Dietary mineral intakes predict Coronavirus-disease 2019 (COVID-19) incidence and hospitalization in older adults
et al., BMC Nutrition, doi:10.1186/s40795-024-00821-5, Mar 2024
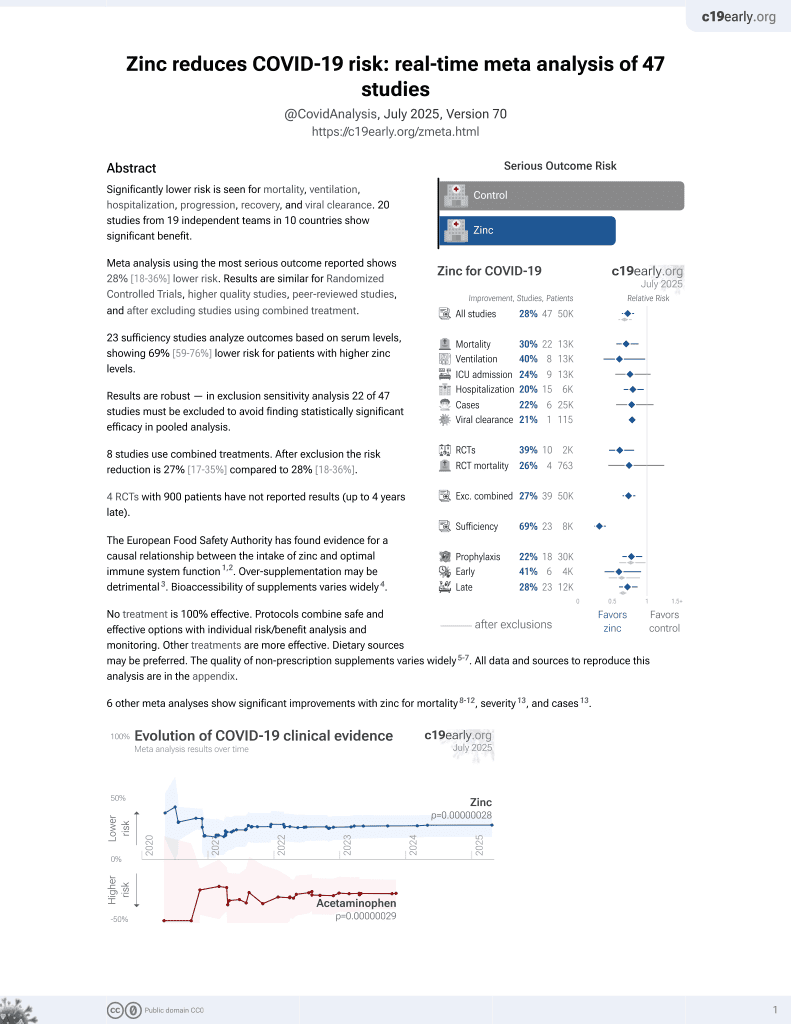
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000019 from 42 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
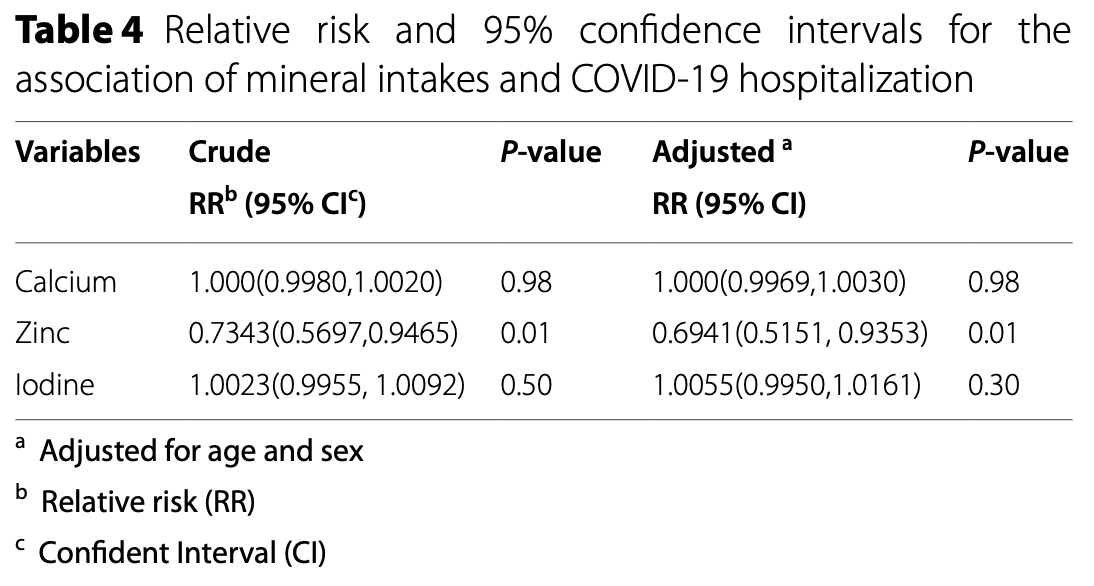
Analysis of 1,957 older adults showing lower risk of COVID-19 hospitalization with higher dietary zinc intake. Each unit increase in zinc intake was associated with a 31% reduction in the risk of COVID-19 hospitalization after adjustments. A dynamical system model showed that consumption of zinc < 9.7mg per day was associated with a 1.5 times greater risk of COVID-19 infection.
