Low levels of vitamin D were associated with coagulopathy among hospitalized coronavirus disease-19 (COVID-19) patients: A single-centered study in Indonesia
et al., Journal of Medical Biochemistry, doi:10.5937/jomb0-30228 , Feb 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
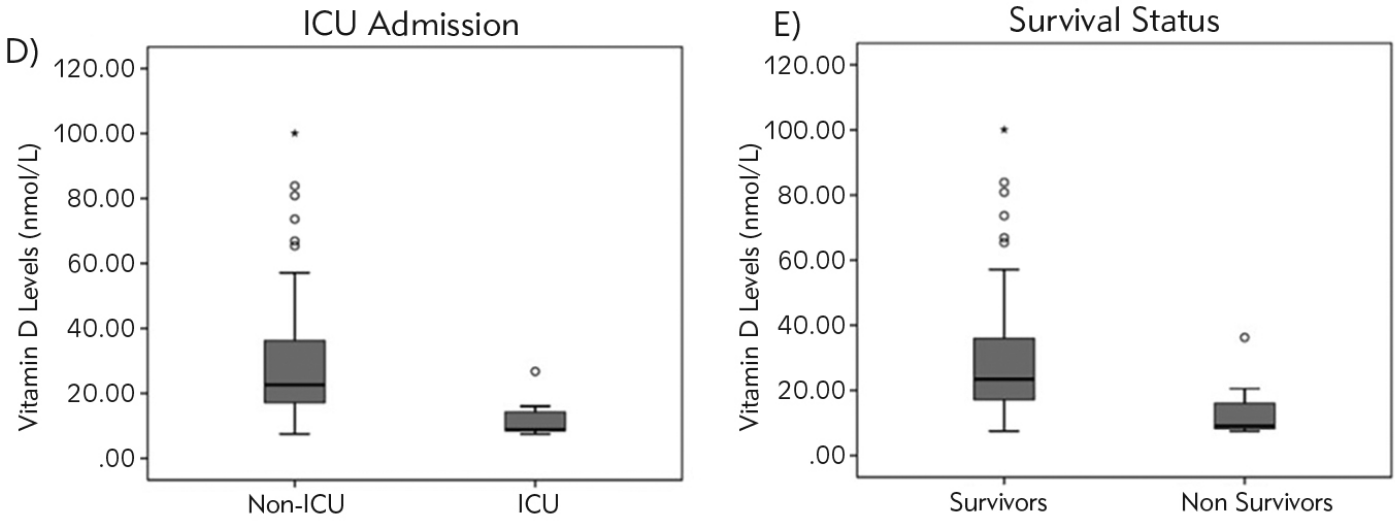
Retrospective 50 hospitalized PCR+ patients in Indonesia showing ICU admission, mortality, ISTH DIC (Disseminated Intravascular Coagulation) score ≥5, and increased D-dimer significantly associated with lower vitamin D levels.
This is the 46th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 91.5% lower, RR 0.09, p = 0.32, high D levels 0 of 8 (0.0%), low D levels 9 of 42 (21.4%), NNT 4.7, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), >49.92 nmol/L.
|
|
risk of ICU admission, 90.5% lower, RR 0.10, p = 0.32, high D levels 0 of 8 (0.0%), low D levels 8 of 42 (19.0%), NNT 5.2, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), >49.92 nmol/L.
|
|
risk of progression, 81.5% lower, OR 0.19, p = 0.04, high D levels 8, low D levels 42, inverted to make OR<1 favor high D levels, ISTH DIC≥5, >49.92 nmol/L, bivariate, RR approximated with OR.
|
|
risk of progression, 44.4% lower, OR 0.56, p = 0.03, high D levels 8, low D levels 42, inverted to make OR<1 favor high D levels, increased D-dimer >2 mg/L, >49.92 nmol/L, multivariate, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Susianti et al., 12 Feb 2021, retrospective, Indonesia, peer-reviewed, 8 authors.
