Physical Activity Modifies the Severity of COVID-19 in Hospitalized Patients—Observational Study
et al., Journal of Clinical Medicine, doi:10.3390/jcm12124046, NCT05200767, Jun 2023
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 131 hospitalized patients in Poland, showing lower mortality and improved recovery with a history of higher physical activity.
|
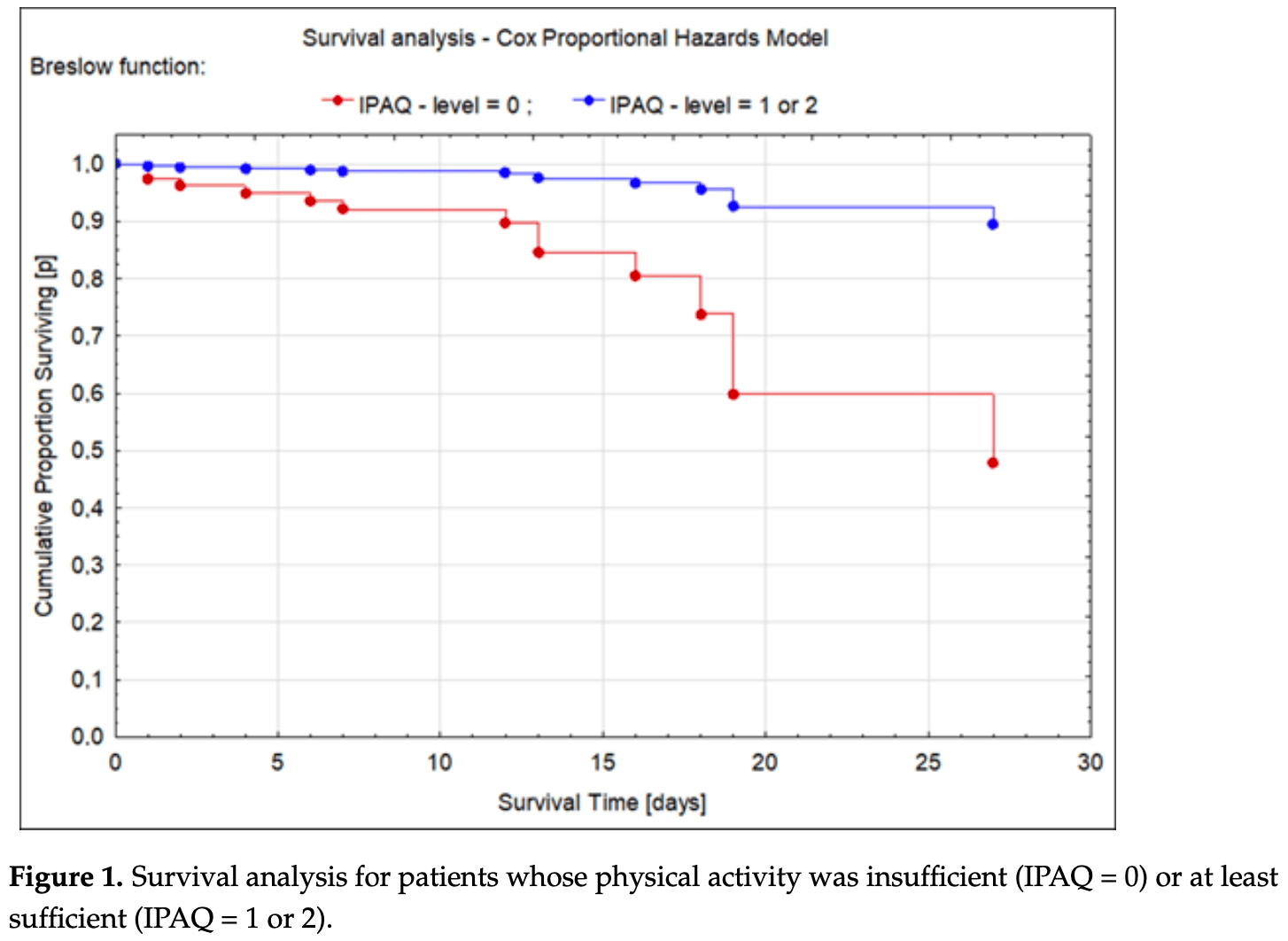
risk of death, 62.0% lower, HR 0.38, p = 0.21, high activity levels 71, low activity levels 60, inverted to make HR<1 favor high activity levels, IPAQ 1/2 vs. IPAQ 0, Cox proportional hazards.
