The effect of vitamin D deficiency on platelet parameters in patients with COVID-19
et al., Frontiers in Cellular and Infection Microbiology, doi:10.3389/fcimb.2024.1360075, Mar 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
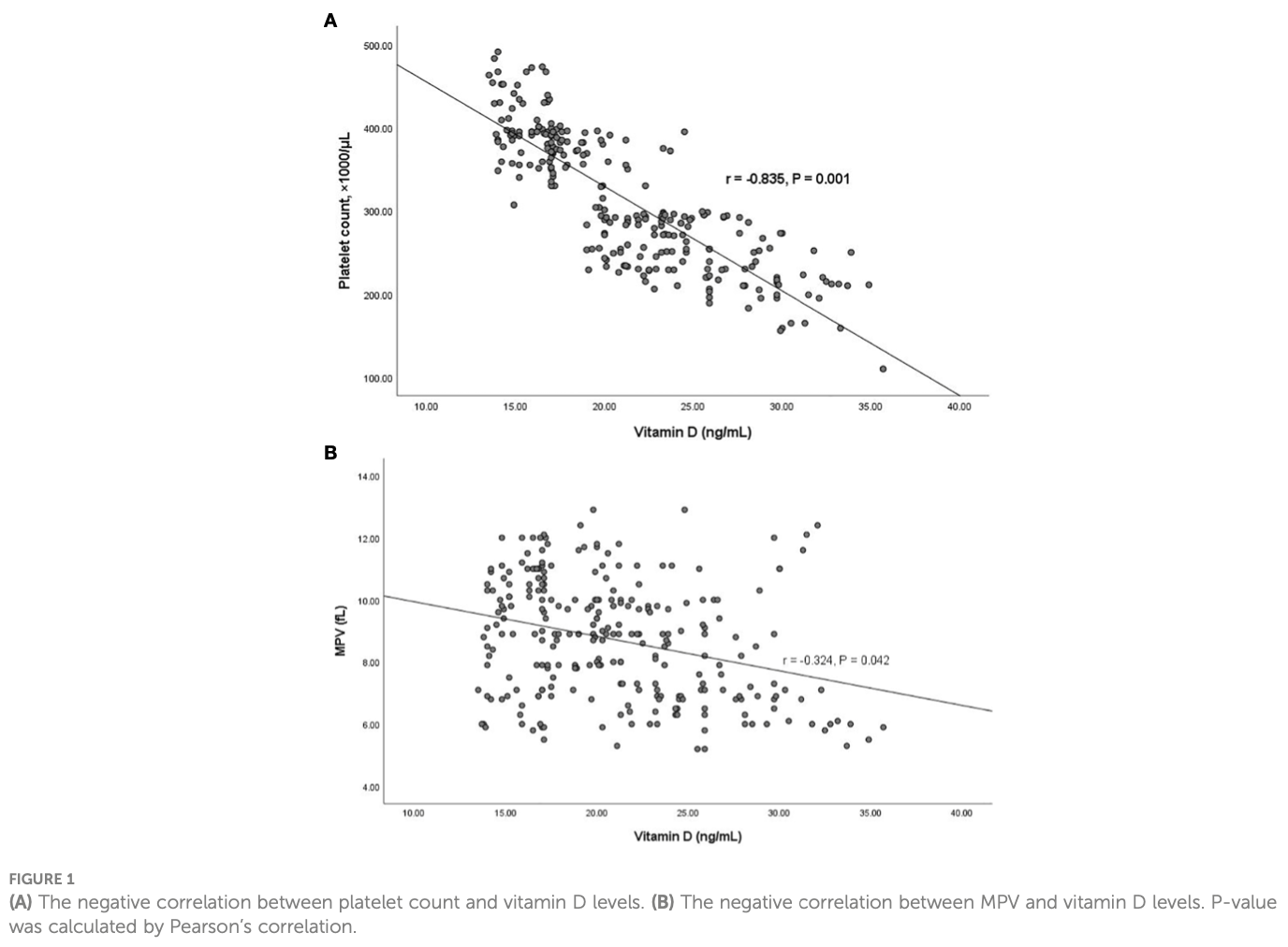
Retrospective study of 707 COVID-19 patients showing higher platelet count and mean platelet volume (MPV) in patients with vitamin D deficiency compared to those without deficiency and healthy controls. There was a significant negative correlation between platelet count and MPV with vitamin D levels in the deficient patients. Authors conclude that maintaining adequate vitamin D levels in COVID-19 patients is important and may reduce susceptibility to diseases like coronary artery disease.