The dietary mineral intakes were collected using a Food Frequency Questionnaire (FFQ) between 2007-2010 during the first phase of the MASHAD study. This data was used to predict COVID-19 incidence and hospitalization between 2020-2022. A gap of 10 to 15 years introduces confounding, as dietary habits may change significantly over time.
This study is excluded in the after exclusion results of meta-analysis:
the hospitalization result is only provided with respect to continuous values and the confidence interval is not reported for the case result.
|
risk of hospitalization, 30.6% lower, OR 0.69, p = 0.02, RR approximated with OR, per unit change, per unit change.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Seifi et al., 4 Mar 2024, retrospective, Iran, peer-reviewed, mean age 49.7, 8 authors, study period February 2020 - June 2022.
Contact: ghayourmobarhan@yahoo.com.
Dietary mineral intakes predict Coronavirus-disease 2019 (COVID-19) incidence and hospitalization in older adults
BMC Nutrition, doi:10.1186/s40795-024-00821-5
Background The aim of this study was to determine the association between dietary mineral intake and Coronavirus-disease 2019 (COVID-19) infection and its associated hospitalization. Methods This cohort study utilized the MASHAD study population, which comprised individuals aged 35-65. Upon recruitment in 2007, dietary intake was documented using a validated 65-item food frequency questionnaire (FFQ). Data on COVID-19 PCR test results was collected from all relevant medical centers in Mashhad between February 2020 and June 2022. The regression model included dietary minerals and employed the backward variable selection method, along with advanced data analysis techniques.
Results The final analysis involved 1957 participants, including 193 COVID-19-positive patients. The mean age was 49.71 and 50.28 years in the COVID-19-positive and negative groups, respectively (p = 0.12). Dietary intakes of magnesium, iron, and potassium were notably lower in COVID-19-positive patients (P < 0.05). Following adjustments for age and sex, dietary iron remained significantly associated with COVID-19 incidence (OR = 0.94, 95% CI: 0.90-0.98). Furthermore, a statistically significant relationship was observed between dietary zinc and hospitalization due to COVID-19 (OR = 0.69, 95% CI: 0.51-0.93). In dynamical system models, intakes of calcium, zinc, and iron below the cut-offs of 1138, 9.7, and 8.17 mg/day, respectively, were linked to an increased risk of COVID-19 incidence.
Conclusion Higher dietary iron and zinc intake are associated with decreased risk of COVID-19 infection and hospitalization, respectively.
Authors' contributions N.S. and M.Gh. designed study. A.A. and H.B. collected data. EM.F. and S.Gh. analyzed data. F.Gh, H.B. and N.S. wrote the main manuscript text. G.A.F. and M.Gh. did critical revision. All authors reviewed the manuscript.
Declarations Ethics approval and consent to participate All experiments were performed in accordance with the declaration of Helsinki and Mashhad University of Medical Sciences ethical guidelines and regulations. The research protocol was approved by the School of Medicine, Mashhad University of Medical Sciences, Biomedical Research Ethics Committee (IR.MUMS.MEDICAL.REC.1398.228). All participants signed a written inform consent before participating in the study.