|
|
risk of no recovery, 61.0% lower, HR 0.39, p = 0.19, high activity levels 71, low activity levels 60, IPAQ 1/2 vs. IPAQ 0, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sutkowska et al., 14 Jun 2023, prospective, Poland, peer-reviewed, 14 authors, study period 31 January, 2022 - 11 February, 2022, trial NCT05200767 (history).
Contact: edyta.sutkowska@umw.edu.pl (corresponding author), astanek@tlen.pl, grzegorz.k.jakubiak@gmail.com, katarzyna.madziarska@umw.edu.pl, mmadziarski@usk.wroc.pl, ksutkowska@usk.wroc.pl, adrianna.borowkow@gmail.com, justyna.mazurek@umw.edu.pl.
Physical Activity Modifies the Severity of COVID-19 in Hospitalized Patients—Observational Study
Journal of Clinical Medicine, doi:10.3390/jcm12124046
Background and aim: Physical activity (PA) can modulate the immune response, but its impact on infectious disease severity is unknown. We assess if the PA level impacts the severity of COVID-19. Methods: Prospective, cohort study for adults hospitalized due to COVID-19, who filled out the International Physical Activity Questionnaire (IPAQ). Disease severity was expressed as death, transfer to intensive care unit (ICU), oxygen therapy (OxTh), hospitalization length, complications, C-reactive protein, and procalcitonin level. Results: Out of 326 individuals, 131 (57; 43.51% women) were analyzed: age: median-70; range: 20-95; BMI: mean-27.18 kg/m 2 ; and SD: ±4.77. During hospitalization: 117 (83.31%) individuals recovered, nine (6.87%) were transferred to ICU, five (3.82%) died, and 83 (63.36%) needed OxTh. The median for the hospital stay was 11 (range: 3-49) for discharged patients, and mean hospitalization length was 14 (SD: ±5.8312) for deaths and 14.22 days (SD: ±6.92) for ICU-transferred patients. The median for MET-min/week was 660 (range: 0-19,200). Sufficient or high PA was found in recovered patients but insufficient PA was observed in dead or ICU-transferred patients (p = 0.03). The individuals with poor PA had a higher risk of death (HR = 2.63; ±95%CI 0.58-11.93; p = 0.037). OxTh was used more often in the less active individuals (p = 0.03). The principal component analysis confirmed a relationship between insufficient PA and an unfavorable course of the disease. Conclusion: A higher level of PA is associated with a milder course of COVID-19.
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflict of interest.
References
Alves, Lomba, Gonçalves-De-Albuquerque, Burth, Irisin, None, doi:10.3389/fendo.2022.879066
Biernat, Stupnicki, Gajewski, International Physical Activity Questionnaire (IPAQ)-Polish version, Wych Fiz. Spor
Biscarini, Colaneri, Ludovisi, Seminari, Pieri et al., The obesity paradox: Analysis from the SMAtteo COvid-19 REgistry (SMACORE) cohort, Nutr. Metab. Cardiovasc. Dis, doi:10.1016/j.numecd.2020.07.047
Borghouts, Keizer, Exercise and insulin sensitivity: A review, Int. J. Sports Med, doi:10.1055/s-2000-8847
Brodin, Immune determinants of COVID-19 disease presentation and severity, Nat. Med. 2021, doi:10.1038/s41591-020-01202-8
Chandarana, Pisuchpen, Krieger, Dane, Mikheev et al., Association of body composition parameters measured on CT with risk of hospitalization in patients with Covid-19, Eur. J. Radiol
Chen, Stevinson, Ku, Chang, Chu, Relationships of leisure-time and non-leisure-time physical activity with depressive symptoms: A population-based study of Taiwanese older adults, Int. J. Behav. Nutr. Phys. Act
Craig, Marshall, Sjöström, Bauman, Booth et al., International physical activity questionnaire: 12-country reliability and validity, Med. Sci. Sports Exerc, doi:10.1249/01.MSS.0000078924.61453.FB
De Candia, Prattichizzo, Garavelli, Matarese, Cells, Warriors of SARS-CoV-2 infection, doi:10.1016/j.it.2020.11.002
De Sanctis, Ruggiero, Soliman, Daar, Di Maio et al., Coronavirus Disease 2019 (COVID-19) in adolescents: An update on current clinical and diagnostic characteristics, Acta Biomed, doi:10.23750/abm.v91i2.9543
Denay, Breslow, Turner, Nieman, Roberts et al., ACSM call to action statement: COVID-19 considerations for sports and physical activity, Curr. Sports Med. Rep, doi:10.1249/JSR.0000000000000739
