Association of vitamin D level and severity of COVID-19 disease
et al., Journal of Southeast Asian Medical Research, doi:10.55374/jseamed.v8.202, Jun 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 97 hospitalized COVID-19 patients in Thailand showing vitamin D deficiency associated with higher risk of severe illness.
This is the 198th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
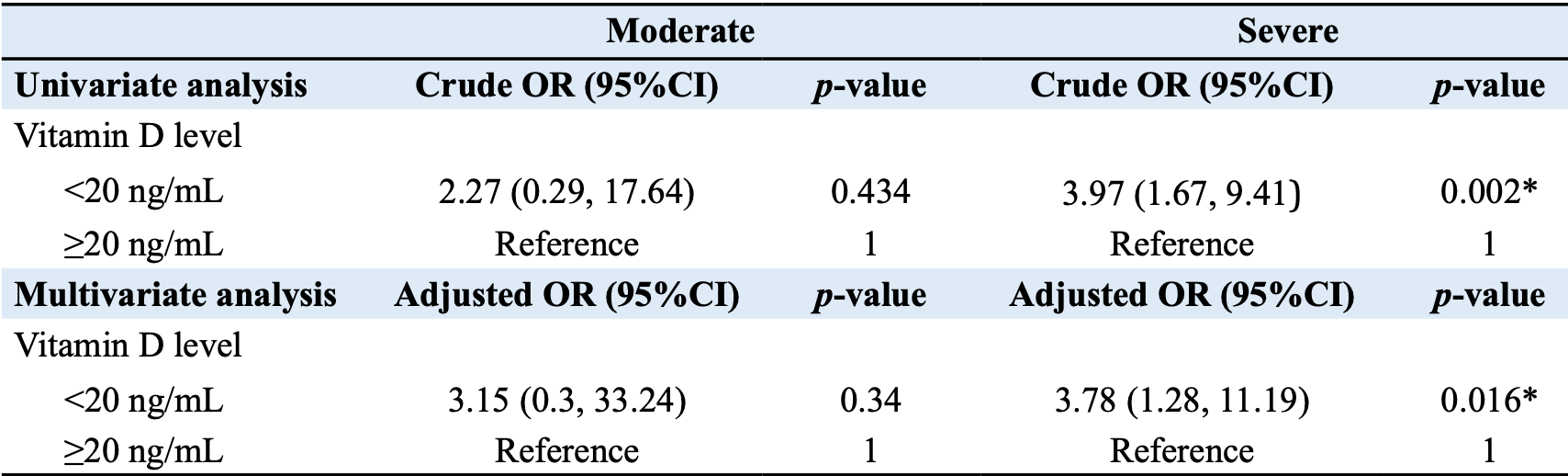
risk of severe case, 51.2% lower, RR 0.49, p = 0.02, high D levels (≥20ng/mL) 16 of 52 (30.8%), low D levels (<20ng/mL) 28 of 45 (62.2%), NNT 3.2, adjusted per study, inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, multivariable.
|
|
moderate case, 67.3% lower, RR 0.33, p = 0.34, high D levels (≥20ng/mL) 2 of 52 (3.8%), low D levels (<20ng/mL) 2 of 45 (4.4%), adjusted per study, inverted to make RR<1 favor high D levels (≥20ng/mL), odds ratio converted to relative risk, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Singhsakul et al., 9 Jun 2024, retrospective, Thailand, peer-reviewed, mean age 50.8, 6 authors, study period 1 September, 2021 - 30 November, 2021.
Contact: sasiwimon.tra@gmail.com.
