Brain temperature and free water increases after mild COVID-19 infection
et al., Scientific Reports, doi:10.1038/s41598-024-57561-6, Mar 2024
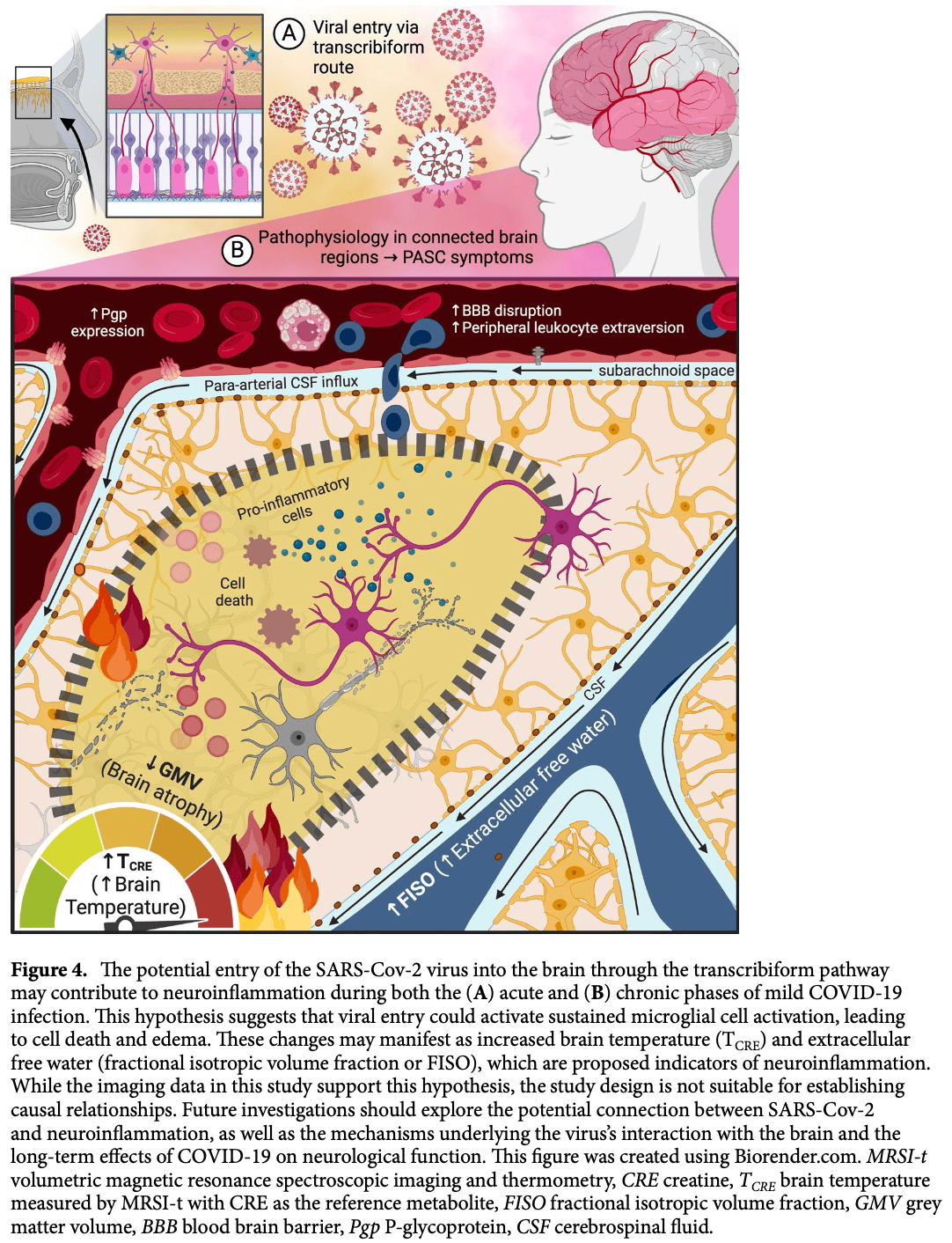
Analysis of 10 patients with brain imaging before and after mild COVID-19 suggesting that the primary route for SARS-CoV-2 entry into the central nervous system (CNS) is via the olfactory nerve in the nasal cavity, a pathway known as the transcribiform route. The findings showed that participants with chronic olfactory dysfunction had the most pronounced brain temperature increases in the primary olfactory cortex, indicating a potential link between viral entry through the olfactory pathway and persistent neurological symptoms. Authors hypothesize that SARS-CoV-2 could infect the olfactory epithelium and travel along the olfactory nerves, crossing the cribriform plate and entering the brain, leading to neuroinflammation and other neurological complications.
Sharma et al., 28 Mar 2024, USA, peer-reviewed, mean age 27.4, 4 authors, study period May 2021 - March 2023.
Contact: ayushe.sharma@yale.edu, jszaflarski@uabmc.edu.
Brain temperature and free water increases after mild COVID-19 infection
Scientific Reports, doi:10.1038/s41598-024-57561-6
The pathophysiology underlying the post-acute sequelae of COVID-19 remains understudied and poorly understood, particularly in healthy adults with a history of mild infection. Chronic neuroinflammation may underlie these enduring symptoms, but studying neuroinflammatory phenomena in vivo is challenging, especially without a comparable pre-COVID-19 dataset. In this study, we present a unique dataset of 10 otherwise healthy individuals scanned before and after experiencing mild COVID-19. Two emerging MR-based methods were used to map pre-to post-COVID-19 brain temperature and free water changes. Post-COVID-19 brain temperature and free water increases, which are indirect biomarkers of neuroinflammation, were found in structures functionally associated with olfactory, cognitive, and memory processing. The largest pre-to post-COVID brain temperature increase was observed in the left olfactory tubercle (p = 0.007, 95% CI [0.48, 3.01]), with a mean increase of 1.75 °C. Notably, the olfactory tubercle is also the region of the primary olfactory cortex where participants with chronic olfactory dysfunction showed the most pronounced increases as compared to those without lingering olfactory dysfunction (adjusted p FDR = 0.0189, 95% CI [1.42, 5.27]). These preliminary insights suggest a potential link between neuroinflammation and chronic cognitive and olfactory dysfunction following mild COVID-19, although further investigations are needed to improve our understanding of what underlies these phenomena.