Consent for publication Not applicable.
Competing interests The authors declare no competing interests.
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Abdulah, Hassan, Relation of dietary factors with infection and mortality rates of COVID-19 across the world, J Nutr Health Aging
Andreini, Putignano, Rosato, Banci, The human iron-proteome, Metallomics
Banerjee, Dynamics of the COVID-19 pandemic: nonlinear approaches on the modelling, prediction and control, European Phys J Special Topics
Bennouar, Cherif, Kessira, Bennouar, Abdi, Vitamin D deficiency and low serum calcium as predictors of poor prognosis in patients with severe COVID-19, J Am Coll Nutr
Bilal, Dambaeva, Kwak-Kim, Gilman-Sachs, Beaman, A role for iodide and thyroglobulin in modulating the function of human immune cells, Front Immunol
Calder, Carr, Gombart, Eggersdorfer, Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections, Nutrients
Cronin, Woolf, Weiss, Penninger, The role of iron regulation in immunometabolism and immune-related disease, Front Mol Biosci
Filippo, Formenti, Rovere-Querini, Carlucci, Conte et al., Hypocalcemia is highly prevalent and predicts hospitalization in patients with COVID-19, Endocrine
Frise, Cheng, Nickol, Curtis, Pollard et al., Clinical iron deficiency disturbs normal human responses to hypoxia, J Clin Investig
Ghayour-Mobarhan, Moohebati, Esmaily, Ebrahimi, Parizadeh et al., Mashhad stroke and heart atherosclerotic disorder (MASHAD) study: design, baseline characteristics and 10-year cardiovascular risk estimation, Int J Public Health
Hafezi, Seifi, Bahari, Mohammadi, Ghasemabadi et al., The association between macronutrient intakes and coronavirus disease 2019 (COVID-19) in an Iranian population: applying a dynamical system model, J Health Popul Nutr
Higgins, Nonlinear systems in medicine, Yale J Biol Med
Jothimani, Kailasam, Danielraj, Nallathambi, Ramachandran et al., COVID-19: Poor outcomes in patients with zinc deficiency, Int J Infect Dis
Jothimani, Kailasam, Danielraj, Nallathambi, Ramachandran et al., COVID-19: poor outcomes in patients with zinc deficiency, Int J Infect Dis
Maggini, Pierre, Calder, Immune function and micronutrient requirements change over the life course, Nutrients
Mahsa, Zahra, Heidarian, Mehrangiz, Majid et al., Validation of a short semi-quantitative food frequency questionnaire for adults: a pilot study, J Nutr Sci Dietetics
Mehri, Ghorbani, Farhadi-Babadi, Rahimi, Barati et al., Risk Factors Associated with Severity and Death from COVID-19 in Iran: A Systematic Review and Meta-Analysis Study, J Intensive Care Med
Ravasco, Aranha, Borralho, Da, Silva et al., Colorectal cancer: can nutrients modulate NF-kappaB and apoptosis?, Clin Nutr
Read, Obeid, Ahlenstiel, Ahlenstiel, The role of zinc in antiviral immunity, Adv Nutr
Schoenenberger, Schmid, Tanase, Beck, Schwaninger, Structural analysis of system dynamics models, Simul Model Pract Theory
Sun, Zhang, Zou, Liu, Li et al., Serum calcium as a biomarker of clinical severity and prognosis in patients with coronavirus disease 2019, Aging
Van Doorn, Yu, Viral respiratory infections. Hunter's tropical medicine and emerging infectious diseases
Venter, Eyerich, Sarin, Klatt, Nutrition and the immune system: a complicated tango, Nutrients
Vogel-González, Talló-Parra, Herrera-Fernández, Pérez-Vilaró, Chillón et al., Low zinc levels at admission associates with poor clinical outcomes in SARS-CoV-2 infection, Nutrients
Walker, Black, Zinc and the risk for infectious disease, Annu Rev Nutr
Willett, Howe, Kushi, Adjustment for total energy intake in epidemiologic studies, Am J Clin Nutr
Willy, Neugebauer, Gerngroß, The Concept of nonlinearity in complex systems, European J Trauma
Wray, Bridwell, Schauer, Shackelford, Bebarta et al., The diamond of death: Hypocalcemia in trauma and resuscitation, Am J Emerg Med
Zhou, Li, Li, The associations of iron related biomarkers with risk, clinical severity and mortality in SARS-CoV-2 patients: a meta-analysis, Nutrients
DOI record:
{
"DOI": "10.1186/s40795-024-00821-5",
"ISSN": [
"2055-0928"
],