ASSOCIATION OF VITAMIN D LEVEL AND SEVERITY OF COVID-19 DISEASE
Journal of Southeast Asian Medical Research, doi:10.55374/jseamed.v8.202
Background: Studies indicate that vitamin D can lower the incidence of viral respiratory infections and is necessary for the human immune system to function properly. Vitamin D deficiency may be a risk factor for the severity of COVID-19, including mortality, hospitalization, and length of hospital stay. Objectives: This study aimed to investigate the association between vitamin D levels and the severity of COVID-19 disease. Methods: The participants were COVID-19 patients aged 18 years or older who tested positive for the virus on Real-Time PCR tests, treated as inpatients at Banphaeo General Hospital between September 1 and November 30, 2021. For each patient, baseline characteristics, including sex, weight, height, and underlying diseases, were collected. Three categories were used to categorize COVID-19 disease: mild, moderate, and severe. At the beginning of the study, blood tests were performed on each patient to determine their 25-hydroxyvitamin D levels. Results: Of 97 patients, 64 were male (66%), with a mean age of 50.8±17.7 years. The mean vitamin D level was 27.8±9.6 ng/mL, with 45 (46.4%) showing vitamin D deficiency and 39 (40.2%) indicating vitamin D insufficiency. Among COVID-19 patients with vitamin D deficiency, 28 (63.6%) were classified as severe, compared to only 16 severe cases (36.4%) among those without vitamin D deficiency, demonstrating statistically significant differences (p=0.006). Patients with vitamin D deficiency had a 3.97 times higher risk of experiencing severity (95% CI: 1.67, 9.41, p=0.002) than those without a vitamin D deficit. After adjusting for variable factors, results indicated that patients with vitamin D deficiency had a 3.78-fold increased risk of getting severe illness than those without deficiency (95% CI: 1.28, 11.19, p=0.016). Conclusion: These findings suggested that vitamin D deficiency was associated with the severity of COVID-19.
Conflict of interest The authors declare they have no conflict of interest.
References
Adami, Rossini, Bogliolo, Cantatore, Varenna et al., An exploratory study on the role of vitamin D supplementation in improving pain and disease activity in rheumatoid arthritis, Mod Rheumatol
Annweiler, Hanotte, De L'eprevier, Sabatier, Lafaie et al., Vitamin D and survival in COVID-19 patients: A quasi-experimental study, J Steroid Biochem Mol Biol
Aranow, Journal of investigative medicine : the official publication of the, American Federation for Clinical Research
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy, BMC Infect Dis
Chailurkit, Aekplakorn, Ongphiphadhanakul, Regional variation and determinants of vitamin D status in sunshine-abundant Thailand, BMC Public Health
D'avolio, Avataneo, Manca, Cusato, Nicolò et al., 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients
Dimitrov, White, Species-specific regulation of innate immunity by vitamin D signaling, J Steroid Biochem Mol Biol
Hanff, Harhay, Brown, Cohen, Mohareb, Is there an association between COVID-19 mortality and the renin-angiotensin system? A call for epidemiologic investigations, Clin Infect Dis
Hansdottir, Monick, Hinde, Lovan, Look et al., Respiratory epithelial cells convert inactive vitamin D to its active form: Potential effects on host defense, J Immunol
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline, J Clin Endocrinol Metab
Hossein-Nezhad, Holick, Vitamin D for health: A global perspective, Mayo Clin Proc
Jiang, Chou, Chen, Cathelicidin attenuates hyperoxia-induced lung injury by inhibiting oxidative stress in newborn rats, Free Radic Biol Med
Karatekin, Kaya, Salihoğlu, Balci, Nuhoğlu, Association of subclinical vitamin D deficiency in newborns with acute lower respiratory infection and their mothers, Eur J Clin Nutr
Martineau, Jolliffe, Greenberg, Aloia, Bergman et al., Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis, Health Technol Assess
Mercola, Grant, Wagner, Evidence regarding vitamin D and risk of COVID-19 and its severity, Nutrients
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial, JAMA
Nimitphong, Holick, Vitamin D status and sun exposure in southeast Asia, Dermatoendocrinol
Palacios, Gonzalez, Is vitamin D deficiency a major global public health problem?, J Steroid Biochem Mol Biol
Rhodes, Subramanian, Laird, Griffin, Kenny, Perspective: Vitamin D deficiency and COVID-19 severity -plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, J Intern Med
Sassi, Tamone, Amelio, Vitamin D: Nutrient, hormone, and immunomodulator, Nutrients
Shah, Varna, Sharma, Mavalankar, Does vitamin D supplementation reduce COVID-19 severity?: a systematic review, QJM
Siwamogsatham, Ongphiphadhanakul, Tangpricha, Vitamin D deficiency in Thailand, J Clin Transl Endocrinol