Ethical statement The authors confirm that they have read the Journal's position on ethical publication, and that all study procedures and this report are consistent with those guidelines.
Author contributions All author listed made substantial, direct, and intellectual contributions to this work. Conceptualization: JPS and AAS. Data acquisition: AAS and RN. Data processing: AAS, RN, and AG. Formal analysis: AAS. Data curation: AAS. Data visualization: AAS. Writing-original draft preparation: AAS. Writing-review and editing: JPS, AAS, RN, and AG. Project supervision: JPS. Funding acquisition: JPS.
Competing interests The authors declare no competing interests.
References
Achar, Ghosh, COVID-19-associated neurological disorders: The potential route of CNS invasion and blood-brain barrier relevance, Cells
Annink, Brain temperature of infants with neonatal encephalopathy following perinatal asphyxia calculated using magnetic resonance spectroscopy, Pediatr. Res
Ansorg, Witte, Urbach, Age-dependent kinetics of dentate gyrus neurogenesis in the absence of cyclin D2, BMC Neurosci
Ashburner, Friston, Voxel-based morphometry-The methods, NeuroImage
Benjamini, Yekutieli, The Control of the False Discovery Rate in Multiple Testing Under Dependency
Bougakov, Podell, Goldberg, Multiple neuroinvasive pathways in COVID-19, Mol. Neurobiol
Cansler, Wright, Stetzik, Wesson, Neurochemical organization of the ventral striatum's olfactory tubercle, J. Neurochem
Danese, Lewis, Psychoneuroimmunology of early-life stress: The hidden wounds of childhood trauma?, Neuropsychopharmacology
Di Stadio, Olfactory dysfunction, headache, and mental clouding in adults with long-COVID-19: What is the link between cognition and olfaction? A cross-sectional study, Brain Sci
Dietrich, Alonso, Halley, Busto, Delayed posttraumatic brain hyperthermia worsens outcome after fluid percussion brain injury: A light and electron microscopic study in rats, Neurosurgery
Dietrich, Alonso, Halley, Early microvascular and neuronal consequences of traumatic brain injury: A light and electron microscopic study in rats, J. Neurotrauma
Dietrich, Atkins, Bramlett, Is Temperature an Important Variable in Recovery After Mild Traumatic Brain Injury?
Douaud, SARS-CoV-2 is associated with changes in brain structure in UK Biobank, Nature
Du, Two-year follow-up of brain structural changes in patients who recovered from COVID-19: A prospective study, Psychiatry Res
Duan, Alterations of frontal-temporal gray matter volume associate with clinical measures of older adults with COVID-19, Neurobiol. Stress
Díez-Cirarda, Multimodal neuroimaging in post-COVID syndrome and correlation with cognition, Brain
Edwards, NODDI-DTI: Estimating neurite orientation and dispersion parameters from a diffusion tensor in healthy white matter, Front. Neurosci
Fastenrath, Human cerebellum and corticocerebellar connections involved in emotional memory enhancement, Proc. Natl. Acad. Sci. USA
Frontera, Bidirectional control of fear memories by cerebellar neurons projecting to the ventrolateral periaqueductal grey, Nat. Commun
Gadziola, Tylicki, Christian, Wesson, The olfactory tubercle encodes odor valence in behaving mice, J. Neurosci
Goodman, White matter and neurite morphology differ in psychogenic nonepileptic seizures, Ann. Clin. Transl. Neurol
Graham, Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 "long haulers, Ann. Clin. Transl. Neurol
Guedj, From early limbic inflammation to long COVID sequelae, Brain
Howard, Odor quality coding and categorization in human posterior piriform cortex, Nat. Neurosci
Hugon, Cognitive decline and brainstem hypometabolism in long COVID: A case series, Brain Behav
Kamiya, Hori, Aoki, Noddi, None, Clinical Research
Lawrenson, Cerebellar modulation of memory encoding in the periaqueductal grey and fear behaviour, eLife
Lee, Neurovascular injury with complement activation and inflammation in COVID-19, Brain
Lehmann, Longitudinal reproducibility of neurite orientation dispersion and density imaging (NODDI) derived metrics in the white matter, Neuroscience
Mainland, Olfactory impairments in patients with unilateral cerebellar lesions are selective to inputs from the contralesional nostril, J. Neurosci
Mariak, The relationship between directly measured human cerebral and tympanic temperatures during changes in brain temperatures, Eur. J. Appl. Physiol. Occup. Physiol
Maudsley, Comprehensive processing, display and analysis for in vivo MR spectroscopic imaging, NMR Biomed
Maudsley, Goryawala, Sheriff, Effects of tissue susceptibility on brain temperature mapping, NeuroImage
Mcfarquhar, Multivariate and repeated measures (MRM): A new toolbox for dependent and multimodal group-level neuroimaging data, Neuroimage
Mcilvoy, Comparison of brain temperature to core temperature: A review of the literature, J. Neurosci. Nurs
Mcnair, Lorr, Droppleman, Profile of Mood States (POMS)
Mizrahi, Long covid outcomes at one year after mild SARS-CoV-2 infection: Nationwide cohort study, BMJ
Najt, Richards, Fortune, Brain imaging in patients with COVID-19: A systematic review, Brain Behav. Immunity Health
Nigri, Connectivity of the amygdala, piriform, and orbitofrontal cortex during olfactory stimulation: A functional MRI study, NeuroReport