"URL": "http://dx.doi.org/10.1186/s40795-024-00821-5",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>The aim of this study was to determine the association between dietary mineral intake and Coronavirus-disease 2019 (COVID-19) infection and its associated hospitalization.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>This cohort study utilized the MASHAD study population, which comprised individuals aged 35–65. Upon recruitment in 2007, dietary intake was documented using a validated 65-item food frequency questionnaire (FFQ). Data on COVID-19 PCR test results was collected from all relevant medical centers in Mashhad between February 2020 and June 2022. The regression model included dietary minerals and employed the backward variable selection method, along with advanced data analysis techniques.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>The final analysis involved 1957 participants, including 193 COVID-19-positive patients. The mean age was 49.71 and 50.28 years in the COVID-19-positive and negative groups, respectively (<jats:italic>p</jats:italic> = 0.12). Dietary intakes of magnesium, iron, and potassium were notably lower in COVID-19-positive patients (<jats:italic>P</jats:italic> < 0.05). Following adjustments for age and sex, dietary iron remained significantly associated with COVID-19 incidence (OR = 0.94, 95% CI: 0.90–0.98). Furthermore, a statistically significant relationship was observed between dietary zinc and hospitalization due to COVID-19 (OR = 0.69, 95% CI: 0.51–0.93). In dynamical system models, intakes of calcium, zinc, and iron below the cut-offs of 1138, 9.7, and 8.17 mg/day, respectively, were linked to an increased risk of COVID-19 incidence.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>Higher dietary iron and zinc intake are associated with decreased risk of COVID-19 infection and hospitalization, respectively.</jats:p>\n </jats:sec>",
"alternative-id": [
"821"
],
"article-number": "42",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "9 February 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "3 January 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "4 March 2024"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "All experiments were performed in accordance with the declaration of Helsinki and Mashhad University of Medical Sciences ethical guidelines and regulations. The research protocol was approved by the School of Medicine, Mashhad University of Medical Sciences, Biomedical Research Ethics Committee (IR.MUMS.MEDICAL.REC.1398.228). All participants signed a written inform consent before participating in the study."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Not applicable."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Seifi",
"given": "Najmeh",
"sequence": "first"
},
{
"affiliation": [],
"family": "Bahari",
"given": "Hossein",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ghiasi Hafezi",
"given": "Somayeh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ghotbani",
"given": "Farzaneh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Afzalinia",
"given": "AhmadReza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ferns",
"given": "Gordon A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Farkhani",
"given": "Ehsan Mosa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ghayour-mobarhan",
"given": "Majid",
"sequence": "additional"
}
],
"container-title": "BMC Nutrition",
"container-title-short": "BMC Nutr",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
3,
4
]
],
"date-time": "2024-03-04T11:01:36Z",
"timestamp": 1709550096000
},
"deposited": {
"date-parts": [
[
2024,
3,
4
]
],
"date-time": "2024-03-04T11:06:31Z",
"timestamp": 1709550391000
},
"indexed": {
"date-parts": [
[
2024,
3,
5
]
],
"date-time": "2024-03-05T00:47:30Z",
"timestamp": 1709599650503
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
3,
4
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
3,
4
]
],
"date-time": "2024-03-04T00:00:00Z",
"timestamp": 1709510400000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
3,
4
]
],
"date-time": "2024-03-04T00:00:00Z",
"timestamp": 1709510400000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s40795-024-00821-5.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s40795-024-00821-5/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s40795-024-00821-5.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2024,
3,
4
]
]
},
"published-online": {
"date-parts": [
[
2024,
3,
4
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "821_CR1",
"unstructured": "WHO COVID-19 Dashboard. Geneva: World Health Organization, 2020. Available online: https://covid19.who.int/."
