COVID-19 in patients with hepatobiliary and pancreatic diseases in East London: a single-centre cohort study
et al., Pancreatology, doi:10.1016/j.pan.2020.10.005, Mar 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 15,440 patients with hepatobiliary and pancreatic diseases in the United Kingdom, 226 with confirmed COVID-19, showing higher risk with vitamin D supplementation. Results are likely confounded by impaired vitamin D processing and propensity to prescribe supplementation based on specifics of each patient's disease and vitamin D levels. Adjustments used broad age ranges, likely adding to residual confounding.
This is the 24th of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
This study is excluded in the after exclusion results of meta-analysis:
significant unadjusted confounding possible.
|
risk of death, 42.1% higher, RR 1.42, p = 0.34, treatment 21 of 64 (32.8%), control 26 of 135 (19.3%), adjusted per study, odds ratio converted to relative risk.
|
|
risk of case, 146.0% higher, RR 2.46, p < 0.001, treatment 69 of 2,168 (3.2%), control 139 of 12,681 (1.1%), adjusted per study, odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ullah et al., 4 Mar 2021, retrospective, United Kingdom, peer-reviewed, 3 authors, dosage not specified.
COVID-19 in patients with hepatobiliary and pancreatic diseases: A single-centre cross-sectional study in East London
doi:10.1101/2020.09.07.20189621
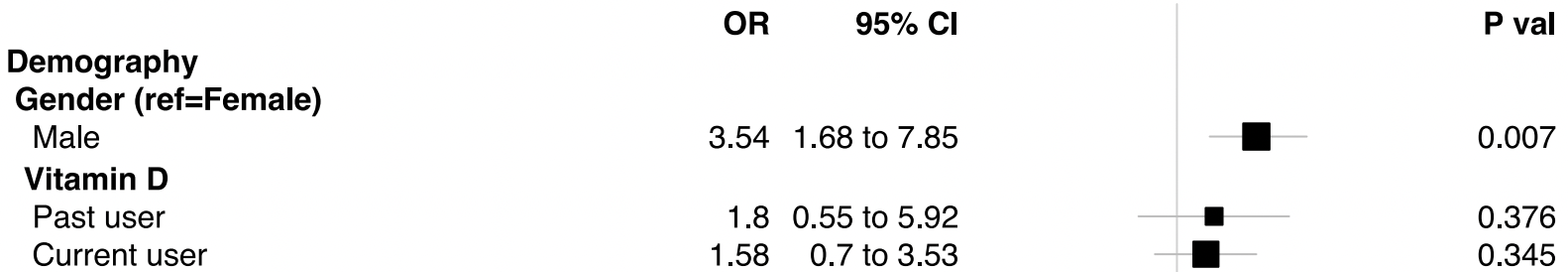
Objective To explore risk factors associated with COVID-19 susceptibility and survival in patients with pre-existing hepato-pancreato-biliary (HPB) conditions. Design Cross-sectional study. Setting East London Pancreatic Cancer Epidemiology (EL-PaC-Epidem) study at Barts Health NHS Trust, UK. Linked electronic health records were interrogated on a cohort of participants (age ≥ 18 years), reported with HPB conditions between 1 April 2008 and 6 March 2020. Participants EL-PaC-Epidem study participants, alive on 12 February 2020, and living in East London within the previous six months (n=15 440). The cohort represents a multi-ethnic population with 51.7% belonging to the non-White background. Main outcome measure COVID-19 incidence and mortality. Results Some 226 (1.5%) participants had confirmed COVID-19 diagnosis between 12 February and 12 June 2020, with an increased odds for men (OR 1.56; 95% CI 1.2 to 2.04) and Black ethnicity (2.04; 1.39 to 2.95) as well as patients with moderate to severe liver disease (2.2; 1.35 to 3.59). Each additional comorbidity increased the odds of infection by 62%. Substance mis-users were at more risk of infection, so were patients on Vitamin D treatment. The higher odds ratios in patients with chronic pancreatic or mild liver conditions, age>70, and history of smoking or obesity were due to co-existing comorbidities. Increased odds of death were observed for men (3.54; 1.68 to 7.85) and Black ethnicity (3.77; 1.38 to 10.7). Patients having respiratory complications from COVID-19 without a history of chronic respiratory disease also had higher odds of death (5.77; 1.75 to 19).