Dutra, Da-Silva, Mineo, Turner, Editorial: The effects of physical activity and exercise on immune responses to infection, Front. Immunol, doi:10.3389/fimmu.2022.842568
Fezeu, Julia, Henegar, Bitu, Hu et al., Obesity is associated with higher risk of intensive care unit admission and death in influenza A (H1N1) patients: A systematic review and meta-analysis, Obes. Rev, doi:10.1111/j.1467-789X.2011.00864.x
Fox, The influence of physical activity on mental well-being, Public Health Nutr, doi:10.1017/S1368980099000567
Hu, Huang, Yin, The cytokine storm and COVID-19, J. Med. Virol, doi:10.1002/jmv.26232
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, Lancet, doi:10.1016/S0140-6736(20)30183-5
Jakobsson, Cotgreave, Furberg, Arnberg, Svensson, Potential physiological and cellular mechanisms of exercise that decrease the risk of severe complications and mortality following SARS-CoV-2 infection. Sports 2021, doi:10.3390/sports9090121
Lan, Chang, Tai, Relationship between components of leisure physical activity and mortality in Taiwanese older adults, Prev. Med, doi:10.1016/j.ypmed.2006.03.016
Lim, Lee, Jeong, Han, Association of Physical Activity with SARS-CoV-2 Infection and Severe Clinical Outcomes Among Patients in South Korea, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2023.9840
Martinez-Gomez, Guallar-Castillon, Garcia-Esquinas, Bandinelli, Rodríguez-Artalejo, Physical activity and the effect of multimorbidity on all-cause mortality in older adults, Mayo Clin. Proc, doi:10.1016/j.mayocp.2016.12.004
Molanorouzi, Khoo, Morris, Motives for adult participation in physical activity: Type of activity, age, and gender, doi:10.1186/s12889-015-1429-7
Myers, Kokkinos, Nyelin, Physical activity, cardiorespiratory fitness, and the metabolic syndrome, Nutrients, doi:10.3390/nu11071652
Nieman, Coronavirus disease-2019: A tocsin to our aging, unfit, corpulent, and immunodeficient society, J. Sport Health Sci, doi:10.1016/j.jshs.2020.05.001
Nieman, Exercise Is Medicine for Immune Function: Implication for COVID-19, Curr. Sports Med. Rep
Nieman, Pence, Exercise immunology: Future directions, J. Sport Health Sci, doi:10.1016/j.jshs.2019.12.003
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J. Sport Health Sci, doi:10.1016/j.jshs.2018.09.009
Novotová, Pavl Ů, Dvořáčková, Arnal-Gómez, Espí-López, Influence of walking as physiological training to improve respiratory parameters in the elderly population, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19137995
Pedersen, Febbraio, Muscle as an endocrine organ: Focus on muscle-derived interleukin-6, Physiol. Rev, doi:10.1152/physrev.90100.2007
Posadzki, Pieper, Bajpai, Makaruk, Könsgen et al., Exercise/physical activity and health outcomes: An overview of Cochrane systematic reviews, BMC Public Health, doi:10.1186/s12889-020-09855-3
Puciato, Sociodemographic associations of physical activity in people of working age, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph16122134
Romero Starke, Reissig, Petereit-Haack, Schmauder, Nienhaus et al., The isolated effect of age on the risk of COVID-19 severe outcomes: A systematic review with meta-analysis, BMJ Glob, doi:10.1136/bmjgh-2021-006434
Rothschild, Islam, Bishop, Kilding, Stewart et al., Factors influencing AMPK activation during cycling exercise: A pooled analysis and meta-regression, Sports Med, doi:10.1007/s40279-021-01610-x
Rottoli, Bernante, Belvedere, Balsamo, Garelli et al., How important is obesity as a risk factor for respiratory failure, intensive care admission and death in hospitalised COVID-19 patients? Results from a single Italian centre, Eur. J. Endocrinol, doi:10.1530/EJE-20-0541
Rütten, Vuillemin, Ooijendijk, Schena, Sjöströmet et al., Physical activity monitoring in Europe. The European Physical Activity Surveillance System (EUPASS) approach and indicator testing, Public Health Nutr, doi:10.1079/PHN2002449
Schnohr, O'keefe, Marott, Lange, Jensen, Dose of jogging and long-term mortality: The Copenhagen City Heart Study, J. Am. Coll. Cardiol, doi:10.1016/j.jacc.2014.11.023