},
{
"DOI": "10.1038/s41564-020-0695-z",
"author": "The species Severe acute respiratory syndrome-related coronavirus",
"doi-asserted-by": "publisher",
"first-page": "536",
"issue": "4",
"journal-title": "Nat Microbiol",
"key": "821_CR2",
"unstructured": "The species Severe acute respiratory syndrome-related coronavirus. classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–44.",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/B978-0-323-55512-8.00033-8",
"doi-asserted-by": "crossref",
"key": "821_CR3",
"unstructured": "van Doorn HR, Yu H. Viral respiratory infections. Hunter's tropical medicine and emerging infectious diseases: Elsevier; 2020. p. 284–8."
},
{
"DOI": "10.1177/08850666231166344",
"doi-asserted-by": "crossref",
"key": "821_CR4",
"unstructured": "Mehri A, Sotoodeh Ghorbani S, Farhadi-Babadi K, Rahimi E, Barati Z, Taherpour N, et al. Risk Factors Associated with Severity and Death from COVID-19 in Iran: A Systematic Review and Meta-Analysis Study. J Intensive Care Med. 2023:8850666231166344."
},
{
"DOI": "10.3390/nu12041181",
"author": "PC Calder",
"doi-asserted-by": "publisher",
"first-page": "1181",
"issue": "4",
"journal-title": "Nutrients",
"key": "821_CR5",
"unstructured": "Calder PC, Carr AC, Gombart AF, Eggersdorfer M. Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections. Nutrients. 2020;12(4):1181.",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/nu12030818",
"author": "C Venter",
"doi-asserted-by": "publisher",
"first-page": "818",
"issue": "3",
"journal-title": "Nutrients",
"key": "821_CR6",
"unstructured": "Venter C, Eyerich S, Sarin T, Klatt KC. Nutrition and the immune system: a complicated tango. Nutrients. 2020;12(3):818.",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.09.014",
"author": "D Jothimani",
"doi-asserted-by": "publisher",
"first-page": "343",
"journal-title": "Int J Infect Dis",
"key": "821_CR7",
"unstructured": "Jothimani D, Kailasam E, Danielraj S, Nallathambi B, Ramachandran H, Sekar P, et al. COVID-19: poor outcomes in patients with zinc deficiency. Int J Infect Dis. 2020;100:343–9.",
"volume": "100",
"year": "2020"
},
{
"author": "JP Higgins",
"first-page": "247",
"issue": "5–6",
"journal-title": "Yale J Biol Med",
"key": "821_CR8",
"unstructured": "Higgins JP. Nonlinear systems in medicine. Yale J Biol Med. 2002;75(5–6):247.",
"volume": "75",
"year": "2002"
},
{
"DOI": "10.1140/epjs/s11734-022-00724-1",
"author": "S Banerjee",
"doi-asserted-by": "publisher",
"first-page": "3275",
"issue": "18–20",
"journal-title": "European Phys J Special Topics",
"key": "821_CR9",
"unstructured": "Banerjee S. Dynamics of the COVID-19 pandemic: nonlinear approaches on the modelling, prediction and control. European Phys J Special Topics. 2022;231(18–20):3275–80.",
"volume": "231",
"year": "2022"
},
{
"DOI": "10.1007/s00068-003-1248-x",
"author": "C Willy",
"doi-asserted-by": "publisher",
"first-page": "11",
"journal-title": "European J Trauma",
"key": "821_CR10",
"unstructured": "Willy C, Neugebauer EAM, Gerngroß H. The Concept of nonlinearity in complex systems. European J Trauma. 2003;29:11–22.",
"volume": "29",
"year": "2003"
},
{
"DOI": "10.1016/j.simpat.2021.102333",
"author": "L Schoenenberger",
"doi-asserted-by": "publisher",
"first-page": "102333",
"journal-title": "Simul Model Pract Theory",
"key": "821_CR11",
"unstructured": "Schoenenberger L, Schmid A, Tanase R, Beck M, Schwaninger M. Structural analysis of system dynamics models. Simul Model Pract Theory. 2021;110:102333.",
"volume": "110",
"year": "2021"
},
{
"DOI": "10.1007/s00038-015-0679-6",