Qin, Long-term microstructure and cerebral blood flow changes in patients recovered from COVID-19 without neurological manifestations, J. Clin. Invest
Rau, Widespread white matter oedema in subacute COVID-19 patients with neurological symptoms, Brain
Ravi, Miller, Michopoulos, The immunology of stress and the impact of inflammation on the brain and behaviour, BJPsych. Adv
Rostampour, Hashemi, Najibi, Oghabian, Detection of structural abnormalities of cortical and subcortical gray matter in patients with MRI-negative refractory epilepsy using neurite orientation dispersion and density imaging, Phys. Med
Rzechorzek, A daily temperature rhythm in the human brain predicts survival after brain injury, Brain
Salomon, Brain volumetric changes in the general population following the COVID-19 outbreak and lockdown, NeuroImage
Sepehrband, Brain tissue compartment density estimated using diffusion-weighted MRI yields tissue parameters consistent with histology, Hum. Brain Mapp
Sharma, A preliminary study of the effects of cannabidiol (CBD) on brain structure in patients with epilepsy, Epilepsy Behav. Rep
Sharma, Nenert, Goodman, Szaflarski, Concordance between focal brain temperature elevations and focal edema in temporal lobe epilepsy, Epilepsia
Sharma, Repeatability and reproducibility of in-vivo brain temperature measurements, Front. Hum. Neurosci
Sherif, Pathogenic mechanisms of post-acute sequelae of SARS-CoV-2 infection (PASC), eLife
Sone, Abnormal neurite density and orientation dispersion in unilateral temporal lobe epilepsy detected by advanced diffusion imaging, NeuroImage Clin
Stettler, Axel, Representations of odor in the piriform cortex, Neuron
Taribagil, Creer, Tahir, Long COVID syndrome, BMJ Case Rep
Troubat, Neuroinflammation and depression: A review, Eur. J. Neurosci
Van Kessel, Olde Hartman, Lucassen, Van Jaarsveld, Post-acute and long-COVID-19 symptoms in patients with mild diseases: A systematic review, Fam. Pract
Visser, Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET
Wang, Brain temperature and its fundamental properties: A review for clinical neuroscientists, Front. Neurosci
Winston, The potential role of novel diffusion imaging techniques in the understanding and treatment of epilepsy, Quant. Imaging Med. Surg
Xydakis, Post-viral effects of COVID-19 in the olfactory system and their implications, Lancet Neurol
Zelano, Montag, Khan, Sobel, A specialized odor memory buffer in primary olfactory cortex, PLOS ONE
Zhang, Cerebellar involvement in olfaction: An fMRI study, J Neuroimaging
Zhang, Schneider, Wheeler-Kingshott, Alexander, Noddi, Practical in vivo neurite orientation dispersion and density imaging of the human brain, NeuroImage
Zhao, Rapid vigilance and episodic memory decrements in COVID-19 survivors, Brain Commun
Zhou, Characterizing functional pathways of the human olfactory system, eLife
Zigmond, Snaith, The hospital anxiety and depression scale, Acta Psychiatr. Scand
DOI record:
{
"DOI": "10.1038/s41598-024-57561-6",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-024-57561-6",
"abstract": "<jats:title>Abstract</jats:title><jats:p>The pathophysiology underlying the post-acute sequelae of COVID-19 remains understudied and poorly understood, particularly in healthy adults with a history of mild infection. Chronic neuroinflammation may underlie these enduring symptoms, but studying neuroinflammatory phenomena in vivo is challenging, especially without a comparable pre-COVID-19 dataset. In this study, we present a unique dataset of 10 otherwise healthy individuals scanned before and after experiencing mild COVID-19. Two emerging MR-based methods were used to map pre- to post-COVID-19 brain temperature and free water changes. Post-COVID-19 brain temperature and free water increases, which are indirect biomarkers of neuroinflammation, were found in structures functionally associated with olfactory, cognitive, and memory processing. The largest pre- to post-COVID brain temperature increase was observed in the left olfactory tubercle (<jats:italic>p</jats:italic> = 0.007, 95% CI [0.48, 3.01]), with a mean increase of 1.75 °C. Notably, the olfactory tubercle is also the region of the primary olfactory cortex where participants with chronic olfactory dysfunction showed the most pronounced increases as compared to those without lingering olfactory dysfunction (adjusted <jats:italic>p</jats:italic><jats:sub>FDR</jats:sub> = 0.0189, 95% CI [1.42, 5.27]). These preliminary insights suggest a potential link between neuroinflammation and chronic cognitive and olfactory dysfunction following mild COVID-19, although further investigations are needed to improve our understanding of what underlies these phenomena.</jats:p>",
"alternative-id": [
"57561"
],
"article-number": "7450",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "12 September 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "19 March 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "28 March 2024"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Sharma",
"given": "Ayushe A.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Nenert",
"given": "Rodolphe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Goodman",
"given": "Adam M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Szaflarski",
"given": "Jerzy P.",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