Sette, Crotty, Adaptive immunity to SARS-CoV-2 and COVID-19, Cell, doi:10.1016/j.cell.2021.01.007
Simonnet, Chetboun, Poissy, Raverdy, Noulette et al., High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obesity, doi:10.1002/oby.22831
Simpson, Kunz, Agha, Graff, Exercise and the regulation of immune functions, Prog. Mol. Biol. Transl. Sci, doi:10.1016/bs.pmbts.2015.08.001
Vancampfort, Koyanagi, Ward, Rosenbaum, Schuch et al., Chronic physical conditions, multimorbidity and physical activity across 46 low-and middle-income countries, Int. J. Behav. Nutr. Phys. Act, doi:10.1186/s12966-017-0463-5
Wu, Chen, Cai, Xia, Zhou et al., Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.0994
Yang, Ding, Zou, Shen, Hu et al., Visceral adiposity and high intramuscular fat deposition independently predict critical illness in patients with SARS-CoV-2, Obesity, doi:10.1002/oby.22971
DOI record:
{
"DOI": "10.3390/jcm12124046",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm12124046",
"abstract": "<jats:p>Background and aim: Physical activity (PA) can modulate the immune response, but its impact on infectious disease severity is unknown. We assess if the PA level impacts the severity of COVID-19. Methods: Prospective, cohort study for adults hospitalized due to COVID-19, who filled out the International Physical Activity Questionnaire (IPAQ). Disease severity was expressed as death, transfer to intensive care unit (ICU), oxygen therapy (OxTh), hospitalization length, complications, C-reactive protein, and procalcitonin level. Results: Out of 326 individuals, 131 (57; 43.51% women) were analyzed: age: median—70; range: 20–95; BMI: mean—27.18 kg/m²; and SD: ±4.77. During hospitalization: 117 (83.31%) individuals recovered, nine (6.87%) were transferred to ICU, five (3.82%) died, and 83 (63.36%) needed OxTh. The median for the hospital stay was 11 (range: 3–49) for discharged patients, and mean hospitalization length was 14 (SD: ±5.8312) for deaths and 14.22 days (SD: ±6.92) for ICU-transferred patients. The median for MET-min/week was 660 (range: 0–19,200). Sufficient or high PA was found in recovered patients but insufficient PA was observed in dead or ICU-transferred patients (p = 0.03). The individuals with poor PA had a higher risk of death (HR = 2.63; ±95%CI 0.58–11.93; p = 0.037). OxTh was used more often in the less active individuals (p = 0.03). The principal component analysis confirmed a relationship between insufficient PA and an unfavorable course of the disease. Conclusion: A higher level of PA is associated with a milder course of COVID-19.</jats:p>",
"alternative-id": [
"jcm12124046"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-1602-8978",
"affiliation": [
{
"name": "University Rehabilitation Centre, Wroclaw Medical University, 50-556 Wroclaw, Poland"
}
],
"authenticated-orcid": false,
"family": "Sutkowska",
"given": "Edyta",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-6939-9898",
"affiliation": [
{
"name": "Department and Clinic of Internal Medicine, Angiology, and Physical Medicine, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, 41-902 Bytom, Poland"
}
],
"authenticated-orcid": false,
"family": "Stanek",
"given": "Agata",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3624-3691",
"affiliation": [
{
"name": "Clinical Department of Nephrology and Transplantation Medicine, Wroclaw Medical University, 50-556 Wroclaw, Poland"
}
],
"authenticated-orcid": false,
"family": "Madziarska",
"given": "Katarzyna",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0039-8306",
"affiliation": [
{
"name": "Department and Clinic of Internal Medicine, Angiology, and Physical Medicine, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, 41-902 Bytom, Poland"
}
],
"authenticated-orcid": false,
"family": "Jakubiak",
"given": "Grzegorz K.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2992-5499",
"affiliation": [
{
"name": "Clinical Department of Emergency Medicine, Wroclaw Medical University, 50-556 Wroclaw, Poland"
}
],
"authenticated-orcid": false,