"author": "M Ghayour-Mobarhan",
"doi-asserted-by": "publisher",
"first-page": "561",
"issue": "5",
"journal-title": "Int J Public Health",
"key": "821_CR12",
"unstructured": "Ghayour-Mobarhan M, Moohebati M, Esmaily H, Ebrahimi M, Parizadeh SMR, Heidari-Bakavoli AR, et al. Mashhad stroke and heart atherosclerotic disorder (MASHAD) study: design, baseline characteristics and 10-year cardiovascular risk estimation. Int J Public Health. 2015;60(5):561–72.",
"volume": "60",
"year": "2015"
},
{
"DOI": "10.1186/s41043-023-00448-5",
"author": "SG Hafezi",
"doi-asserted-by": "publisher",
"first-page": "114",
"issue": "1",
"journal-title": "J Health Popul Nutr",
"key": "821_CR13",
"unstructured": "Hafezi SG, Seifi N, Bahari H, Mohammadi M, Ghasemabadi A, Ferns GA, et al. The association between macronutrient intakes and coronavirus disease 2019 (COVID-19) in an Iranian population: applying a dynamical system model. J Health Popul Nutr. 2023;42(1):114.",
"volume": "42",
"year": "2023"
},
{
"author": "A Mahsa",
"first-page": "49",
"issue": "2",
"journal-title": "J Nutr Sci Dietetics",
"key": "821_CR14",
"unstructured": "Mahsa A, Zahra A, Hamid Heidarian M, Mehrangiz E-M, Majid G-M, Gorden F. Validation of a short semi-quantitative food frequency questionnaire for adults: a pilot study. J Nutr Sci Dietetics. 2017;3(2):49–55.",
"volume": "3",
"year": "2017"
},
{
"DOI": "10.1016/j.clnu.2009.06.006",
"author": "P Ravasco",
"doi-asserted-by": "publisher",
"first-page": "42",
"issue": "1",
"journal-title": "Clin Nutr",
"key": "821_CR15",
"unstructured": "Ravasco P, Aranha MM, Borralho PM, da Moreira Silva IB, Correia L, Fernandes A, et al. Colorectal cancer: can nutrients modulate NF-kappaB and apoptosis? Clin Nutr. 2010;29(1):42–6.",
"volume": "29",
"year": "2010"
},
{
"DOI": "10.1093/ajcn/65.4.1220S",
"author": "WC Willett",
"doi-asserted-by": "publisher",
"first-page": "S1220",
"issue": "4",
"journal-title": "Am J Clin Nutr",
"key": "821_CR16",
"unstructured": "Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65(4):S1220–8.",
"volume": "65",
"year": "1997"
},
{
"DOI": "10.3390/nu10101531",
"author": "S Maggini",
"doi-asserted-by": "publisher",
"first-page": "1531",
"issue": "10",
"journal-title": "Nutrients",
"key": "821_CR17",
"unstructured": "Maggini S, Pierre A, Calder PC. Immune function and micronutrient requirements change over the life course. Nutrients. 2018;10(10):1531.",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1039/c8mt00146d",
"author": "C Andreini",
"doi-asserted-by": "publisher",
"first-page": "1223",
"journal-title": "Metallomics",
"key": "821_CR18",
"unstructured": "Andreini C, Putignano V, Rosato A, Banci L. The human iron-proteome. Metallomics. 2018;10:1223–31.",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.3389/fmolb.2019.00116",
"author": "SJ Cronin",
"doi-asserted-by": "publisher",
"first-page": "116",
"journal-title": "Front Mol Biosci",
"key": "821_CR19",
"unstructured": "Cronin SJ, Woolf CJ, Weiss G, Penninger JM. The role of iron regulation in immunometabolism and immune-related disease. Front Mol Biosci. 2019;6:116.",
"volume": "6",
"year": "2019"
},
{
"DOI": "10.1172/JCI85715",
"author": "MC Frise",
"doi-asserted-by": "publisher",
"first-page": "2139",
"issue": "6",
"journal-title": "J Clin Investig",
"key": "821_CR20",
"unstructured": "Frise MC, Cheng H-Y, Nickol AH, Curtis MK, Pollard KA, Roberts DJ, et al. Clinical iron deficiency disturbs normal human responses to hypoxia. J Clin Investig. 2016;126(6):2139–50.",
"volume": "126",
"year": "2016"
},
{
"DOI": "10.3390/nu14163406",