Teshome, Adane, Girma, Mekonnen, The impact of vitamin D level on COVID-19 infection: Systematic review and meta-analysis, Front Public Health
Wang, Joshi, Jackson, Christensen, Nayfeh, Association of vitamin D deficiency with COVID-19 infection severity: Systematic review and metaanalysis, Clin Endocrinol (Oxf)
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, transmission, diagnosis, and treatment of Coronavirus disease 2019 (COVID-19): A review, JAMA
Wolff, Nee, Hickey, Marschollek, Risk factors for Covid-19 severity and fatality: a structured literature review, Infection
Ye, Tang, Liao, Shaw, Deng et al., Does serum vitamin D level affect COVID-19 infection and its severity? -A case-control study, J Am Coll Nutr
DOI record:
{
"DOI": "10.55374/jseamed.v8.202",
"ISSN": [
"2697-5424",
"2586-8241"
],
"URL": "http://dx.doi.org/10.55374/jseamed.v8.202",
"abstract": "<jats:p>Background: Studies indicate that vitamin D can lower the incidence of viral respiratory infections and is necessary for the human immune system to function properly. Vitamin D deficiency may be a risk factor for the severity of COVID-19, including mortality, hospitalization, and length of hospital stay.\nObjectives: This study aimed to investigate the association between vitamin D levels and the severity of COVID-19 disease.\nMethods: The participants were COVID-19 patients aged 18 years or older who tested positive for the virus on Real-Time PCR tests, treated as inpatients at Banphaeo General Hospital between September 1 and November 30, 2021. For each patient, baseline characteristics, including sex, weight, height, and underlying diseases, were collected. Three categories were used to categorize COVID-19 disease: mild, moderate, and severe. At the beginning of the study, blood tests were performed on each patient to determine their 25-hydroxyvitamin D levels.\nResults: Of 97 patients, 64 were male (66%), with a mean age of 50.8±17.7 years. The mean vitamin D level was 27.8±9.6 ng/mL, with 45 (46.4%) showing vitamin D deficiency and 39 (40.2%) indicating vitamin D insufficiency. Among COVID-19 patients with vitamin D deficiency, 28 (63.6%) were classified as severe, compared to only 16 severe cases (36.4%) among those without vitamin D deficiency, demonstrating statistically significant differences (p=0.006). Patients with vitamin D deficiency had a 3.97 times higher risk of experiencing severity (95% CI: 1.67, 9.41, p=0.002) than those without a vitamin D deficit. After adjusting for variable factors, results indicated that patients with vitamin D deficiency had a 3.78-fold increased risk of getting severe illness than those without deficiency (95% CI: 1.28, 11.19, p=0.016). Conclusion: These findings suggested that vitamin D deficiency was associated with the severity of COVID-19.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Singhsakul",
"given": "Amol",
"sequence": "first"
},
{
"affiliation": [],
"family": "Satirapoj",
"given": "Bancha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nimitphuwadon",
"given": "Sirinthip",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rapeepattana",
"given": "Sirate",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Benjamanukul",
"given": "Saovanee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Traiyan",
"given": "Sasiwimon",
"sequence": "additional"
}
],
"container-title": "Journal of Southeast Asian Medical Research",
"container-title-short": "J Southeast Asian Med Res",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
6,
9
]
],
"date-time": "2024-06-09T02:57:09Z",
"timestamp": 1717901829000
},
"deposited": {
"date-parts": [
[
2024,
6,
9
]
],
"date-time": "2024-06-09T02:57:26Z",
"timestamp": 1717901846000
},
"indexed": {
"date-parts": [
[
2024,
6,
9
]
],
"date-time": "2024-06-09T03:10:45Z",
"timestamp": 1717902645165
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
6,
9
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
6,
9
]
],
"date-time": "2024-06-09T00:00:00Z",
"timestamp": 1717891200000
}
}
],
"link": [
{
"URL": "https://jseamed.org/index.php/jseamed/article/download/202/133",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://jseamed.org/index.php/jseamed/article/download/202/133",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "33699",
"original-title": [],
"page": "e0202",
"prefix": "10.55374",
"published": {
"date-parts": [
[
2024,
6,
9
]
]
},
"published-online": {
"date-parts": [
[
2024,
6,
9
]
]
},
"publisher": "Phramongkutklao Hospital Foundation",
"reference": [
{
"DOI": "10.1001/jama.2020.12839",
"doi-asserted-by": "crossref",
"key": "4575",
"unstructured": "Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of Coronavirus disease 2019 (COVID-19): A review. JAMA 2020; 324: 782."
},
{
"DOI": "10.1007/s15010-020-01509-1",
"doi-asserted-by": "crossref",
"key": "4576",
"unstructured": "Wolff D, Nee S, Hickey NS, Marschollek M. Risk factors for Covid-19 severity and fatality: a structured literature review. Infection 2021; 49: 15–28."