"family": "Sokołowski",
"given": "Janusz",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Department of Rheumatology and Internal Medicine, University Hospital, 50-556 Wroclaw, Poland"
}
],
"family": "Madziarski",
"given": "Marcin",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8459-4103",
"affiliation": [
{
"name": "Department of General, Minimally Invasive and Endocrine Surgery, University Hospital, 50-556 Wroclaw, Poland"
}
],
"authenticated-orcid": false,
"family": "Sutkowska-Stępień",
"given": "Karolina",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1556-0177",
"affiliation": [
{
"name": "University Rehabilitation Centre, Wroclaw Medical University, 50-556 Wroclaw, Poland"
}
],
"authenticated-orcid": false,
"family": "Biernat",
"given": "Karolina",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8983-0286",
"affiliation": [
{
"name": "University Rehabilitation Centre, Wroclaw Medical University, 50-556 Wroclaw, Poland"
}
],
"authenticated-orcid": false,
"family": "Mazurek",
"given": "Justyna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Angiology and Physical Medicine, Specialist Hospital No.2, 41-902 Bytom, Poland"
}
],
"family": "Borowkow-Bulek",
"given": "Adrianna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Postgraduate–Internship, University Hospital, 50-556 Wrocław, Poland"
}
],
"family": "Czyżewski",
"given": "Jakub",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Postgraduate–Internship, University Hospital, 50-556 Wrocław, Poland"
}
],
"family": "Wilk",
"given": "Gabriela",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Postgraduate–Internship, University Hospital, 50-556 Wrocław, Poland"
}
],
"family": "Jagasyk",
"given": "Arkadiusz",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Drugs Form Technology, Wroclaw Medical University, 50-556 Wroclaw, Poland"
}
],
"family": "Marciniak",
"given": "Dominik",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
6,
15
]
],
"date-time": "2023-06-15T06:03:19Z",
"timestamp": 1686808999000
},
"deposited": {
"date-parts": [
[
2023,
6,
15
]
],
"date-time": "2023-06-15T07:59:19Z",
"timestamp": 1686815959000
},
"indexed": {
"date-parts": [
[
2023,
6,
16
]
],
"date-time": "2023-06-16T04:20:27Z",
"timestamp": 1686889227973
},
"is-referenced-by-count": 0,
"issue": "12",
"issued": {
"date-parts": [
[
2023,
6,
14
]
]
},
"journal-issue": {
"issue": "12",
"published-online": {
"date-parts": [
[
2023,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
14
]
],
"date-time": "2023-06-14T00:00:00Z",
"timestamp": 1686700800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/12/12/4046/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "4046",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
6,
14
]
]
},
"published-online": {
"date-parts": [
[
2023,
6,
14
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "ref_1",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1530/EJE-20-0541",
"article-title": "How important is obesity as a risk factor for respiratory failure, intensive care admission and death in hospitalised COVID-19 patients? Results from a single Italian centre",
"author": "Rottoli",
"doi-asserted-by": "crossref",
"first-page": "389",
"journal-title": "Eur. J. Endocrinol.",
"key": "ref_2",
"volume": "183",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"article-title": "Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "1031",
"journal-title": "JAMA Intern. Med.",
"key": "ref_3",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1136/bmjgh-2021-006434",
"article-title": "The isolated effect of age on the risk of COVID-19 severe outcomes: A systematic review with meta-analysis",
"author": "Reissig",
"doi-asserted-by": "crossref",
"first-page": "e006434",
"journal-title": "BMJ Glob. Health",
"key": "ref_4",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1186/s12889-015-1429-7",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Molanorouzi, K., Khoo, S., and Morris, T. (2015). Motives for adult participation in physical activity: Type of activity, age, and gender. BMC Public Health, 15."