Talebzadeh et al., 8 Mar 2024, retrospective, Iran, peer-reviewed, 7 authors.
Contact: a.qasemi2012@yahoo.com.
The effect of vitamin D deficiency on platelet parameters in patients with COVID-19
Frontiers in Cellular and Infection Microbiology, doi:10.3389/fcimb.2024.1360075
Introduction: Since there is very little information about the relationship between platelet parameters and vitamin D concentration in patients with COVID-19, the aim of this study is to investigate the relationship between serum vitamin D level and platelet parameters in patients with COVID-19 and to compare these parameters in patients with COVID-19 without vitamin D deficiency and, subsequently, the prognostic value of these parameters in cases of vitamin D deficiency. Methods: Seven hundred and forty-three patients diagnosed with COVID-19 were enrolled in this study. Patients were divided into two groups: those with and without vitamin D deficiency. The associations between platelet indices and vitamin D levels were analyzed by Pearson's correlation analysis and a one-way ANOVA test. Results: Platelet count and mean platelet volume (MPV) were significantly higher in the patients with vitamin D deficiency than in the patients without vitamin D deficiency. There was a significant negative correlation between platelet count and MPV with vitamin D levels in patients with vitamin D deficiency (r = -0.835, P = 0.001 & r = -0.324, P = 0.042, respectively). Vitamin D levels in COVID-19 patients can determine the platelet count and MPV of the patients. Discussion: The aforementioned results imply that maintaining an elevated concentration of vitamin D in COVID-19 patients is important because it is associated with a decrease in MPV, which in turn reduces susceptibility to diseases such as coronary artery disease.
Ethics statement Ethical principles were followed based on the ethical protocol approved by the Ethics Committee at Semnan University of Medical Sciences, Semnan, Iran (IR.SEMUMS.REC.1401.309). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions AT: Data curation, Investigation, Writingoriginal draft. HG: Conceptualization, Methodology, Visualization, Writingoriginal draft. KG: Software, Validation, Writingoriginal draft. SY: Formal analysis, Methodology, Software, Writingoriginal draft. BY: Project administration, Resources, Supervision, Writingoriginal
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aihara, Azuma, Akaike, Ikeda, Yamashita et al., Disruption of nuclear vitamin D receptor gene causes enhanced thrombogenicity in mice, J. Biol. Chem, doi:10.1074/jbc.M404865200
Alanli, Kücükay, Yalcin, Relationship between vitamin D levels and platelet count: A retrospective study, Gulhane Med. J, doi:10.4274/gulhane
Amrein, Scherkl, Hoffmann, Neuwersch-Sommeregger, Köstenberger et al., Vitamin D deficiency 2.0: an update on the current status worldwide, Eur. J. Clin. Nutr, doi:10.1038/s41430-020-0558-y
Ates, Kiki, Bilen, Keles, Kocȩr et al., Association of mean platelet volume with the degree of retinopathy in patients with diabetes mellitus, Eur. J. Gen. Med, doi:10.29333/ejgm/82648
Barrett, Bilaloglu, Cornwell, Burgess, Virginio et al., Platelets contribute to disease severity in COVID-19, J. Thromb. Haemostasis, doi:10.1111/jth.15534
Bodnar, Simhan, Catov, Roberts, Platt et al., Maternal vitamin D status and the risk of mild and severe preeclampsia, Epidemiol. (Cambridge Mass), doi:10.1097/EDE.0000000000000039
Chu, Hu, Qi, Li, Zhang et al., Bifunctional effect of the inflammatory cytokine tumor necrosis factor a on megakaryopoiesis and platelet production, J. Thromb. Haemostasis, doi:10.1111/jth.15891
Coban, Bostan, Ozdogan, The mean platelet volume in subjects with impaired fasting glucose, Platelets, doi:10.1080/09537100500220729
Coomes, Haghbayan, Interleukin-6 in COVID-19: a systematic review and meta-analysis, Rev. Med. virology, doi:10.1002/rmv.2141
Cure, Cure, Yuce, Yazici, Karakoyun et al., Mean platelet volume and vitamin D level, Ann. Lab. Med, doi:10.3343/alm.2014.34.2.98
