",
"key": "ref_60",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1111/irv.13235",
"article-title": "Sex differences in COVID-19 symptom severity and trajectories among ambulatory adults",
"author": "Massion",
"doi-asserted-by": "crossref",
"first-page": "e13235",
"journal-title": "Influenza Other Respir. Viruses",
"key": "ref_61",
"volume": "17",
"year": "2023"
},
{
"DOI": "10.3390/v15030657",
"doi-asserted-by": "crossref",
"key": "ref_62",
"unstructured": "Vashisht, A., Ahluwalia, P., Mondal, A.K., Singh, H., Sahajpal, N.S., Fulzele, S., Kota, V., Gahlay, G.K., and Kolhe, R. (2023). Immune Factors Drive Expression of SARS-CoV-2 Receptor Genes Amid Sexual Disparity. Viruses, 15."
},
{
"DOI": "10.1001/jama.2020.6771",
"article-title": "Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection",
"author": "Spinato",
"doi-asserted-by": "crossref",
"first-page": "2089",
"journal-title": "JAMA",
"key": "ref_63",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1111/ene.14273",
"article-title": "Acute-onset smell and taste disorders in the context of COVID-19: A pilot multicentre polymerase chain reaction based case–control study",
"author": "Monreal",
"doi-asserted-by": "crossref",
"first-page": "1738",
"journal-title": "Eur. J. Neurol.",
"key": "ref_64",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1002/alr.22587",
"article-title": "Smell dysfunction: A biomarker for COVID-19",
"author": "Moein",
"doi-asserted-by": "crossref",
"first-page": "944",
"journal-title": "Int. Forum Allergy Rhinol.",
"key": "ref_65",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2009787",
"article-title": "Large-vessel stroke as a presenting feature of COVID-19 in the young",
"author": "Oxley",
"doi-asserted-by": "crossref",
"first-page": "e60",
"journal-title": "N. Engl. J. Med.",
"key": "ref_66",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.4103/ijmr.IJMR_957_20",
"article-title": "Clinical management of COVID-19",
"author": "Varghese",
"doi-asserted-by": "crossref",
"first-page": "401",
"journal-title": "Indian J. Med. Res.",
"key": "ref_67",
"volume": "151",
"year": "2020"
},
{
"DOI": "10.1007/s10072-020-04801-y",
"article-title": "Neurological manifestations of COVID-19: A systematic review and meta-analysis of proportions",
"author": "Favas",
"doi-asserted-by": "crossref",
"first-page": "3437",
"journal-title": "Neurol. Sci.",
"key": "ref_68",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1136/svn-2020-000431",
"article-title": "Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "279",
"journal-title": "Stroke Vasc. Neurol.",
"key": "ref_69",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1038/s41586-021-03207-w",
"article-title": "Evolution of antibody immunity to SARS-CoV-2",
"author": "Gaebler",
"doi-asserted-by": "crossref",
"first-page": "639",
"journal-title": "Nature",
"key": "ref_70",
"volume": "591",
"year": "2021"
},
{
"DOI": "10.3988/jcn.2017.13.3.227",
"article-title": "Neurological complications during treatment of Middle East respiratory syndrome",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "227",
"journal-title": "J. Clin. Neurol.",
"key": "ref_71",
"volume": "13",
"year": "2017"
},
{
"DOI": "10.1001/archneur.61.11.1669",
"article-title": "Neuromuscular disorders in severe acute respiratory syndrome",
"author": "Tsai",
"doi-asserted-by": "crossref",
"first-page": "1669",
"journal-title": "Arch. Neurol.",
"key": "ref_72",
"volume": "61",
"year": "2004"
},
{
"DOI": "10.1016/j.virol.2006.01.049",
"article-title": "Human coronavirus OC43 infection induces chronic encephalitis leading to disabilities in BALB/C mice",
"author": "Jacomy",
"doi-asserted-by": "crossref",
"first-page": "335",
"journal-title": "Virology",
"key": "ref_73",
"volume": "349",
"year": "2006"
},
{
"DOI": "10.1186/s12985-017-0719-3",
"article-title": "Multiple sclerosis: An example of pathogenic viral interaction?",
"author": "Fierz",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Virol. J.",
"key": "ref_74",
"volume": "14",
"year": "2017"
},
{
"DOI": "10.1146/annurev-pathol-020117-043952",
"article-title": "Type I interferons in autoimmune disease",
"author": "Crow",
"doi-asserted-by": "crossref",
"first-page": "369",
"journal-title": "Annu. Rev. Pathol. Mech. Dis.",
"key": "ref_75",
"volume": "14",
"year": "2019"
},
{
"DOI": "10.1128/JVI.74.19.8913-8921.2000",
"article-title": "Neuroinvasion by human respiratory coronaviruses",
"author": "Arbour",
"doi-asserted-by": "crossref",
"first-page": "8913",
"journal-title": "J. Virol.",
"key": "ref_76",
"volume": "74",
"year": "2000"
},
{
"DOI": "10.1016/j.clim.2007.02.002",
"article-title": "Long-term human coronavirus-myelin cross-reactive T-cell clones derived from multiple sclerosis patients",
"author": "Boucher",
"doi-asserted-by": "crossref",
"first-page": "258",
"journal-title": "Clin. Immunol.",
"key": "ref_77",
"volume": "123",
"year": "2007"
},
{
"DOI": "10.1016/j.neuron.2019.05.035",
"article-title": "Transneuronal propagation of pathologic α-synuclein from the gut to the brain models Parkinson’s disease",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "627",
"journal-title": "Neuron",
"key": "ref_78",
"volume": "103",
"year": "2019"
},
{
"DOI": "10.3390/ijms20092115",
"doi-asserted-by": "crossref",
"key": "ref_79",
"unstructured": "Srikantha, P., and Mohajeri, M.H. (2019). The possible role of the microbiota-gut-brain-axis in autism spectrum disorder. Int. J. Mol. Sci., 20."