3,
28
]
],
"date-time": "2024-03-28T22:01:38Z",
"timestamp": 1711663298000
},
"deposited": {
"date-parts": [
[
2024,
3,
28
]
],
"date-time": "2024-03-28T23:01:24Z",
"timestamp": 1711666884000
},
"funder": [
{
"award": [
"1F31NS129288-01",
"T32-NS061788-13"
],
"name": "U.S. Department of Health & Human Services | NIH | National Institute of Neurological Disorders and Stroke"
},
{
"name": "In addition to the funders listed above (PI: AS), the State of Alabama General Fund and the UAB Epilepsy Center supported this study"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
29
]
],
"date-time": "2024-03-29T01:30:19Z",
"timestamp": 1711675819149
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
3,
28
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
3,
28
]
],
"date-time": "2024-03-28T00:00:00Z",
"timestamp": 1711584000000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
3,
28
]
],
"date-time": "2024-03-28T00:00:00Z",
"timestamp": 1711584000000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-024-57561-6.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-57561-6",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-57561-6.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2024,
3,
28
]
]
},
"published-online": {
"date-parts": [
[
2024,
3,
28
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1093/fampra/cmab076",
"author": "SAM Van Kessel",
"doi-asserted-by": "publisher",
"first-page": "159",
"issue": "1",
"journal-title": "Fam. Pract.",
"key": "57561_CR1",
"unstructured": "Van Kessel, S. A. M., Olde Hartman, T. C., Lucassen, P. L. B. J. & Van Jaarsveld, C. H. M. Post-acute and long-COVID-19 symptoms in patients with mild diseases: A systematic review. Fam. Pract. 39(1), 159–167 (2022).",
"volume": "39",
"year": "2022"
},
{
"DOI": "10.1136/bmj-2022-072529",
"author": "B Mizrahi",
"doi-asserted-by": "publisher",
"first-page": "e072529",
"journal-title": "BMJ",
"key": "57561_CR2",
"unstructured": "Mizrahi, B. et al. Long covid outcomes at one year after mild SARS-CoV-2 infection: Nationwide cohort study. BMJ 380, e072529–e072529 (2023).",
"volume": "380",
"year": "2023"
},
{
"DOI": "10.1016/j.psychres.2022.114969",
"author": "Y Du",
"doi-asserted-by": "publisher",
"first-page": "114969",
"journal-title": "Psychiatry Res.",
"key": "57561_CR3",
"unstructured": "Du, Y. et al. Two-year follow-up of brain structural changes in patients who recovered from COVID-19: A prospective study. Psychiatry Res. 319, 114969–114969 (2023).",
"volume": "319",
"year": "2023"
},
{
"DOI": "10.3390/brainsci12020154",
"author": "A Di Stadio",
"doi-asserted-by": "publisher",
"first-page": "122",
"issue": "2",
"journal-title": "Brain Sci.",
"key": "57561_CR4",
"unstructured": "Di Stadio, A. et al. Olfactory dysfunction, headache, and mental clouding in adults with long-COVID-19: What is the link between cognition and olfaction? A cross-sectional study. Brain Sci. 12(2), 122 (2022).",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1002/acn3.51350",
"author": "EL Graham",
"doi-asserted-by": "publisher",
"first-page": "1073",
"issue": "5",
"journal-title": "Ann. Clin. Transl. Neurol.",
"key": "57561_CR5",
"unstructured": "Graham, E. L. et al. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 “long haulers”. Ann. Clin. Transl. Neurol. 8(5), 1073–1085 (2021).",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1093/braincomms/fcab295",
"author": "S Zhao",
"doi-asserted-by": "publisher",
"first-page": "33",
"issue": "1",
"journal-title": "Brain Commun.",
"key": "57561_CR6",
"unstructured": "Zhao, S. et al. Rapid vigilance and episodic memory decrements in COVID-19 survivors. Brain Commun. 4(1), 33 (2022).",
"volume": "4",
"year": "2022"
},
{
"DOI": "10.1016/j.bbih.2021.100290",
"author": "P Najt",
"doi-asserted-by": "publisher",
"first-page": "100290",
"journal-title": "Brain Behav. Immunity Health",
"key": "57561_CR7",
"unstructured": "Najt, P., Richards, H. L. & Fortune, D. G. Brain imaging in patients with COVID-19: A systematic review. Brain Behav. Immunity Health 16, 100290–100290 (2021).",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1002/brb3.2513",
"author": "J Hugon",
"doi-asserted-by": "publisher",
"first-page": "e2513",
"issue": "4",
"journal-title": "Brain Behav.",
"key": "57561_CR8",
"unstructured": "Hugon, J. et al. Cognitive decline and brainstem hypometabolism in long COVID: A case series. Brain Behav. 12(4), e2513–e2513 (2022).",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1093/brain/awac384",
"author": "M Díez-Cirarda",
"doi-asserted-by": "publisher",
"first-page": "2142",
"journal-title": "Brain",
"key": "57561_CR9",
"unstructured": "Díez-Cirarda, M. et al. Multimodal neuroimaging in post-COVID syndrome and correlation with cognition. Brain 146, 2142 (2022).",
"volume": "146",
"year": "2022"
},
{
"DOI": "10.1038/s41586-022-04569-5",
"author": "G Douaud",
"doi-asserted-by": "publisher",
"first-page": "697",
"issue": "7907",
"journal-title": "Nature",
"key": "57561_CR10",
"unstructured": "Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604(7907), 697–707 (2022).",
"volume": "604",
"year": "2022"
},
{
"key": "57561_CR11",
"unstructured": "Visser, D. et al. Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET. medRxiv 2022.06.02.22275916–2022.06.02.22275916 (2022)."