Dai, Zhu, Manson, Song, Li et al., Magnesium status and supplementation influence vitamin D status and metabolism: results from a randomized trial, Am. J. Clin. Nutr, doi:10.1093/ajcn/nqy274
Ghaffari, Rad, Moradi Hasan-Abad, Khosravi, Benvidi et al., Association of the human platelet antigens polymorphisms with platelet count in patients with COVID-19, Front. Med, doi:10.3389/fmed.2023.1265568
Gur, Karadeniz, Genc, Eskicioglu, Yalcin et al., Relationship between mean platelet volume and vitamin D deficiency in gestational diabetes mellitus, Arch. Endocrinol. Metab, doi:10.1590/2359-3997000000063
Harrison, Goodall, Studies on mean platelet volume (MPV)new editorial policy, Platelets, doi:10.1080/09537104.2016.1225467
Jolicoeur, Lamontagne, Impairment of bone marrow pre-B and B cells in MHV3 chronically-infected mice. Corona-and Related Viruses: Current Concepts in Molecular Biology and Pathogenesis, Adv. Exp. Med. Biol, doi:10.1007/978-1-4615-1899-0_33
Kaser, Brandacher, Steurer, Kaser, Offner et al., Interleukin-6 stimulates thrombopoiesis through thrombopoietin: role in inflammatory thrombocytosis, Blood J. Am. Soc. Hematology, doi:10.1182/blood.V98.9.2720
Khazai, Judd, Tangpricha, Calcium and vitamin D: skeletal and extraskeletal health, Curr. Rheumatol. Rep, doi:10.1007/s11926-008-0020-y
Korzonek-Szlacheta, Hudzik, Nowak, Szkodzinski, Nowak et al., Mean platelet volume is associated with serum 25-hydroxyvitamin D concentrations in patients with stable coronary artery disease, Heart Vessels, doi:10.1007/s00380-018-1182-9
Li, Huang, Zou, Yang, Hui et al., Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes, J. Med. virology, doi:10.1002/jmv.26424
Liu, Sun, Guo, Chen, Zhang et al., Association between platelet parameters and mortality in coronavirus disease 2019: Retrospective cohort study, Platelets, doi:10.1080/09537104.2020.1754383
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA network Open, doi:10.1001/jamanetworkopen.2020.19722
Meng, Wei, Chang, Peng, Shi et al., The plateletto-lymphocyte ratio, superior to the neutrophil-to-lymphocyte ratio, correlates with hepatitis C virus infection, Int. J. Infect. Diseases, doi:10.1016/j.ijid.2016.02.025
Park, Kim, Seo, Hong, Cho et al., Inverse relationship between vitamin D levels and platelet indices in Korean adults, Hematology, doi:10.1080/10245332.2017.1318334
Pohl, Behling, Oliver, Kilani, Monson et al., Serum aminotransferase levels and platelet counts as predictors of degree of fibrosis in chronic hepatitis C virus infection, Am. J. gastroenterology, doi:10.1111/j.1572-0241.2001.05268.x
Silvagno, De Vivo, Attanasio, Gallo, Mazzucco et al., Mitochondrial localization of vitamin D receptor in human platelets and differentiated megakaryocytes, PLoS One, doi:10.1371/journal.pone.0008670
Vatandost, Jahani, Afshari, Amiri, Heidarimoghadam et al., Prevalence of vitamin D deficiency in Iran: a systematic review and meta-analysis, Nutr. Health, doi:10.1177/0260106018802968
Wojszel, Czyzewska, Dymicka-Piekarska, Matowicka-Karna, Jakubowska et al., Platelets activation in depending on glycaemic control in diabetes type 2, Polski Merkuriusz Lekarski: Organ Polskiego Towarzystwa Lekarskiego
Yang, Ng, Li, Thrombocytopenia in patients with severe acute respiratory syndrome, Hematology, doi:10.1080/10245330400026170
Yu, Jia, Tang, Liu, Wei, SARS-CoV-2 infection and stem cells: Interaction and intervention, Stem Cell Res, doi:10.1016/j.scr.2020.101859
Zhang, Wu, Zhang, Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak, Curr. Biol, doi:10.1016/j.cub.2020.03.022
Zhong, Peng, Mean platelet volume/platelet count ratio predicts severe pneumonia of COVID-19, J. Clin. Lab. analysis, doi:10.1002/jcla.23607
DOI record:
{
"DOI": "10.3389/fcimb.2024.1360075",
"ISSN": [
"2235-2988"
],
"URL": "http://dx.doi.org/10.3389/fcimb.2024.1360075",