Low levels of vitamin D were associated with coagulopathy among hospitalized coronavirus disease-19 (COVID-19) patients: A single-centered study in Indonesia
Journal of Medical Biochemistry, doi:10.5937/jomb0-30228
Background: This study was aimed to explore the association of vitamin D in the risk of coagulopathy in coronavirus disease-19 . Methods: Clinical and laboratory findings were obtained from 50 confirmed COVID-19 patients hospitalized in Saiful Anwar General Hospital, Malang, Indonesia, from September to November 2020. Thrombotic events during hospitalization were recorded, and the ISTH disseminated intravascular coagulation (DIC) score was used to classify overt DIC. Hypovitaminosis D was defined by serum vitamin D level <49.92 nmol/L. Results: Among 50 patients, 42 (84%) had hypovitaminosis D, and 6 (12%) developed thrombotic events. Vitamin D levels were lower in patients with thrombotic events (p=0.015), D-dimer >2 mg/L (p=0.006), ISTH DIC score 5 (p=0.020), admitted on ICU (p=0.002), and non-survivor groups (p=0.007). Multivariate analysis for the risk in increased D-dimer levels showed low vitamin D as the only significant risk factor with OR 1.8 (1.2-4.4), p=0.034. Low vitamin D also increased the risk for developing overt DIC with OR. 5.4 (1.0-30.2), p=0.039. Vitamin D level had negative correlations with ferritin (R=-0.316, p=0.044) and CRP (R=-0.530, p=0.000).
Kratak sadr`aj Uvod: Cilj ove studije je bio da istra`i povezanost vitamina D sa rizikom od koagulopatije kod koronavirusne bolesti 2019 (COVID-19). Metode: Klini~ki i laboratorijski nalazi dobijeni su od 50 potvr|enih pacijenata sa COVID-19 hospitalizovanih u op{toj bolnici Saiful Anvar u Malangu u Indoneziji, od septembra do novembra 2020. Zabele`eni su tromboti~ni doga|aji tokom hospitalizacije, a rezultati ISTH diseminovane intravaskularne koagulacije (DIC) kori{}eni su za klasifikaciju o~igledne DIC. Hipovitaminoza D je definisana nivoom vitamina D u serumu <49,92 nmol/L. Rezultati: Od 50 pacijenata, 42 (84%) je imalo hipovitaminozu D, a 6 (12%) je razvilo tromboti~ke doga|aje. Nivoi vitamina D su bili ni`i kod pacijenata sa tromboti~kim doga|ajima (p=0,015), D-dimerom >2 mg/L (p=0,006), ISTH DIC rezultatima 5 (p=0,020), primljenih na intenzivnu negu (p=0,002), i grupa koje nisu pre`ivele (p=0,007). Multivarijantna analiza rizika za pove}ane nivoe D-dimera pokazala je nizak nivo vitamina D kao jedini zna~ajni faktor rizika sa OR 1,8 (1,2-4,4), p=0,034. Nizak nivo vitamina D je tako|e pove}ao rizik od razvoja o~iglednog DIC-a sa OR 5,4 (1,0-30,2), p=0,039. Nivo
Conflict of interest statement All the authors declare that they have no conflict of interest in this work.
References
Abou-Ismail, Diamond, Kapoor, Arafah, Nayak, The hypercoagulable state in COVID-19: Incidence, pathophysiology, and management, Thromb Res
Ahnach, Zbiri, Nejjari, Ousti, Elkettani, Creactive protein as an early predictor of COVID-19 severity, J Med Biochem
Aihara, Azuma, Akaike, Ikeda, Yamashita et al., Disruption of nuclear vitamin D receptor gene causes enhanced thrombogenicity in mice, J Biol Chem
Bouillon, Carmeliet, Vitamin D insufficiency: Definition, diagnosis and management, Best Pract Res Clin Endocrinol Metab
Carpagnano, Lecce, Quaranta, Zito, Buonamico et al., Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest
Connors, Levy, COVID-19 and its implications for thrombosis and anticoagulation, Blood
Dao, Patel, Overton, Rhame, Pals et al., Low vitamin D among HIV-infected adults: prevalence of and risk factors for low vitamin D Levels in a cohort of HIV-infected adults and comparison to prevalence among adults in the US general population, Clin Infect Dis
Entezari-Maleki, Talasaz, Salarifar, Hadjibabaie, Javadi et al., Plasma Vitamin D Status and Its Correlation with Risk Factors of Thrombosis, P-selectin and hs-CRP Level in Patients with Venous Thromboembolism; the First Study of Iranian Population, Iran J Pharm Res