},
{
"DOI": "10.1093/brain/awac151",
"author": "MH Lee",
"doi-asserted-by": "publisher",
"first-page": "2555",
"journal-title": "Brain",
"key": "57561_CR12",
"unstructured": "Lee, M. H. et al. Neurovascular injury with complement activation and inflammation in COVID-19. Brain 145, 2555 (2022).",
"volume": "145",
"year": "2022"
},
{
"DOI": "10.1093/brain/awac045",
"author": "A Rau",
"doi-asserted-by": "publisher",
"first-page": "3203",
"issue": "9",
"journal-title": "Brain",
"key": "57561_CR13",
"unstructured": "Rau, A. et al. Widespread white matter oedema in subacute COVID-19 patients with neurological symptoms. Brain 145(9), 3203–3213 (2022).",
"volume": "145",
"year": "2022"
},
{
"DOI": "10.1172/JCI147329",
"author": "Y Qin",
"doi-asserted-by": "publisher",
"first-page": "1473",
"issue": "8",
"journal-title": "J. Clin. Invest.",
"key": "57561_CR14",
"unstructured": "Qin, Y. et al. Long-term microstructure and cerebral blood flow changes in patients recovered from COVID-19 without neurological manifestations. J. Clin. Invest. 131(8), 1473 (2021).",
"volume": "131",
"year": "2021"
},
{
"DOI": "10.1111/epi.17538",
"author": "AA Sharma",
"doi-asserted-by": "publisher",
"first-page": "1289",
"journal-title": "Epilepsia",
"key": "57561_CR15",
"unstructured": "Sharma, A. A., Nenert, R., Goodman, A. & Szaflarski, J. P. Concordance between focal brain temperature elevations and focal edema in temporal lobe epilepsy. Epilepsia 65, 1289 (2023).",
"volume": "65",
"year": "2023"
},
{
"DOI": "10.3389/fnhum.2020.598435",
"author": "AA Sharma",
"doi-asserted-by": "publisher",
"first-page": "598435",
"journal-title": "Front. Hum. Neurosci.",
"key": "57561_CR16",
"unstructured": "Sharma, A. A. et al. Repeatability and reproducibility of in-vivo brain temperature measurements. Front. Hum. Neurosci. 14, 598435–598435 (2020).",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/BF00239873",
"author": "Z Mariak",
"doi-asserted-by": "publisher",
"first-page": "545",
"issue": "6",
"journal-title": "Eur. J. Appl. Physiol. Occup. Physiol.",
"key": "57561_CR17",
"unstructured": "Mariak, Z. et al. The relationship between directly measured human cerebral and tympanic temperatures during changes in brain temperatures. Eur. J. Appl. Physiol. Occup. Physiol. 69(6), 545–549 (1994).",
"volume": "69",
"year": "1994"
},
{
"DOI": "10.1097/01376517-200402000-00004",
"author": "L McIlvoy",
"doi-asserted-by": "publisher",
"first-page": "23",
"issue": "1",
"journal-title": "J. Neurosci. Nurs.",
"key": "57561_CR18",
"unstructured": "McIlvoy, L. Comparison of brain temperature to core temperature: A review of the literature. J. Neurosci. Nurs. 36(1), 23–31 (2004).",
"volume": "36",
"year": "2004"
},
{
"DOI": "10.3389/fnins.2014.00307",
"author": "H Wang",
"doi-asserted-by": "publisher",
"first-page": "307",
"journal-title": "Front. Neurosci.",
"key": "57561_CR19",
"unstructured": "Wang, H. et al. Brain temperature and its fundamental properties: A review for clinical neuroscientists. Front. Neurosci. 8, 307 (2014).",
"volume": "8",
"year": "2014"
},
{
"key": "57561_CR20",
"unstructured": "Dietrich, W.D., Atkins, C.M. & Bramlett, H.M. Is Temperature an Important Variable in Recovery After Mild Traumatic Brain Injury? (Faculty of 1000 Ltd., 2017)."
},
{
"DOI": "10.1089/neu.1994.11.289",
"author": "WD Dietrich",
"doi-asserted-by": "publisher",
"first-page": "289",
"issue": "3",
"journal-title": "J. Neurotrauma",
"key": "57561_CR21",
"unstructured": "Dietrich, W. D., Alonso, O. & Halley, M. Early microvascular and neuronal consequences of traumatic brain injury: A light and electron microscopic study in rats. J. Neurotrauma 11(3), 289–301 (1994).",
"volume": "11",
"year": "1994"
},
{
"author": "WD Dietrich",
"first-page": "533",
"issue": "3",
"journal-title": "Neurosurgery",
"key": "57561_CR22",
"unstructured": "Dietrich, W. D., Alonso, O., Halley, M. & Busto, R. Delayed posttraumatic brain hyperthermia worsens outcome after fluid percussion brain injury: A light and electron microscopic study in rats. Neurosurgery 38(3), 533–541 (1996).",
"volume": "38",
"year": "1996"
},
{
"DOI": "10.1038/s41390-019-0739-3",
"author": "KV Annink",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Pediatr. Res.",
"key": "57561_CR23",
"unstructured": "Annink, K. V. et al. Brain temperature of infants with neonatal encephalopathy following perinatal asphyxia calculated using magnetic resonance spectroscopy. Pediatr. Res. 88, 1–6 (2020).",
"volume": "88",
"year": "2020"
},
{
"key": "57561_CR24",
"unstructured": "Brain Temperature: Physiology and Pathophysiology after Brain Injury. 13-13 (Hindawi Publishing Corporation)."