},
{
"DOI": "10.1038/s43587-022-00321-w",
"article-title": "Severe COVID-19 induces molecular signatures of aging in the human brain",
"author": "Mavrikaki",
"doi-asserted-by": "crossref",
"first-page": "1130",
"journal-title": "Nat. Aging",
"key": "ref_80",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.1038/s41380-022-01786-2",
"article-title": "SARS-CoV-2 promotes microglial synapse elimination in human brain organoids",
"author": "Samudyata",
"doi-asserted-by": "crossref",
"first-page": "3939",
"journal-title": "Mol. Psychiatry",
"key": "ref_81",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1111/cns.13116",
"article-title": "Mitochondrial dysfunction in neurodegenerative diseases and the potential countermeasure",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "816",
"journal-title": "CNS Neurosci. Ther.",
"key": "ref_82",
"volume": "25",
"year": "2019"
},
{
"DOI": "10.3389/fnagi.2020.614650",
"doi-asserted-by": "crossref",
"key": "ref_83",
"unstructured": "Ganji, R., and Reddy, P.H. (2021). Impact of COVID-19 on mitochondrial-based immunity in aging and age-related diseases. Front. Aging Neurosci., 12."
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"article-title": "Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "91",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_84",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2020-046980",
"article-title": "Association of frailty status with adverse clinical outcomes in patients with COVID-19: Protocol for a systematic review and dose–response meta-analysis",
"author": "Pei",
"doi-asserted-by": "crossref",
"first-page": "e046980",
"journal-title": "BMJ Open",
"key": "ref_85",
"volume": "11",
"year": "2021"
},
{
"article-title": "Cytokine Deficiencies in Patients with Long-COVID",
"author": "Williams",
"first-page": "672",
"journal-title": "J. Clin. Cell. Immunol.",
"key": "ref_86",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.bbi.2020.12.022",
"article-title": "High frequency of cerebrospinal fluid autoantibodies in COVID-19 patients with neurological symptoms",
"author": "Franke",
"doi-asserted-by": "crossref",
"first-page": "415",
"journal-title": "Brain Behav. Immun.",
"key": "ref_87",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1101/2021.01.10.20249014",
"doi-asserted-by": "crossref",
"key": "ref_88",
"unstructured": "GGarcia, M.A., Barreras, P.V., Lewis, A., Pinilla, G., Sokoll, L.J., Kickler, T., Mostafa, H., Caturegli, M., Moghekar, A., and Fitzgerald, K.C. (2021). Cerebrospinal fluid in COVID-19 neurological complications: No cytokine storm or neuroinflammation. medRxiv."
},
{
"DOI": "10.1016/j.bbih.2024.100805",
"article-title": "Changes in neuroinflammatory biomarkers correlate with disease severity and neuroimaging alterations in patients with COVID-19 neurological complications",
"author": "Pinto",
"doi-asserted-by": "crossref",
"first-page": "100805",
"journal-title": "Brain Behav. Immun. Health",
"key": "ref_89",
"volume": "39",
"year": "2024"
},
{
"DOI": "10.1161/STROKEAHA.120.030995",
"article-title": "Acute cerebrovascular events in hospitalized COVID-19 patients",
"author": "Rothstein",
"doi-asserted-by": "crossref",
"first-page": "e219",
"journal-title": "Stroke",
"key": "ref_90",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.20944/preprints202402.0892.v1",
"doi-asserted-by": "crossref",
"key": "ref_91",
"unstructured": "Tang, N., Kido, T., Shi, J., McCafferty, E., Ford, J.M., Dal Bon, K., and Pulliam, L. (2024). Blood markers show neural consequences of longCOVID-19. Cells, 13."
},
{
"DOI": "10.1101/2024.02.27.24303438",
"doi-asserted-by": "crossref",
"key": "ref_92",
"unstructured": "Zielińska-Turek, J., Turek, G., Lyson, T., Gajewski, J., Ząbek, M., and Dorobek, M. (2024). Inflammatory proteins as strong predictors of death in COVID-19 patients with coexisting neurological diseases. medRxiv."