"abstract": "<jats:sec><jats:title>Introduction</jats:title><jats:p>Since there is very little information about the relationship between platelet parameters and vitamin D concentration in patients with COVID-19, the aim of this study is to investigate the relationship between serum vitamin D level and platelet parameters in patients with COVID-19 and to compare these parameters in patients with COVID-19 without vitamin D deficiency and, subsequently, the prognostic value of these parameters in cases of vitamin D deficiency.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>Seven hundred and forty-three patients diagnosed with COVID-19 were enrolled in this study. Patients were divided into two groups: those with and without vitamin D deficiency. The associations between platelet indices and vitamin D levels were analyzed by Pearson’s correlation analysis and a one-way ANOVA test.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Platelet count and mean platelet volume (MPV) were significantly higher in the patients with vitamin D deficiency than in the patients without vitamin D deficiency. There was a significant negative correlation between platelet count and MPV with vitamin D levels in patients with vitamin D deficiency (r = -0.835, P = 0.001 &amp; r = -0.324, P = 0.042, respectively). Vitamin D levels in COVID-19 patients can determine the platelet count and MPV of the patients.</jats:p></jats:sec><jats:sec><jats:title>Discussion</jats:title><jats:p>The aforementioned results imply that maintaining an elevated concentration of vitamin D in COVID-19 patients is important because it is associated with a decrease in MPV, which in turn reduces susceptibility to diseases such as coronary artery disease.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fcimb.2024.1360075"
],
"author": [
{
"affiliation": [],
"family": "Talebzadeh",
"given": "Amirhossein",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ghaffari",
"given": "Hadi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ghaffari",
"given": "Kazem",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yazdanpanah",
"given": "Sorur",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yousefi Goltappeh",
"given": "Bahman",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Eslami",
"given": "Majid",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ghasemi",
"given": "Ali",
"sequence": "additional"
}
],
"container-title": "Frontiers in Cellular and Infection Microbiology",
"container-title-short": "Front. Cell. Infect. Microbiol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2024,
3,
8
]
],
"date-time": "2024-03-08T04:32:12Z",
"timestamp": 1709872332000
},
"deposited": {
"date-parts": [
[
2024,
3,
8
]
],
"date-time": "2024-03-08T04:32:15Z",
"timestamp": 1709872335000
},
"indexed": {
"date-parts": [
[
2024,
3,
9
]
],
"date-time": "2024-03-09T00:41:13Z",
"timestamp": 1709944873206
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
3,
8
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
3,
8
]
],
"date-time": "2024-03-08T00:00:00Z",
"timestamp": 1709856000000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fcimb.2024.1360075/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2024,
3,
8
]
]
},
"published-online": {
"date-parts": [
[
2024,
3,
8
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1074/jbc.M404865200",
"article-title": "Disruption of nuclear vitamin D receptor gene causes enhanced thrombogenicity in mice",
"author": "Aihara",
"doi-asserted-by": "publisher",
"first-page": "35798",
"journal-title": "J. Biol. Chem.",
"key": "B1",
"volume": "279",
"year": "2004"
},
{
"DOI": "10.4274/gulhane",
"article-title": "Relationship between vitamin D levels and platelet count: A retrospective study",
"author": "Alanli",
"doi-asserted-by": "publisher",
"first-page": "174",
"journal-title": "Gulhane Med. J.",
"key": "B2",
"volume": "62",
"year": "2020"
},
{
"DOI": "10.1038/s41430-020-0558-y",
"article-title": "Vitamin D deficiency 2.0: an update on the current status worldwide",
"author": "Amrein",
"doi-asserted-by": "publisher",
"first-page": "1498",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "B3",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.29333/ejgm/82648",
"article-title": "Association of mean platelet volume with the degree of retinopathy in patients with diabetes mellitus",
"author": "Ateş",
"doi-asserted-by": "publisher",
"first-page": "99",
"journal-title": "Eur. J. Gen. Med.",