Conclusions In this large population-based study of HPB patients, men, Black ethnicity, pre-existing moderate to severe liver conditions, six common medical multimorbidities, substance mis-use, and a history of Vitamin D treatment independently posed higher odds of acquiring COVID-19 compared to their respective counterparts. The odds of death were significantly high for men and Black people.
FOOTNOTES Contributors: ADU designed the study, and was responsible for undertaking and completing data collection, processing and analysis. HMK and CC oversaw the conduct and management of the study. All the authors contributed to the selection of study variables and interpretation post analysis. ADU wrote the first drafts of the report and all the authors made critical revisions. Data sharing: All statistical data relevant to the study are included in the article or uploaded as supplementary information. Only the corresponding author had full access to all the participants' data in the study. The authors confirm that researchers seeking the completely anonymised final analysis dataset for this work can submit a data request to the corresponding author. Transparency statement: The corresponding author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
Almario, Chey, Spiegel, Increased risk of COVID-19 among users of proton-pump inhibitors, Am J Gastroenterol
Blanco, Ambrosioni, Garcia, COVID-19 in patients with HIV: clinical case series, Lancet HIV
Brenner, Ungaro, Gearry, Corticosteroids, but not TNF Antagonists, are Associated with Adverse COVID-19 Outcomes in Patients With Inflammatory Bowel Diseases: Results from an International Registry, Gastroenterology
Ciulla, Switching to another antihypertensive effective drug when using ACEIs/ARBs to treat arterial hypertension during COVID-19, Eur Heart J
Dai, Liu, Liu, Patients with Cancer Appear More Vulnerable to SARS-CoV-2: A Multicenter Study during the COVID-19 Outbreak, Cancer Discov
Deng, Yin, Chen, Zeng, Clinical determinants for fatality of 44,672 patients with COVID-19, Crit Care
Docherty, Harrison, Green, Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study, BMJ
Dubey, Ghosh, Chatterjee, Biswas, Chattergee et al., COVID-19 and addiction, Diabetes Metab Syndr
Fang, Karakiulakis, Roth, Gurwitz, Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?, Lancet Respir Med
Gibson, Evans, An, Jones, ACE 2 Coding Variants: A Potential X-linked Risk Factor for COVID-19 Disease, doi:10.1101/2020.04
Glasheen, Cordier, Gumpina, Charlson Comorbidity Index: ICD-9 Update and ICD-10 Translation, Am Health Drug Benefits
Gou, Fu, Yue, Gut microbiota may underlie the predisposition of healthy individuals to COVID-19, Preprint at medRxiv, doi:10.1101/2020.04.22.20076091
Guan, Liang, Zhao, Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis, Eur Respir J
Gubatan, Levitte, Patel, Prevalence, risk factors and clinical outcomes of COVID-19 in patients with a history of pancreatitis in Northern California, Gut
Hadi, Werge, Kristiansen, Coronavirus Disease-19
Halpin, Faner, Sibila, Do chronic respiratory diseases or their treatment affect the risk of SARS-CoV-2 infection?, Lancet Respir Med
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Jain, Chaurasia, Sengar, Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci Rep
Katabathina, Flaherty, Dasyam, Biliary Diseases with Pancreatic Counterparts": Cross-sectional Imaging Findings, Radiographics
Khawaja, Warwick, Hysi, Associations with COVID-19 hospitalisation amongst 406,793 adults: the UK Biobank prospective cohort study, Preprint, doi:10.1101/2020.05.06.2009295747
Kovesdy, Furth, Zoccali, Obesity and Kidney Disease, Can J Kidney Health Dis
Leber, Mayrhauser, Rybczynski, Innate immune dysfunction in acute and chronic liver disease, Wien Klin Wochenschr
Lee, Yeniova, Moon, Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching, Gut
Lighter, Phillips, Hochman, Obesity in Patients Younger Than 60