Farnik, Bojunga, Berger, Allwinn, Waidmann et al., Low vitamin D serum concentration is associated with high levels of hepatitis B virus replication in chronically infected patients, Hepatology
Fb, Toh, Hoots, Wada, Levi, Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation, Thromb Haemost
Helms, Tacquard, Severac, Leonard-Lorant, Ohana et al., High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study, Intensive Care Med
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Kabeerdoss, Danda, Understanding immunopathological fallout of human coronavirus infections including COVID-19: Will they cross the path of rheumatologists?, Int J Rheum Dis
Khademvatani, Seyyed-Mohammadzad, Akbari, Rezaei, Eskandari et al., The relationship between vitamin D status and idiopathic lowerextremity deep vein thrombosis, Int J Gen Med
Klok, Kruip, Van Der Meer, Arbous, Gommers et al., Incidence of thrombotic complications in critically ill ICU patients with COVID-19, Thromb Res
Manion, Hullsiek, Wilson, Rhame, Kojic et al., Vitamin D deficiency is associated with IL-6 levels and monocyte activation in HIV-infected persons, PLoS One
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression, Lancet
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J
Milinkovi}, Sari}, Jovi~i}, Mirkovi}, Ai} et al., Lipid status association with 25-hydroxy vitamin D: Cross sectional study of end stage renal disease patients, J Med Biochem
Mohammad, Mishra, Ashraf, Emerging Role of Vitamin D and its Associated Molecules in Pathways Related to Pathogenesis of Thrombosis, Biomolecules
Ortega-Paz, Capodanno, Montalescot, Angiolillo, COVID-19 Associated Thrombosis and Coagulopathy: Review of the Pathophysiology and Implications for Antithrombotic Management, J Am Heart Assoc
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients
Sultan, Twito, Tohami, Ramati, Neumark et al., Vitamin D diminishes the high platelet aggregation of type 2 diabetes mellitus patients, Platelets
Terpos, Ntanasis-Stathopoulos, Elalamy, Kastritis, Sergentanis et al., Hematological findings and complications of COVID-19, Am J Hematol
Thachil, Tang, Gando, Falanga, Cattaneo et al., ISTH interim guidance on recognition and management of coagulopathy in COVID-19, J Thromb Haemost
Wang, Hu, Hu, Zhu, Liu et al., Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China, JAMA
Xiong, Gong, Liu, Xiang, Tan, Loss of vitamin D receptor in chronic kidney disease: a potential mechanism linking inflammation to epithelial-to-mesenchymal transition, Am J Physiol Renal Physiol
Yao, Cao, Wang, Shi, Liu et al., Ddimer as a biomarker for disease severity and mortality in COVID-19 patients: a case control study, J Intensive Care
Zhang, Xiao, Zhang, Xia, Cao et al., Coagulopathy and Anti-phospholipid Antibodies in Patients with Covid-19, N Engl J Med
DOI record:
{
"DOI": "10.5937/jomb0-30228",
"ISSN": [
"1452-8258",
"1452-8266"
],
"URL": "http://dx.doi.org/10.5937/jomb0-30228",
"abstract": "<jats:p>Background: This study was aimed to explore the association of vitamin D in the risk of coagulopathy in coronavirus disease-19 (COVID-19). Methods: Clinical and laboratory findings were obtained from 50 confirmed COVID-19 patients hospitalized in Saiful Anwar General Hospital, Malang, Indonesia, from September to November 2020. Thrombotic events during hospitalization were recorded, and the ISTH disseminated intravascular coagulation (DIC) score was used to classify overt DIC. Hypovitaminosis D was defined by serum vitamin D level <49.92 nmol/L. Results: Among 50 patients, 42 (84%) had hypovitaminosis D, and 6 (12%) developed thrombotic events. Vitamin D levels were lower in patients with thrombotic events (p=0.015), D-dimer >2 mg/L (p=0.006), ISTH DIC score 