},
{
"DOI": "10.1093/brain/awab466",
"author": "NM Rzechorzek",
"doi-asserted-by": "publisher",
"first-page": "2031",
"issue": "6",
"journal-title": "Brain",
"key": "57561_CR25",
"unstructured": "Rzechorzek, N. M. et al. A daily temperature rhythm in the human brain predicts survival after brain injury. Brain 145(6), 2031–2048 (2022).",
"volume": "145",
"year": "2022"
},
{
"DOI": "10.1111/j.1600-0447.1983.tb09716.x",
"author": "AS Zigmond",
"doi-asserted-by": "publisher",
"first-page": "361",
"journal-title": "Acta Psychiatr. Scand.",
"key": "57561_CR26",
"unstructured": "Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361 (1983).",
"volume": "67",
"year": "1983"
},
{
"key": "57561_CR27",
"unstructured": "McNair, D., Lorr, M. & Droppleman, L.F. Profile of Mood States (POMS) (1989)."
},
{
"DOI": "10.1006/nimg.2000.0582",
"author": "J Ashburner",
"doi-asserted-by": "publisher",
"first-page": "805",
"issue": "6",
"journal-title": "NeuroImage",
"key": "57561_CR28",
"unstructured": "Ashburner, J. & Friston, K. J. Voxel-based morphometry—The methods. NeuroImage 11(6), 805–821 (2000).",
"volume": "11",
"year": "2000"
},
{
"DOI": "10.1016/j.ebr.2019.100341",
"doi-asserted-by": "crossref",
"key": "57561_CR29",
"unstructured": "Sharma, A.A. et al. A preliminary study of the effects of cannabidiol (CBD) on brain structure in patients with epilepsy. Epilepsy Behav. Rep. 12, 81 (2019)."
},
{
"DOI": "10.1002/nbm.1025",
"author": "AA Maudsley",
"doi-asserted-by": "publisher",
"first-page": "492",
"issue": "4",
"journal-title": "NMR Biomed.",
"key": "57561_CR30",
"unstructured": "Maudsley, A. A. et al. Comprehensive processing, display and analysis for in vivo MR spectroscopic imaging. NMR Biomed. 19(4), 492–503 (2006).",
"volume": "19",
"year": "2006"
},
{
"DOI": "10.1016/j.neuroimage.2016.09.062",
"author": "AA Maudsley",
"doi-asserted-by": "publisher",
"first-page": "1093",
"journal-title": "NeuroImage",
"key": "57561_CR31",
"unstructured": "Maudsley, A. A., Goryawala, M. Z. & Sheriff, S. Effects of tissue susceptibility on brain temperature mapping. NeuroImage 146, 1093–1101 (2017).",
"volume": "146",
"year": "2017"
},
{
"DOI": "10.1016/j.nicl.2018.09.017",
"author": "D Sone",
"doi-asserted-by": "publisher",
"first-page": "772",
"journal-title": "NeuroImage Clin.",
"key": "57561_CR32",
"unstructured": "Sone, D. et al. Abnormal neurite density and orientation dispersion in unilateral temporal lobe epilepsy detected by advanced diffusion imaging. NeuroImage Clin. 20, 772–772 (2018).",
"volume": "20",
"year": "2018"
},
{
"DOI": "10.1016/j.neuroimage.2012.03.072",
"author": "H Zhang",
"doi-asserted-by": "publisher",
"first-page": "1000",
"issue": "4",
"journal-title": "NeuroImage",
"key": "57561_CR33",
"unstructured": "Zhang, H., Schneider, T., Wheeler-Kingshott, C. A. & Alexander, D. C. NODDI: Practical in vivo neurite orientation dispersion and density imaging of the human brain. NeuroImage 61(4), 1000–1016 (2012).",
"volume": "61",
"year": "2012"
},
{
"DOI": "10.1002/hbm.22872",
"author": "F Sepehrband",
"doi-asserted-by": "publisher",
"first-page": "3687",
"issue": "9",
"journal-title": "Hum. Brain Mapp.",
"key": "57561_CR34",
"unstructured": "Sepehrband, F. et al. Brain tissue compartment density estimated using diffusion-weighted MRI yields tissue parameters consistent with histology. Hum. Brain Mapp. 36(9), 3687–3702 (2015).",
"volume": "36",
"year": "2015"
},
{
"DOI": "10.1016/j.jneumeth.2020.108908",
"doi-asserted-by": "crossref",
"key": "57561_CR35",
"unstructured": "Kamiya, K., Hori, M. & Aoki, S. NODDI in Clinical Research. 108908–108908 (Elsevier B.V., 2020)."
},
{
"DOI": "10.1002/acn3.51198",
"author": "AM Goodman",
"doi-asserted-by": "publisher",
"first-page": "1973",
"issue": "10",
"journal-title": "Ann. Clin. Transl. Neurol.",
"key": "57561_CR36",
"unstructured": "Goodman, A. M. et al. White matter and neurite morphology differ in psychogenic nonepileptic seizures. Ann. Clin. Transl. Neurol. 7(10), 1973–1984 (2020).",
"volume": "7",
"year": "2020"
},
{
"author": "GP Winston",
"first-page": "279",
"issue": "2",
"journal-title": "Quant. Imaging Med. Surg.",
"key": "57561_CR37",
"unstructured": "Winston, G. P. The potential role of novel diffusion imaging techniques in the understanding and treatment of epilepsy. Quant. Imaging Med. Surg. 5(2), 279–27987 (2015).",
"volume": "5",
"year": "2015"
},
{
"DOI": "10.1016/j.ejmp.2018.03.005",
"author": "M Rostampour",
"doi-asserted-by": "publisher",
"first-page": "47",
"journal-title": "Phys. Med.",
"key": "57561_CR38",
"unstructured": "Rostampour, M., Hashemi, H., Najibi, S. M. & Oghabian, M. A. Detection of structural abnormalities of cortical and subcortical gray matter in patients with MRI-negative refractory epilepsy using neurite orientation dispersion and density imaging. Phys. Med. 48, 47–54 (2018).",
"volume": "48",
"year": "2018"
},
{
"DOI": "10.3389/fnins.2017.00720",
"doi-asserted-by": "crossref",
"key": "57561_CR39",
"unstructured": "Edwards, L.J. et al. NODDI-DTI: Estimating neurite orientation and dispersion parameters from a diffusion tensor in healthy white matter. Front. Neurosci. 11, 33 (2017)."