},
{
"DOI": "10.3390/ijerph16122134",
"doi-asserted-by": "crossref",
"key": "ref_6",
"unstructured": "Puciato, D. (2019). Sociodemographic associations of physical activity in people of working age. Int. J. Environ. Res. Public Health, 16."
},
{
"article-title": "Coronavirus Disease 2019 (COVID-19) in adolescents: An update on current clinical and diagnostic characteristics",
"author": "Ruggiero",
"first-page": "184",
"journal-title": "Acta Biomed.",
"key": "ref_7",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1186/s12889-020-09855-3",
"doi-asserted-by": "crossref",
"key": "ref_8",
"unstructured": "Posadzki, P., Pieper, D., Bajpai, R., Makaruk, H., Könsgen, N., Neuhaus, A.L., and Semwal, M. (2020). Exercise/physical activity and health outcomes: An overview of Cochrane systematic reviews. BMC Public Health, 20."
},
{
"DOI": "10.1016/j.ypmed.2006.03.016",
"article-title": "Relationship between components of leisure physical activity and mortality in Taiwanese older adults",
"author": "Lan",
"doi-asserted-by": "crossref",
"first-page": "36",
"journal-title": "Prev. Med.",
"key": "ref_9",
"volume": "43",
"year": "2006"
},
{
"DOI": "10.1017/S1368980099000567",
"article-title": "The influence of physical activity on mental well-being",
"author": "Fox",
"doi-asserted-by": "crossref",
"first-page": "411",
"journal-title": "Public Health Nutr.",
"key": "ref_10",
"volume": "2",
"year": "1999"
},
{
"DOI": "10.1186/1479-5868-9-28",
"article-title": "Relationships of leisure-time and non-leisure-time physical activity with depressive symptoms: A population-based study of Taiwanese older adults",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "28",
"journal-title": "Int. J. Behav. Nutr. Phys. Act.",
"key": "ref_11",
"volume": "14",
"year": "2012"
},
{
"DOI": "10.1016/j.it.2020.11.002",
"article-title": "T cells: Warriors of SARS-CoV-2 infection",
"author": "Prattichizzo",
"doi-asserted-by": "crossref",
"first-page": "18",
"journal-title": "Trends Immunol.",
"key": "ref_12",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1038/s41591-020-01202-8",
"article-title": "Immune determinants of COVID-19 disease presentation and severity",
"author": "Brodin",
"doi-asserted-by": "crossref",
"first-page": "28",
"journal-title": "Nat. Med.",
"key": "ref_13",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2021.01.007",
"article-title": "Adaptive immunity to SARS-CoV-2 and COVID-19",
"author": "Sette",
"doi-asserted-by": "crossref",
"first-page": "861",
"journal-title": "Cell",
"key": "ref_14",
"volume": "184",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2022.842568",
"article-title": "Editorial: The effects of physical activity and exercise on immune responses to infection",
"author": "Dutra",
"doi-asserted-by": "crossref",
"first-page": "842568",
"journal-title": "Front. Immunol.",
"key": "ref_15",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"article-title": "The compelling link between physical activity and the body’s defense system",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "201",
"journal-title": "J. Sport Health Sci.",
"key": "ref_16",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1249/JSR.0000000000000739",
"article-title": "ACSM call to action statement: COVID-19 considerations for sports and physical activity",
"author": "Denay",
"doi-asserted-by": "crossref",
"first-page": "326",
"journal-title": "Curr. Sports Med. Rep.",
"key": "ref_17",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1016/j.jshs.2020.05.001",
"article-title": "Coronavirus disease-2019: A tocsin to our aging, unfit, corpulent, and immunodeficient society",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "293",