5 (p=0.020), admitted on ICU (p=0.002), and non-survivor groups (p=0.007). Multivariate analysis for the risk in increased D-dimer levels showed low vitamin D as the only significant risk factor with OR 1.8 (1.2-4.4), p=0.034. Low vitamin D also increased the risk for developing overt DIC with OR. 5.4 (1.0-30.2), p=0.039. Vitamin D level had negative correlations with ferritin (R=-0.316, p=0.044) and CRP (R=-0.530, p=0.000). Conclusions: In conclusion, a low level of vitamin D was found in most hospitalized COVID-19 patients and might be associated with the development of coagulopathy.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Susianti",
"given": "Hani",
"sequence": "first"
},
{
"affiliation": [],
"family": "Wahono",
"given": "Cesarius",
"sequence": "additional",
"suffix": "Singgih"
},
{
"affiliation": [],
"family": "Rahman",
"given": "Perdana",
"sequence": "additional",
"suffix": "Aditya"
},
{
"affiliation": [],
"family": "Pratama",
"given": "Mirza",
"sequence": "additional",
"suffix": "Zaka"
},
{
"affiliation": [],
"family": "Wulanda",
"given": "Indah",
"sequence": "additional",
"suffix": "Adhita"
},
{
"affiliation": [],
"family": "Hartanti",
"given": "Khoirunisah",
"sequence": "additional",
"suffix": "Dwi"
},
{
"affiliation": [],
"family": "Dewi",
"given": "Elvira",
"sequence": "additional",
"suffix": "Sari"
},
{
"affiliation": [],
"family": "Handono",
"given": "Kusworini",
"sequence": "additional"
}
],
"container-title": "Journal of Medical Biochemistry",
"container-title-short": "J Med Biochemistry",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
2,
12
]
],
"date-time": "2021-02-12T13:57:45Z",
"timestamp": 1613138265000
},
"deposited": {
"date-parts": [
[
2021,
9,
3
]
],
"date-time": "2021-09-03T21:26:15Z",
"timestamp": 1630704375000
},
"indexed": {
"date-parts": [
[
2024,
2,
15
]
],
"date-time": "2024-02-15T08:44:34Z",
"timestamp": 1707986674706
},
"is-referenced-by-count": 7,
"issue": "4",
"issued": {
"date-parts": [
[
2021
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2021
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/BY/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
}
],
"link": [
{
"URL": "https://aseestant.ceon.rs/index.php/jomb/article/download/30228/17082",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://scindeks-clanci.ceon.rs/data/pdf/1452-8258/2021/1452-82582104341S.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "3964",
"original-title": [
"Niski nivoi vitamina D povezani su sa koagulopatijom kod hospitalizovanih pacijenata sa koronavirusom (COVID-19) - jednocentrična studija u Indoneziji"
],
"page": "341-350",
"prefix": "10.5937",
"published": {
"date-parts": [
[
2021
]
]
},
"published-print": {
"date-parts": [
[
2021
]
]
},
"publisher": "Centre for Evaluation in Education and Science (CEON/CEES)",
"reference": [
{
"key": "ref1",
"unstructured": "WHO Coronavirus Disease (COVID-19) Dashboard. https: //covid19.who.int/ (accessed 29 November 2020);"
},
{
"DOI": "10.1001/jama.2020.1585",
"doi-asserted-by": "crossref",
"key": "ref2",
"unstructured": "Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 March 17; 323(11): 1061-9;"
},
{
"DOI": "10.1182/blood.2020006000",
"doi-asserted-by": "crossref",
"key": "ref3",
"unstructured": "Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020 June 4; 135(23): 2033-40;"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "crossref",
"key": "ref4",
"unstructured": "Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020 Feb 15, 395(10223): 497-506;"
},
{
"DOI": "10.1186/s40560-020-00466-z",
"doi-asserted-by": "crossref",
"key": "ref5",
"unstructured": "Yao Y, Cao J, Wang Q, Shi Q, Liu K, Luo Z, et al. Ddimer as a biomarker for disease severity and mortality in COVID-19 patients: a case control study. J Intensive Care 2020 July 10; 8: 49;"
},
{
"DOI": "10.1111/jth.14810",