"key": "B4",
"volume": "6",
"year": "2009"
},
{
"DOI": "10.1111/jth.15534",
"article-title": "Platelets contribute to disease severity in COVID-19",
"author": "Barrett",
"doi-asserted-by": "publisher",
"first-page": "3139",
"journal-title": "J. Thromb. Haemostasis.",
"key": "B5",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1097/EDE.0000000000000039",
"article-title": "Maternal vitamin D status and the risk of mild and severe preeclampsia",
"author": "Bodnar",
"doi-asserted-by": "publisher",
"first-page": "207",
"journal-title": "Epidemiol. (Cambridge Mass).",
"key": "B6",
"volume": "25",
"year": "2014"
},
{
"DOI": "10.1111/jth.15891",
"article-title": "Bifunctional effect of the inflammatory cytokine tumor necrosis factor α on megakaryopoiesis and platelet production",
"author": "Chu",
"doi-asserted-by": "publisher",
"first-page": "2998",
"journal-title": "J. Thromb. Haemostasis.",
"key": "B7",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1080/09537100500220729",
"article-title": "The mean platelet volume in subjects with impaired fasting glucose",
"author": "Coban",
"doi-asserted-by": "publisher",
"first-page": "67",
"journal-title": "Platelets.",
"key": "B8",
"volume": "17",
"year": "2006"
},
{
"DOI": "10.1002/rmv.2141",
"article-title": "Interleukin-6 in COVID-19: a systematic review and meta-analysis",
"author": "Coomes",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Rev. Med. virology.",
"key": "B9",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.3343/alm.2014.34.2.98",
"article-title": "Mean platelet volume and vitamin D level",
"author": "Cure",
"doi-asserted-by": "publisher",
"first-page": "98",
"journal-title": "Ann. Lab. Med.",
"key": "B10",
"volume": "34",
"year": "2014"
},
{
"DOI": "10.1093/ajcn/nqy274",
"article-title": "Magnesium status and supplementation influence vitamin D status and metabolism: results from a randomized trial",
"author": "Dai",
"doi-asserted-by": "publisher",
"first-page": "1249",
"journal-title": "Am. J. Clin. Nutr.",
"key": "B11",
"volume": "108",
"year": "2018"
},
{
"DOI": "10.3389/fmed.2023.1265568",
"article-title": "Association of the human platelet antigens polymorphisms with platelet count in patients with COVID-19",
"author": "Ghaffari",
"doi-asserted-by": "publisher",
"journal-title": "Front. Med.",
"key": "B12",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.1590/2359-3997000000063",
"article-title": "Relationship between mean platelet volume and vitamin D deficiency in gestational diabetes mellitus",
"author": "Gur",
"doi-asserted-by": "publisher",
"first-page": "448",
"journal-title": "Arch. Endocrinol. Metab.",
"key": "B13",
"volume": "59",
"year": "2015"
},
{
"DOI": "10.1080/09537104.2016.1225467",
"article-title": "Studies on mean platelet volume (MPV)-new editorial policy",
"author": "Harrison",
"doi-asserted-by": "publisher",
"first-page": "605",
"journal-title": "Platelets.",
"key": "B14",
"volume": "27",
"year": "2016"
},
{
"article-title": "Impairment of bone marrow pre-B and B cells in MHV3 chronically-infected mice. Corona-and Related Viruses: Current Concepts in Molecular Biology and Pathogenesis",
"author": "Jolicoeur",
"key": "B15",
"volume-title": "Adv. Exp. Med. Biol.",
"year": "1995"
},
{
"DOI": "10.1182/blood.V98.9.2720",
"article-title": "Interleukin-6 stimulates thrombopoiesis through thrombopoietin: role in inflammatory thrombocytosis",
"author": "Kaser",
"doi-asserted-by": "publisher",
"first-page": "2720",
"journal-title": "Blood J. Am. Soc. Hematology.",
"key": "B16",
"volume": "98",
"year": "2001"
},
{
"DOI": "10.1007/s11926-008-0020-y",
"article-title": "Calcium and vitamin D: skeletal and extraskeletal health",
"author": "Khazai",
"doi-asserted-by": "publisher",
"first-page": "110",
"journal-title": "Curr. Rheumatol. Rep.",
"key": "B17",
"volume": "10",
"year": "2008"
},
{
"DOI": "10.1007/s00380-018-1182-9",
"article-title": "Mean platelet volume is associated with serum 25-hydroxyvitamin D concentrations in patients with stable coronary artery disease",
"author": "Korzonek-Szlacheta",
"doi-asserted-by": "publisher",
"first-page": "1275",