"journal-title": "J. Sport Health Sci.",
"key": "ref_18",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26232",
"article-title": "The cytokine storm and COVID-19",
"author": "Hu",
"doi-asserted-by": "crossref",
"first-page": "250",
"journal-title": "J. Med. Virol.",
"key": "ref_19",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1249/JSR.0000000000000867",
"article-title": "Exercise Is Medicine for Immune Function: Implication for COVID-19",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "395",
"journal-title": "Curr. Sports Med. Rep.",
"key": "ref_20",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1007/s40279-021-01610-x",
"article-title": "Factors influencing AMPK activation during cycling exercise: A pooled analysis and meta-regression",
"author": "Rothschild",
"doi-asserted-by": "crossref",
"first-page": "1273",
"journal-title": "Sports Med.",
"key": "ref_21",
"volume": "52",
"year": "2022"
},
{
"DOI": "10.3389/fendo.2022.879066",
"article-title": "Irisin, exercise, and COVID-19",
"author": "Alves",
"doi-asserted-by": "crossref",
"first-page": "879066",
"journal-title": "Front. Endocrinol.",
"key": "ref_22",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.jshs.2019.12.003",
"article-title": "Exercise immunology: Future directions",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "432",
"journal-title": "J. Sport Health Sci.",
"key": "ref_23",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2014.11.023",
"article-title": "Dose of jogging and long-term mortality: The Copenhagen City Heart Study",
"author": "Schnohr",
"doi-asserted-by": "crossref",
"first-page": "411",
"journal-title": "J. Am. Coll. Cardiol.",
"key": "ref_24",
"volume": "65",
"year": "2015"
},
{
"DOI": "10.3390/nu11071652",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Myers, J., Kokkinos, P., and Nyelin, E. (2019). Physical activity, cardiorespiratory fitness, and the metabolic syndrome. Nutrients, 11."
},
{
"DOI": "10.1249/01.MSS.0000078924.61453.FB",
"article-title": "International physical activity questionnaire: 12-country reliability and validity",
"author": "Craig",
"doi-asserted-by": "crossref",
"first-page": "1381",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "ref_26",
"volume": "35",
"year": "2003"
},
{
"article-title": "International Physical Activity Questionnaire (IPAQ)-Polish version",
"author": "Biernat",
"first-page": "47",
"journal-title": "Wych Fiz. Spor.",
"key": "ref_27",
"volume": "51",
"year": "2007"
},
{
"DOI": "10.1079/PHN2002449",
"article-title": "Physical activity monitoring in Europe. The European Physical Activity Surveillance System (EUPASS) approach and indicator testing",
"author": "Vuillemin",
"doi-asserted-by": "crossref",
"first-page": "377",
"journal-title": "Public Health Nutr.",
"key": "ref_28",
"volume": "6",
"year": "2003"
},
{
"DOI": "10.1055/s-2000-8847",
"article-title": "Exercise and insulin sensitivity: A review",
"author": "Borghouts",
"doi-asserted-by": "crossref",
"first-page": "302",
"journal-title": "Int. J. Sports Med.",
"key": "ref_29",
"volume": "21",
"year": "2000"
},
{
"DOI": "10.1152/physrev.90100.2007",
"article-title": "Muscle as an endocrine organ: Focus on muscle-derived interleukin-6",
"author": "Pedersen",
"doi-asserted-by": "crossref",
"first-page": "1379",
"journal-title": "Physiol. Rev.",
"key": "ref_30",
"volume": "88",
"year": "2008"
},
{
"key": "ref_31",
"unstructured": "(2022, June 12). IPAQ International Physical Activity Questionaire. Available online: https://www.physio-pedia.com/images/c/c7/Quidelines_for_interpreting_the_IPAQ.pdf."