"doi-asserted-by": "crossref",
"key": "ref6",
"unstructured": "Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost 2020 May; 18(5): 1023-6;"
},
{
"key": "ref7",
"unstructured": "Ortega-Paz L, Capodanno D, Montalescot G, Angiolillo DJ. COVID-19 Associated Thrombosis and Coagulo - pathy: Review of the Pathophysiology and Implications for Antithrombotic Management. J Am Heart Assoc 2020 November 24: e019650;"
},
{
"DOI": "10.1016/j.thromres.2020.06.029",
"doi-asserted-by": "crossref",
"key": "ref8",
"unstructured": "Abou-Ismail MY, Diamond A, Kapoor S, Arafah Y, Nayak L. The hypercoagulable state in COVID-19: Incidence, pathophysiology, and management. Thromb Res 2020 Oct; 194: 101-15;"
},
{
"DOI": "10.1056/NEJMc2007575",
"doi-asserted-by": "crossref",
"key": "ref9",
"unstructured": "Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, et al. Coagulopathy and Anti-phospholipid Antibodies in Patients with Covid-19. N Engl J Med 2020 April 23; 382(17): e38;"
},
{
"DOI": "10.1111/1756-185X.13909",
"doi-asserted-by": "crossref",
"key": "ref10",
"unstructured": "Kabeerdoss J, Danda D. Understanding immunopathological fallout of human coronavirus infections including COVID-19: Will they cross the path of rheumatologists? Int J Rheum Dis 2020 Aug; 23(8): 998-1008;"
},
{
"DOI": "10.3390/biom9110649",
"doi-asserted-by": "crossref",
"key": "ref11",
"unstructured": "Mohammad S, Mishra A, Ashraf MZ. Emerging Role of Vitamin D and its Associated Molecules in Pathways Related to Pathogenesis of Thrombosis. Biomolecules 2019 Oct 24; 9(11): 649;"
},
{
"DOI": "10.1074/jbc.M404865200",
"doi-asserted-by": "crossref",
"key": "ref12",
"unstructured": "Aihara K, Azuma H, Akaike M, Ikeda Y, Yamashita M, Sudo T, et al. Disruption of nuclear vitamin D receptor gene causes enhanced thrombogenicity in mice. J Biol Chem 2004 August 20; 279(34): 35798-802;"
},
{
"DOI": "10.2147/IJGM.S64812",
"doi-asserted-by": "crossref",
"key": "ref13",
"unstructured": "Khademvatani K, Seyyed-Mohammadzad MH, Akbari M, Rezaei Y, Eskandari R, Rostamzadeh A. The relationship between vitamin D status and idiopathic lowerextremity deep vein thrombosis. Int J Gen Med 2014 June 19; 7: 303-9;"
},
{
"DOI": "10.2478/jomb-2019-0032",
"doi-asserted-by": "crossref",
"key": "ref14",
"unstructured": "Milinković N, Sarić M, Jovičić S, Mirković D,Lèaić V, Ignjatović S. Lipid status association with 25-hydroxy vitamin D: Cross sectional study of end stage renal disease patients. J Med Biochem 2020; 39(4): 309 -17;"
},
{
"DOI": "10.1101/2020.07.01.20144329",
"doi-asserted-by": "crossref",
"key": "ref15",
"unstructured": "Merzon E, Tworowski D, Gorohovski A, Vinker S, Golan Cohen A, Green I, Frenkel-Morgenstern M. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J 2020 July 23: 10.1111/febs.15495;"
},
{
"key": "ref16",
"unstructured": "World Health Organization. WHO Covid-19 case definition. Published 7 August 2020. Accessed 1 September 2020. https: //www.who.int/publications/i/item/ WHO-2019-nCoV-Sur veillance_Case_Definition-2020.1;"
},
{
"DOI": "10.1016/j.beem.2018.09.014",
"doi-asserted-by": "crossref",
"key": "ref17",
"unstructured": "Bouillon R, Carmeliet G. Vitamin D insufficiency: Definition, diagnosis and management. Best Pract Res Clin Endocrinol Metab 2018 Oct; 32(5): 669-84;"
},
{
"DOI": "10.1055/s-0037-1616068",
"doi-asserted-by": "crossref",
"key": "ref18",
"unstructured": "FB Jr, Toh CH, Hoots WK, Wada H, Levi M; Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost 2001 Nov; 86(5): 1327-30;"
},
{
"DOI": "10.1016/j.thromres.2020.04.013",
"doi-asserted-by": "crossref",
"key": "ref19",
"unstructured": "Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020 Jul; 191: 145-7;"
},
{
"DOI": "10.1007/s00134-020-06062-x",
"doi-asserted-by": "crossref",
"key": "ref20",
"unstructured": "Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 2020 Jun; 46(6): 1089-98;"