},
{
"DOI": "10.3390/nu12051359",
"doi-asserted-by": "crossref",
"key": "4577",
"unstructured": "D’Avolio A, Avataneo V, Manca A, Cusato J, De Nicolò A, Lucchini R, et al. 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2. Nutrients 2020; 12: 1359."
},
{
"DOI": "10.1111/cen.14540",
"doi-asserted-by": "crossref",
"key": "4578",
"unstructured": "Wang Z, Joshi A, Leopold K, Jackson S, Christensen S, Nayfeh T, et al. Association of vitamin D deficiency with COVID‐19 infection severity: Systematic review and meta‐ analysis. Clin Endocrinol (Oxf) 2022; 96: 281-7."
},
{
"DOI": "10.1038/sj.ejcn.1602960",
"doi-asserted-by": "crossref",
"key": "4579",
"unstructured": "Karatekin G, Kaya A, Salihoğlu Ö, Balci H, Nuhoğlu A. Association of subclinical vitamin D deficiency in newborns with acute lower respiratory infection and their mothers. Eur J Clin Nutr 2009; 63: 473–7."
},
{
"DOI": "10.1016/j.jsbmb.2015.09.016",
"doi-asserted-by": "crossref",
"key": "4580",
"unstructured": "Dimitrov V, White JH. Species-specific regulation of innate immunity by vitamin D signaling. J Steroid Biochem Mol Biol 2016; 164: 246–53."
},
{
"DOI": "10.3390/nu10111656",
"doi-asserted-by": "crossref",
"key": "4581",
"unstructured": "Sassi F, Tamone C, D’Amelio P. Vitamin D: Nutrient, hormone, and immunomodulator. Nutrients 2018; 10: 1656."
},
{
"DOI": "10.3310/hta23020",
"doi-asserted-by": "crossref",
"key": "4582",
"unstructured": "Martineau AR, Jolliffe DA, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol Assess 2019; 23: 1–44."
},
{
"key": "4583",
"unstructured": "SACN. Update of rapid review: Vitamin D and acute respiratory tract infections. Accessed November11 2022. https://assetspublishingservicegovuk/government/uploads/system/uploads/attachment_data/file/945179/SACN_December2020_VitaminD_AcuteRespiratoryTractInfectionspdf."
},
{
"DOI": "10.3390/nu12113361",
"doi-asserted-by": "crossref",
"key": "4584",
"unstructured": "Mercola J, Grant WB, Wagner CL. Evidence regarding vitamin D and risk of COVID-19 and its severity. Nutrients 2020; 12: 3361."
},
{
"DOI": "10.3389/fpubh.2021.624559",
"doi-asserted-by": "crossref",
"key": "4585",
"unstructured": "Teshome A, Adane A, Girma B, Mekonnen ZA. The impact of vitamin D level on COVID-19 infection: Systematic review and meta-analysis. Front Public Health 2021; 9: 624559."
},
{
"DOI": "10.1093/qjmed/hcac040",
"doi-asserted-by": "crossref",
"key": "4586",
"unstructured": "Shah K, Varna VP, Sharma U, Mavalankar D. Does vitamin D supplementation reduce COVID-19 severity?: a systematic review. QJM 2022; 115: 665–72."
},
{
"DOI": "10.1080/07315724.2020.1826005",
"doi-asserted-by": "crossref",
"key": "4587",
"unstructured": "Ye K, Tang F, Liao X, Shaw BA, Deng M, Huang G, et al. Does serum vitamin D level affect COVID-19 infection and its severity? -A case-control study. J Am Coll Nutr 2021; 40: 724–31."
},
{
"DOI": "10.1016/j.jcte.2014.10.004",
"doi-asserted-by": "crossref",
"key": "4588",
"unstructured": "Siwamogsatham O, Ongphiphadhanakul B, Tangpricha V. Vitamin D deficiency in Thailand. J Clin Transl Endocrinol 2015; 2: 48–9."
},
{
"key": "4589",
"unstructured": "COVID-19 Treatment Guidelines. National Institutes of Health (US). 2019; In: Coronavirus Disease 2019 (COVID-19)"
},
{
"DOI": "10.1210/jc.2011-0385",
"doi-asserted-by": "crossref",
"key": "4590",
"unstructured": "Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab 2011; 96: 1911–30."
},
{
"DOI": "10.1016/j.mayocp.2013.05.011",
"doi-asserted-by": "crossref",
"key": "4591",
"unstructured": "Hossein-nezhad A, Holick MF. Vitamin D for health: A global perspective. Mayo Clin Proc 2013; 88: 720–55."