},
{
"DOI": "10.3390/ijerph19137995",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Novotová, K., Pavlů, D., Dvořáčková, D., Arnal-Gómez, A., and Espí-López, G.V. (2022). Influence of walking as physiological training to improve respiratory parameters in the elderly population. Int. J. Environ. Res. Public Health, 19."
},
{
"key": "ref_33",
"unstructured": "(2022, November 10). Available online: https://virtual.cvot.org/wp-content/uploads/2022/11/CVOT_Summit_2022_Programme_Booklet.pdf."
},
{
"DOI": "10.1016/j.mayocp.2016.12.004",
"article-title": "Physical activity and the effect of multimorbidity on all-cause mortality in older adults",
"author": "Bandinelli",
"doi-asserted-by": "crossref",
"first-page": "376",
"journal-title": "Mayo Clin. Proc.",
"key": "ref_34",
"volume": "92",
"year": "2017"
},
{
"DOI": "10.1186/s12966-017-0463-5",
"article-title": "Chronic physical conditions, multimorbidity and physical activity across 46 low-and middle-income countries",
"author": "Vancampfort",
"doi-asserted-by": "crossref",
"first-page": "6",
"journal-title": "Int. J. Behav. Nutr. Phys. Act.",
"key": "ref_35",
"volume": "14",
"year": "2017"
},
{
"DOI": "10.1016/bs.pmbts.2015.08.001",
"article-title": "Exercise and the regulation of immune functions",
"author": "Simpson",
"doi-asserted-by": "crossref",
"first-page": "355",
"journal-title": "Prog. Mol. Biol. Transl. Sci.",
"key": "ref_36",
"volume": "135",
"year": "2015"
},
{
"DOI": "10.1111/j.1467-789X.2011.00864.x",
"article-title": "Obesity is associated with higher risk of intensive care unit admission and death in influenza A (H1N1) patients: A systematic review and meta-analysis",
"author": "Fezeu",
"doi-asserted-by": "crossref",
"first-page": "653",
"journal-title": "Obes. Rev.",
"key": "ref_37",
"volume": "12",
"year": "2011"
},
{
"DOI": "10.1016/j.numecd.2020.07.047",
"article-title": "The obesity paradox: Analysis from the SMAtteo COvid-19 REgistry (SMACORE) cohort",
"author": "Biscarini",
"doi-asserted-by": "crossref",
"first-page": "1920",
"journal-title": "Nutr. Metab. Cardiovasc. Dis.",
"key": "ref_38",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1002/oby.22831",
"article-title": "High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation",
"author": "Simonnet",
"doi-asserted-by": "crossref",
"first-page": "1195",
"journal-title": "Obesity",
"key": "ref_39",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1002/oby.22971",
"article-title": "Visceral adiposity and high intramuscular fat deposition independently predict critical illness in patients with SARS-CoV-2",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "2040",
"journal-title": "Obesity",
"key": "ref_40",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1016/j.ejrad.2021.110031",
"article-title": "Association of body composition parameters measured on CT with risk of hospitalization in patients with Covid-19",
"author": "Chandarana",
"doi-asserted-by": "crossref",
"first-page": "110031",
"journal-title": "Eur. J. Radiol.",
"key": "ref_41",
"volume": "145",
"year": "2021"
},
{
"DOI": "10.3390/sports9090121",
"doi-asserted-by": "crossref",
"key": "ref_42",
"unstructured": "Jakobsson, J., Cotgreave, I., Furberg, M., Arnberg, N., and Svensson, M. (2021). Potential physiological and cellular mechanisms of exercise that decrease the risk of severe complications and mortality following SARS-CoV-2 infection. Sports, 9."
},
{
"DOI": "10.1001/jamanetworkopen.2023.9840",
"article-title": "Association of Physical Activity with SARS-CoV-2 Infection and Severe Clinical Outcomes Among Patients in South Korea",
"author": "Lim",
"doi-asserted-by": "crossref",
"first-page": "e239840",
"journal-title": "JAMA Netw. Open",
"key": "ref_43",
"volume": "6",
"year": "2023"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/12/12/4046"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Physical Activity Modifies the Severity of COVID-19 in Hospitalized Patients—Observational Study",
"type": "journal-article",
"volume": "12"
}