},
{
"DOI": "10.1093/cid/ciq158",
"doi-asserted-by": "crossref",
"key": "ref21",
"unstructured": "Dao CN, Patel P, Overton ET, Rhame F, Pals SL, Johnson C, et al. Low vitamin D among HIV-infected adults: prevalence of and risk factors for low vitamin D Levels in a cohort of HIV-infected adults and comparison to prevalence among adults in the US general population. Clin Infect Dis 2011 February 1; 52(3): 396-405;"
},
{
"DOI": "10.1002/hep.26488",
"doi-asserted-by": "crossref",
"key": "ref22",
"unstructured": "Farnik H, Bojunga J, Berger A, Allwinn R, Waidmann O, Kronenberger B, et al. Low vitamin D serum concentration is associated with high levels of hepatitis B virus replication in chronically infected patients. Hepatology 2013 Oct; 58(4): 1270-6;"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "crossref",
"key": "ref23",
"unstructured": "Radujkovic A, Hippchen T, Tiwari-Heckler S, Dreher S, Boxberger M, Merle U. Vitamin D Deficiency and Outcome of COVID-19 Patients. Nutrients 2020 Sep 10; 12(9): 2757;"
},
{
"DOI": "10.21203/rs.3.rs-41173/v1",
"doi-asserted-by": "crossref",
"key": "ref24",
"unstructured": "Carpagnano GE, Di Lecce V, Quaranta VN, Zito A, Buonamico E, Capozza E, et al. Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19. J Endocrinol Invest 2020 August 9: 1-7;"
},
{
"key": "ref25",
"unstructured": "Entezari-Maleki T, Hajhossein Talasaz A, Salarifar M, Hadjibabaie M, Javadi MR, Bozorgi A, et al. Plasma Vitamin D Status and Its Correlation with Risk Factors of Thrombosis, P-selectin and hs-CRP Level in Patients with Venous Thromboembolism; the First Study of Iranian Population. Iran J Pharm Res 2014 Winter, 13(1): 319-27;"
},
{
"DOI": "10.1080/09537104.2017.1386298",
"doi-asserted-by": "crossref",
"key": "ref26",
"unstructured": "Sultan M, Twito O, Tohami T, Ramati E, Neumark E, Rashid G. Vitamin D diminishes the high platelet aggregation of type 2 diabetes mellitus patients. Platelets. 2019; 30(1): 120-5;"
},
{
"DOI": "10.5937/jomb0-27554",
"doi-asserted-by": "crossref",
"key": "ref27",
"unstructured": "Ahnach M, Zbiri S, Nejjari S, Ousti F, Elkettani C. Creactive protein as an early predictor of COVID-19 severity. J Med Biochem 2020; 39(4): 500-7;"
},
{
"DOI": "10.1002/ajh.25829",
"doi-asserted-by": "crossref",
"key": "ref28",
"unstructured": "Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, Psaltopoulou T, Gerotziafas G, Dimopoulos MA. Hematological findings and complications of COVID-19. Am J Hematol 2020 Jul, 95(7): 834-47;"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"doi-asserted-by": "crossref",
"key": "ref29",
"unstructured": "Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020 March 28, 395(10229): 1033-4;"
},
{
"DOI": "10.1152/ajprenal.00151.2012",
"doi-asserted-by": "crossref",
"key": "ref30",
"unstructured": "Xiong M, Gong J, Liu Y, Xiang R, Tan X. Loss of vitamin D receptor in chronic kidney disease: a potential mechanism linking inflammation to epithelial-to-mesenchymal transition. Am J Physiol Renal Physiol 2012 Oct; 303(7): F1107-15;"
},
{
"DOI": "10.1371/journal.pone.0175517",
"doi-asserted-by": "crossref",
"key": "ref31",
"unstructured": "Manion M, Hullsiek KH, Wilson EMP, Rhame F, Kojic E, Gibson D, et al. Vitamin D deficiency is associated with IL-6 levels and monocyte activation in HIV-infected persons. PLoS One 2017 May 2; 12(5): e0175517;"
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "https://scindeks.ceon.rs/Article.aspx?artid=1452-82582104341S"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Biochemistry (medical)",
"Clinical Biochemistry"
],
"subtitle": [],
"title": "Low levels of vitamin D were associated with coagulopathy among hospitalized coronavirus disease-19 (COVID-19) patients: A single-centered study in Indonesia",
"type": "journal-article",
"volume": "40"
}