"journal-title": "Heart Vessels.",
"key": "B18",
"volume": "33",
"year": "2018"
},
{
"DOI": "10.1002/jmv.26424",
"article-title": "Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1449",
"journal-title": "J. Med. virology.",
"key": "B19",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1080/09537104.2020.1754383",
"article-title": "Association between platelet parameters and mortality in coronavirus disease 2019: Retrospective cohort study",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "490",
"journal-title": "Platelets.",
"key": "B20",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"article-title": "Association of vitamin D status and other clinical characteristics with COVID-19 test results",
"author": "Meltzer",
"doi-asserted-by": "publisher",
"first-page": "e2019722",
"journal-title": "JAMA network Open",
"key": "B21",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2016.02.025",
"article-title": "The platelet-to-lymphocyte ratio, superior to the neutrophil-to-lymphocyte ratio, correlates with hepatitis C virus infection",
"author": "Meng",
"doi-asserted-by": "publisher",
"first-page": "72",
"journal-title": "Int. J. Infect. Diseases.",
"key": "B22",
"volume": "45",
"year": "2016"
},
{
"DOI": "10.1080/10245332.2017.1318334",
"article-title": "Inverse relationship between vitamin D levels and platelet indices in Korean adults",
"author": "Park",
"doi-asserted-by": "publisher",
"first-page": "623",
"journal-title": "Hematology.",
"key": "B23",
"volume": "22",
"year": "2017"
},
{
"DOI": "10.1111/j.1572-0241.2001.05268.x",
"article-title": "Serum aminotransferase levels and platelet counts as predictors of degree of fibrosis in chronic hepatitis C virus infection",
"author": "Pohl",
"doi-asserted-by": "publisher",
"first-page": "3142",
"journal-title": "Am. J. gastroenterology.",
"key": "B24",
"volume": "96",
"year": "2001"
},
{
"DOI": "10.1371/journal.pone.0008670",
"article-title": "Mitochondrial localization of vitamin D receptor in human platelets and differentiated megakaryocytes",
"author": "Silvagno",
"doi-asserted-by": "publisher",
"journal-title": "PLoS One",
"key": "B25",
"volume": "5",
"year": "2010"
},
{
"DOI": "10.1177/0260106018802968",
"article-title": "Prevalence of vitamin D deficiency in Iran: a systematic review and meta-analysis",
"author": "Vatandost",
"doi-asserted-by": "publisher",
"first-page": "269",
"journal-title": "Nutr. Health",
"key": "B26",
"volume": "24",
"year": "2018"
},
{
"article-title": "Platelets activation in depending on glycaemic control in diabetes type 2",
"author": "Wojszel",
"first-page": "335",
"journal-title": "Polski Merkuriusz Lekarski: Organ Polskiego Towarzystwa Lekarskiego.",
"key": "B27",
"volume": "25",
"year": "2008"
},
{
"DOI": "10.1080/10245330400026170",
"article-title": "Thrombocytopenia in patients with severe acute respiratory syndrome",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "101",
"journal-title": "Hematology.",
"key": "B28",
"volume": "10",
"year": "2005"
},
{
"DOI": "10.1016/j.scr.2020.101859",
"article-title": "SARS-CoV-2 infection and stem cells: Interaction and intervention",
"author": "Yu",
"doi-asserted-by": "publisher",
"first-page": "101859",
"journal-title": "Stem Cell Res.",
"key": "B29",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.cub.2020.03.022",
"article-title": "Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "1346",
"journal-title": "Curr. Biol.",
"key": "B30",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1002/jcla.23607",
"article-title": "Mean platelet volume/platelet count ratio predicts severe pneumonia of COVID-19",
"author": "Zhong",
"doi-asserted-by": "publisher",
"journal-title": "J. Clin. Lab. analysis.",
"key": "B31",
"volume": "35",
"year": "2021"
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fcimb.2024.1360075/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Microbiology (medical)",
"Immunology",
"Microbiology"
],
"subtitle": [],
"title": "The effect of vitamin D deficiency on platelet parameters in patients with COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "14"
}