},
{
"DOI": "10.1016/j.bbi.2023.10.020",
"article-title": "Cognitive, behavioral, neuroimaging and inflammatory biomarkers after hospitalization for COVID-19 in Brazil",
"author": "Sudo",
"doi-asserted-by": "crossref",
"first-page": "434",
"journal-title": "Brain Behav. Immun.",
"key": "ref_93",
"volume": "115",
"year": "2024"
},
{
"DOI": "10.1136/neurintsurg-2020-016220",
"article-title": "Stroke and mechanical thrombectomy in patients with COVID-19: Technical observations and patient characteristics",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "648",
"journal-title": "J. Neurointerventional Surg.",
"key": "ref_94",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1161/STROKEAHA.120.030574",
"article-title": "Treatment of acute ischemic stroke due to large vessel occlusion with COVID-19: Experience from Paris",
"author": "Escalard",
"doi-asserted-by": "crossref",
"first-page": "2540",
"journal-title": "Stroke",
"key": "ref_95",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.1111/ene.14913",
"article-title": "Encephalitis as neurological complication of COVID-19: A systematic review and meta-analysis of incidence, outcomes, and predictors",
"author": "Siow",
"doi-asserted-by": "crossref",
"first-page": "3491",
"journal-title": "Eur. J. Neurol.",
"key": "ref_96",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1017/cjn.2021.102",
"article-title": "Guillain Barre syndrome as a complication of COVID-19: A systematic review",
"author": "Aladawi",
"doi-asserted-by": "crossref",
"first-page": "38",
"journal-title": "Can. J. Neurol. Sci.",
"key": "ref_97",
"volume": "49",
"year": "2022"
},
{
"DOI": "10.1002/glia.22880",
"article-title": "Interleukin-10 is a critical regulator of white matter lesion containment following viral induced demyelination",
"author": "Puntambekar",
"doi-asserted-by": "crossref",
"first-page": "2106",
"journal-title": "Glia",
"key": "ref_98",
"volume": "63",
"year": "2015"
},
{
"DOI": "10.1016/j.bbi.2010.01.005",
"article-title": "Oncostatin M is a novel glucocorticoid-dependent neuroinflammatory factor that enhances oligodendrocyte precursor cell activity in demyelinated sites",
"author": "Glezer",
"doi-asserted-by": "crossref",
"first-page": "695",
"journal-title": "Brain Behav. Immun.",
"key": "ref_99",
"volume": "24",
"year": "2010"
},
{
"DOI": "10.1016/j.bbi.2019.07.027",
"article-title": "Inhibition of CD147 improves oligodendrogenesis and promotes white matter integrity and functional recovery in mice after ischemic stroke",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "13",
"journal-title": "Brain Behav. Immun.",
"key": "ref_100",
"volume": "82",
"year": "2019"
},
{
"DOI": "10.2165/00002018-200932040-00005",
"article-title": "Vaccines and guillain-barre syndrome",
"author": "Haber",
"doi-asserted-by": "crossref",
"first-page": "309",
"journal-title": "Drug Saf.",
"key": "ref_101",
"volume": "32",
"year": "2009"
},
{
"DOI": "10.1001/jama.2021.24939",
"article-title": "Effect of subcutaneous casirivimab and imdevimab antibody combination vs placebo on development of symptomatic COVID-19 in early asymptomatic SARS-CoV-2 infection: A randomized clinical trial",
"author": "Sarkar",
"doi-asserted-by": "crossref",
"first-page": "432",
"journal-title": "JAMA",
"key": "ref_102",
"volume": "327",
"year": "2022"
},
{
"DOI": "10.1093/ofid/ofac053",
"article-title": "Efficacy and safety of regdanvimab (CT-P59): A phase 2/3 randomized, double-blind, placebo-controlled trial in outpatients with mild-to-moderate coronavirus disease 2019",
"author": "Preotescu",
"doi-asserted-by": "crossref",
"first-page": "ofac053",
"journal-title": "Open Forum Infectious Diseases",
"key": "ref_103",
"volume": "Volume 9",
"year": "2022"
},
{
"DOI": "10.3390/biology11071084",
"doi-asserted-by": "crossref",
"key": "ref_104",
"unstructured": "Cuenca-Zaldivar, J.N., Monroy Acevedo, Á., Fernández-Carnero, J., Sánchez-Romero, E.A., Villafañe, J.H., and Barragán Carballar, C. (2022). Effects of a Multicomponent Exercise Program on Improving Frailty in Post-COVID-19 Older Adults after Intensive Care Units: A Single-Group Retrospective Cohort Study. Biology, 11."
}
],
"reference-count": 104,
"references-count": 104,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1999-4915/16/8/1183"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Neurological Complications of COVID-19: Unraveling the Pathophysiological Underpinnings and Therapeutic Implications",
"type": "journal-article",
"volume": "16"
}