},
{
"DOI": "10.1186/s12879-021-06281-7",
"doi-asserted-by": "crossref",
"key": "4592",
"unstructured": "Campi I, Gennari L, Merlotti D, Mingiano C, Frosali A, Giovanelli L, et al. Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy. BMC Infect Dis 2021; 21: 566."
},
{
"DOI": "10.1016/j.jsbmb.2013.11.003",
"doi-asserted-by": "crossref",
"key": "4593",
"unstructured": "Palacios C, Gonzalez L. Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol 2014;n144: 138–45."
},
{
"DOI": "10.1186/1471-2458-11-853",
"doi-asserted-by": "crossref",
"key": "4594",
"unstructured": "Chailurkit L-O, Aekplakorn W, Ongphiphadhanakul B. Regional variation and determinants of vitamin D status in sunshine-abundant Thailand. BMC Public Health 2011; 11: 853."
},
{
"DOI": "10.1080/14397595.2018.1532622",
"doi-asserted-by": "crossref",
"key": "4595",
"unstructured": "Adami G, Rossini M, Bogliolo L, Cantatore FP, Varenna M, Malavolta N, et al. An exploratory study on the role of vitamin D supplementation in improving pain and disease activity in rheumatoid arthritis. Mod Rheumatol 2019; 29: 1059–62."
},
{
"DOI": "10.1111/joim.13149",
"doi-asserted-by": "crossref",
"key": "4596",
"unstructured": "Rhodes JM, Subramanian S, Laird E, Griffin G, Kenny RA. Perspective: Vitamin D deficiency and COVID‐19 severity – plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis. J Intern Med 2021; 289: 97–115."
},
{
"DOI": "10.1016/j.jsbmb.2020.105771",
"doi-asserted-by": "crossref",
"key": "4597",
"unstructured": "Annweiler C, Hanotte B, Grandin de l’Eprevier C, Sabatier J-M, Lafaie L, Célarier T. Vitamin D and survival in COVID-19 patients: A quasi-experimental study. J Steroid Biochem Mol Biol 2020; 204: 105771."
},
{
"DOI": "10.4161/derm.24054",
"doi-asserted-by": "crossref",
"key": "4598",
"unstructured": "Nimitphong H, Holick MF. Vitamin D status and sun exposure in southeast Asia. Dermatoendocrinol 2013; 5: 34–7."
},
{
"DOI": "10.4049/jimmunol.181.10.7090",
"doi-asserted-by": "crossref",
"key": "4599",
"unstructured": "Hansdottir S, Monick MM, Hinde SL, Lovan N, Look DC, Hunninghake GW. Respiratory epithelial cells convert inactive vitamin D to its active form: Potential effects on host defense. J Immunol 2008; 181: 7090–9."
},
{
"DOI": "10.1016/j.freeradbiomed.2020.02.005",
"doi-asserted-by": "crossref",
"key": "4600",
"unstructured": "Jiang J-S, Chou H-C, Chen C-M. Cathelicidin attenuates hyperoxia-induced lung injury by inhibiting oxidative stress in newborn rats. Free Radic Biol Med 2020; 150: 23–9."
},
{
"DOI": "10.2310/JIM.0b013e31821b8755",
"doi-asserted-by": "crossref",
"key": "4601",
"unstructured": "Aranow C. Journal of investigative medicine : the official publication of the American Federation for Clinical Research 2011; 59 : 881–6."
},
{
"DOI": "10.1093/cid/ciaa329",
"doi-asserted-by": "crossref",
"key": "4602",
"unstructured": "Hanff TC, Harhay MO, Brown TS, Cohen JB, Mohareb AM. Is there an association between COVID-19 mortality and the renin-angiotensin system? A call for epidemiologic investigations. Clin Infect Dis 2020; 71: 870–4."
},
{
"DOI": "10.1001/jama.2020.26848",
"doi-asserted-by": "crossref",
"key": "4603",
"unstructured": "Murai IH, Fernandes AL, Sales LP, Pinto AJ, Goessler KF, Duran CSC, et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial. JAMA 2021; 325: 1053."
}
],
"reference-count": 29,
"references-count": 29,
"relation": {},
"resource": {
"primary": {
"URL": "https://jseamed.org/index.php/jseamed/article/view/202"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "ASSOCIATION OF VITAMIN D LEVEL AND SEVERITY OF COVID-19 DISEASE",
"type": "journal-article",
"volume": "8"
}