},
{
"DOI": "10.7554/eLife.47177",
"doi-asserted-by": "crossref",
"key": "57561_CR40",
"unstructured": "Zhou, G. et al. Characterizing functional pathways of the human olfactory system. eLife 8, 14 (2019)."
},
{
"DOI": "10.1016/j.neuroimage.2016.02.053",
"author": "M McFarquhar",
"doi-asserted-by": "publisher",
"first-page": "373",
"journal-title": "Neuroimage",
"key": "57561_CR41",
"unstructured": "McFarquhar, M. et al. Multivariate and repeated measures (MRM): A new toolbox for dependent and multimodal group-level neuroimaging data. Neuroimage 132, 373–373 (2016).",
"volume": "132",
"year": "2016"
},
{
"DOI": "10.1214/aos/1013699998",
"doi-asserted-by": "crossref",
"key": "57561_CR42",
"unstructured": "Benjamini, Y. & Yekutieli, D. The Control of the False Discovery Rate in Multiple Testing Under Dependency. 1165–1188 (2001)."
},
{
"DOI": "10.1016/j.ynstr.2021.100326",
"author": "K Duan",
"doi-asserted-by": "publisher",
"first-page": "100326",
"journal-title": "Neurobiol. Stress",
"key": "57561_CR43",
"unstructured": "Duan, K. et al. Alterations of frontal-temporal gray matter volume associate with clinical measures of older adults with COVID-19. Neurobiol. Stress 14, 100326–100326 (2021).",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1523/JNEUROSCI.4750-14.2015",
"author": "MA Gadziola",
"doi-asserted-by": "publisher",
"first-page": "4515",
"issue": "11",
"journal-title": "J. Neurosci.",
"key": "57561_CR44",
"unstructured": "Gadziola, M. A., Tylicki, K. A., Christian, D. L. & Wesson, D. W. The olfactory tubercle encodes odor valence in behaving mice. J. Neurosci. 35(11), 4515–4527 (2015).",
"volume": "35",
"year": "2015"
},
{
"DOI": "10.1111/jnc.14919",
"author": "HL Cansler",
"doi-asserted-by": "publisher",
"first-page": "425",
"issue": "4",
"journal-title": "J. Neurochem.",
"key": "57561_CR45",
"unstructured": "Cansler, H. L., Wright, K. N., Stetzik, L. A. & Wesson, D. W. Neurochemical organization of the ventral striatum’s olfactory tubercle. J. Neurochem. 152(4), 425–425 (2020).",
"volume": "152",
"year": "2020"
},
{
"DOI": "10.1038/nn.2324",
"doi-asserted-by": "crossref",
"key": "57561_CR46",
"unstructured": "Howard, J.D. et al. Odor quality coding and categorization in human posterior piriform cortex. Nat. Neurosci. 12(7), 932–938 (2009)."
},
{
"DOI": "10.1371/journal.pone.0004965",
"author": "C Zelano",
"doi-asserted-by": "publisher",
"first-page": "e4965",
"issue": "3",
"journal-title": "PLOS ONE",
"key": "57561_CR47",
"unstructured": "Zelano, C., Montag, J., Khan, R. & Sobel, N. A specialized odor memory buffer in primary olfactory cortex. PLOS ONE 4(3), e4965–e4965 (2009).",
"volume": "4",
"year": "2009"
},
{
"DOI": "10.1016/j.neuron.2009.09.005",
"author": "DD Stettler",
"doi-asserted-by": "publisher",
"first-page": "854",
"issue": "6",
"journal-title": "Neuron",
"key": "57561_CR48",
"unstructured": "Stettler, D. D. & Axel, R. Representations of odor in the piriform cortex. Neuron 63(6), 854–864 (2009).",
"volume": "63",
"year": "2009"
},
{
"DOI": "10.1093/brain/awab215",
"author": "E Guedj",
"doi-asserted-by": "publisher",
"first-page": "e65",
"issue": "8",
"journal-title": "Brain",
"key": "57561_CR49",
"unstructured": "Guedj, E. et al. From early limbic inflammation to long COVID sequelae. Brain 144(8), e65–e65 (2021).",
"volume": "144",
"year": "2021"
},
{
"DOI": "10.1523/JNEUROSCI.0920-05.2005",
"author": "JD Mainland",
"doi-asserted-by": "publisher",
"first-page": "6362",
"issue": "27",
"journal-title": "J. Neurosci.",
"key": "57561_CR50",
"unstructured": "Mainland, J. D. et al. Olfactory impairments in patients with unilateral cerebellar lesions are selective to inputs from the contralesional nostril. J. Neurosci. 25(27), 6362–6362 (2005).",
"volume": "25",
"year": "2005"
},
{
"DOI": "10.1111/jon.12843",
"doi-asserted-by": "crossref",
"key": "57561_CR51",
"unstructured": "Zhang, Z.H. et al. Cerebellar involvement in olfaction: An fMRI study. J Neuroimaging 31(3), 517–523 (2021)."
},
{
"DOI": "10.7554/eLife.76278",
"doi-asserted-by": "crossref",
"key": "57561_CR52",
"unstructured": "Lawrenson, C. et al. Cerebellar modulation of memory encoding in the periaqueductal grey and fear behaviour. eLife 11, 7627 (2022)."