Mantovani, Beatrice, Dalbeni, Coronavirus disease 2019 and prevalence of chronic liver disease: A meta-analysis, Liver Int
Mcnabb-Baltar, Grover, Lipase elevation in patients with COVID-19, Am J Gastroenterol
Mcneely, Kumar, Rieckmann, Barriers and facilitators affecting the implementation of substance use screening in primary care clinics: a qualitative study of patients, providers, and staff, Addict Sci Clin Pract
Miyara, Low incidence of daily active tobacco smoking in patients with symptomatic COVID-19, Qeios, doi:10.32388/WPP19W.3
O'mara, Could ACE inhibitors and particularly ARBs increase susceptibility to COVID-19 infection?, BMJ
Ornell, Moura, Scherer, The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment, Psychiatry Res
Perez-Guzman, Daunt, Mukherjee, Clinical characteristics and predictors of outcomes of hospitalized patients with COVID-19 in a multi-ethnic London NHS Trust: a retrospective cohort study, Clin Infect Dis, doi:10.1093/cid/ciaa1091
Piroth, Cottenet, Mariet, Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study, Lancet Respir Med, doi:10.1016/s2213-2600(20)30527-0
Platt, Warwick, Are some ethnic groups more vulnerable to COVID-19 than others? Institute for Fiscal Studies
Rentsch, Kidwai-Khan, Tate, Covid-19 testing, hospital admission, and intensive care among 2,026,227 United States veterans aged 54-75 years, doi:10.1101/2020.04.09.20059964
Schultze, Walker, Mackenna, Risk of COVID-19-related death among patients with chronic obstructive pulmonary disease or asthma prescribed inhaled corticosteroids: an observational cohort study using the OpenSAFELY platform, Lancet Respir Med
Tanne, Covid 19: Patients have many more complications than flu patients, finds US study, BMJ
Thaweerat, Current evidence on pancreatic involvement in SARS-CoV-2 infection, Pancrteatology
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature
Yeoh, Zuo, Lui, Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19, Gut
Zhang, Kang, Gong, Digestive system is a potential route of COVID-19: an analysis of single-cell coexpression pattern of key proteins in viral entry process, Gut
DOI record:
{
"DOI": "10.1016/j.pan.2020.10.005",
"ISSN": [
"1424-3903"
],
"URL": "http://dx.doi.org/10.1016/j.pan.2020.10.005",
"alternative-id": [
"S1424390320307298"
],
"author": [
{
"affiliation": [],
"family": "Ullah",
"given": "Abu Dayem",
"sequence": "first"
},
{
"affiliation": [],
"family": "Kocher",
"given": "Hemant",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chelala",
"given": "Claude",
"sequence": "additional"
}
],
"container-title": [
"Pancreatology"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
11,
24
]
],
"date-time": "2020-11-24T00:00:17Z",
"timestamp": 1606176017000
},
"deposited": {
"date-parts": [
[
2020,
11,
24
]
],
"date-time": "2020-11-24T08:56:53Z",
"timestamp": 1606208213000
},
"indexed": {
"date-parts": [
[
2021,
12,
21
]
],
"date-time": "2021-12-21T08:36:43Z",
"timestamp": 1640075803344
},
"is-referenced-by-count": 1,
"issn-type": [
{
"type": "print",
"value": "1424-3903"
}
],
"issue": "8",
"issued": {
"date-parts": [
[
2020,
12
]
]
},
"journal-issue": {
"issue": "8",
"published-print": {
"date-parts": [
[
2020,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
12,
1
]
],
"date-time": "2020-12-01T00:00:00Z",
"timestamp": 1606780800000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1424390320307298?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1424390320307298?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "e15",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2020,
12
]
]
},
"published-print": {
"date-parts": [
[
2020,
12
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"score": 1,
"short-container-title": [
"Pancreatology"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Gastroenterology",
"Hepatology",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": [
"COVID-19 in patients with hepatobiliary and pancreatic diseases in East London: a single-centre cohort study"
],
"type": "journal-article",
"volume": "20"
}