},
{
"DOI": "10.1073/pnas.2204900119",
"author": "M Fastenrath",
"doi-asserted-by": "publisher",
"first-page": "e2204900119",
"issue": "41",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "57561_CR53",
"unstructured": "Fastenrath, M. et al. Human cerebellum and corticocerebellar connections involved in emotional memory enhancement. Proc. Natl. Acad. Sci. USA 119(41), e2204900119–e2204900119 (2022).",
"volume": "119",
"year": "2022"
},
{
"DOI": "10.1038/s41467-020-18953-0",
"doi-asserted-by": "crossref",
"key": "57561_CR54",
"unstructured": "Frontera, J.L. et al. Bidirectional control of fear memories by cerebellar neurons projecting to the ventrolateral periaqueductal grey. Nat. Commun. 11(1), 1–17 (2020)."
},
{
"DOI": "10.1192/bja.2020.82",
"author": "M Ravi",
"doi-asserted-by": "publisher",
"first-page": "158",
"issue": "3",
"journal-title": "BJPsych. Adv.",
"key": "57561_CR55",
"unstructured": "Ravi, M., Miller, A. H. & Michopoulos, V. The immunology of stress and the impact of inflammation on the brain and behaviour. BJPsych. Adv. 27(3), 158–165 (2021).",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1111/ejn.14720",
"author": "R Troubat",
"doi-asserted-by": "publisher",
"first-page": "151",
"issue": "1",
"journal-title": "Eur. J. Neurosci.",
"key": "57561_CR56",
"unstructured": "Troubat, R. et al. Neuroinflammation and depression: A review. Eur. J. Neurosci. 53(1), 151–171 (2021).",
"volume": "53",
"year": "2021"
},
{
"DOI": "10.1016/j.neuroimage.2021.118311",
"author": "T Salomon",
"doi-asserted-by": "publisher",
"first-page": "118311",
"journal-title": "NeuroImage",
"key": "57561_CR57",
"unstructured": "Salomon, T. et al. Brain volumetric changes in the general population following the COVID-19 outbreak and lockdown. NeuroImage 239, 118311–118311 (2021).",
"volume": "239",
"year": "2021"
},
{
"DOI": "10.1136/bcr-2020-241485",
"author": "P Taribagil",
"doi-asserted-by": "publisher",
"first-page": "e241485",
"issue": "4",
"journal-title": "BMJ Case Rep.",
"key": "57561_CR58",
"unstructured": "Taribagil, P., Creer, D. & Tahir, H. Long COVID syndrome. BMJ Case Rep. 14(4), e241485–e241485 (2021).",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.3390/cells9112360",
"author": "A Achar",
"doi-asserted-by": "publisher",
"first-page": "2360",
"issue": "11",
"journal-title": "Cells",
"key": "57561_CR59",
"unstructured": "Achar, A. & Ghosh, C. COVID-19-associated neurological disorders: The potential route of CNS invasion and blood–brain barrier relevance. Cells 9(11), 2360–2360 (2020).",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1007/s12035-020-02152-5",
"doi-asserted-by": "crossref",
"key": "57561_CR60",
"unstructured": "Bougakov, D., Podell, K. & Goldberg, E. Multiple neuroinvasive pathways in COVID-19. Mol. Neurobiol. 58(2), 564–575 (2020)."
},
{
"DOI": "10.1038/npp.2016.198",
"doi-asserted-by": "crossref",
"key": "57561_CR61",
"unstructured": "Danese, A. & Lewis, S. J. Psychoneuroimmunology of early-life stress: The hidden wounds of childhood trauma? Neuropsychopharmacology 42(1), 99–114 (2017)."
},
{
"DOI": "10.1186/1471-2202-13-46",
"doi-asserted-by": "crossref",
"key": "57561_CR62",
"unstructured": "Ansorg, A., Witte, O.W. & Urbach, A. Age-dependent kinetics of dentate gyrus neurogenesis in the absence of cyclin D2. BMC Neurosci. 13(1), 56 (2012)."
},
{
"DOI": "10.1097/WNR.0b013e32835d5d2b",
"author": "A Nigri",
"doi-asserted-by": "publisher",
"first-page": "171",
"issue": "4",
"journal-title": "NeuroReport",
"key": "57561_CR63",
"unstructured": "Nigri, A. et al. Connectivity of the amygdala, piriform, and orbitofrontal cortex during olfactory stimulation: A functional MRI study. NeuroReport 24(4), 171–175 (2013).",
"volume": "24",
"year": "2013"
},
{
"DOI": "10.1016/S1474-4422(21)00182-4",
"author": "MS Xydakis",
"doi-asserted-by": "publisher",
"first-page": "753",
"issue": "9",
"journal-title": "Lancet Neurol.",
"key": "57561_CR64",
"unstructured": "Xydakis, M. S. et al. Post-viral effects of COVID-19 in the olfactory system and their implications. Lancet Neurol. 20(9), 753–753 (2021).",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.7554/eLife.86002",
"doi-asserted-by": "crossref",
"key": "57561_CR65",
"unstructured": "Sherif, Z.A. et al. Pathogenic mechanisms of post-acute sequelae of SARS-CoV-2 infection (PASC). eLife 12, e86002 (2023)."
},
{
"DOI": "10.1016/j.neuroscience.2021.01.005",
"doi-asserted-by": "crossref",
"key": "57561_CR66",
"unstructured": "Lehmann, N. et al. Longitudinal reproducibility of neurite orientation dispersion and density imaging (NODDI) derived metrics in the white matter. Neuroscience 457, 4 (2021)."
}
],
"reference-count": 66,
"references-count": 66,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-024-57561-6"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Brain temperature and free water increases after mild COVID-19 infection",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "14"
}