"author": "S Zhou",
"doi-asserted-by": "publisher",
"first-page": "3406",
"issue": "16",
"journal-title": "Nutrients",
"key": "821_CR21",
"unstructured": "Zhou S, Li H, Li S. The associations of iron related biomarkers with risk, clinical severity and mortality in SARS-CoV-2 patients: a meta-analysis. Nutrients. 2022;14(16):3406.",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1093/advances/nmz013",
"author": "SA Read",
"doi-asserted-by": "publisher",
"first-page": "696",
"issue": "4",
"journal-title": "Adv Nutr",
"key": "821_CR22",
"unstructured": "Read SA, Obeid S, Ahlenstiel C, Ahlenstiel G. The role of zinc in antiviral immunity. Adv Nutr. 2019;10(4):696–710.",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1146/annurev.nutr.23.011702.073054",
"author": "CF Walker",
"doi-asserted-by": "publisher",
"first-page": "255",
"issue": "1",
"journal-title": "Annu Rev Nutr",
"key": "821_CR23",
"unstructured": "Walker CF, Black RE. Zinc and the risk for infectious disease. Annu Rev Nutr. 2004;24(1):255–75.",
"volume": "24",
"year": "2004"
},
{
"DOI": "10.3390/nu13020562",
"author": "M Vogel-González",
"doi-asserted-by": "publisher",
"first-page": "562",
"issue": "2",
"journal-title": "Nutrients",
"key": "821_CR24",
"unstructured": "Vogel-González M, Talló-Parra M, Herrera-Fernández V, Pérez-Vilaró G, Chillón M, Nogués X, et al. Low zinc levels at admission associates with poor clinical outcomes in SARS-CoV-2 infection. Nutrients. 2021;13(2):562.",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.09.014",
"author": "D Jothimani",
"doi-asserted-by": "publisher",
"first-page": "343",
"journal-title": "Int J Infect Dis",
"key": "821_CR25",
"unstructured": "Jothimani D, Kailasam E, Danielraj S, Nallathambi B, Ramachandran H, Sekar P, et al. COVID-19: Poor outcomes in patients with zinc deficiency. Int J Infect Dis. 2020;100:343–9.",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.18632/aging.103526",
"author": "J-K Sun",
"doi-asserted-by": "publisher",
"first-page": "11287",
"issue": "12",
"journal-title": "Aging (Albany NY)",
"key": "821_CR26",
"unstructured": "Sun J-K, Zhang W-H, Zou L, Liu Y, Li J-J, Kan X-H, et al. Serum calcium as a biomarker of clinical severity and prognosis in patients with coronavirus disease 2019. Aging (Albany NY). 2020;12(12):11287.",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1007/s12020-020-02383-5",
"author": "L Di Filippo",
"doi-asserted-by": "publisher",
"first-page": "475",
"issue": "3",
"journal-title": "Endocrine",
"key": "821_CR27",
"unstructured": "Di Filippo L, Formenti AM, Rovere-Querini P, Carlucci M, Conte C, Ciceri F, et al. Hypocalcemia is highly prevalent and predicts hospitalization in patients with COVID-19. Endocrine. 2020;68(3):475–8.",
"volume": "68",
"year": "2020"
},
{
"DOI": "10.1016/j.ajem.2020.12.065",
"author": "JP Wray",
"doi-asserted-by": "publisher",
"first-page": "104",
"journal-title": "Am J Emerg Med",
"key": "821_CR28",
"unstructured": "Wray JP, Bridwell RE, Schauer SG, Shackelford SA, Bebarta VS, Wright FL, et al. The diamond of death: Hypocalcemia in trauma and resuscitation. Am J Emerg Med. 2021;41:104–9.",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1080/07315724.2020.1856013",
"author": "S Bennouar",
"doi-asserted-by": "publisher",
"first-page": "104",
"issue": "2",
"journal-title": "J Am Coll Nutr",
"key": "821_CR29",
"unstructured": "Bennouar S, Cherif AB, Kessira A, Bennouar D-E, Abdi S. Vitamin D deficiency and low serum calcium as predictors of poor prognosis in patients with severe COVID-19. J Am Coll Nutr. 2021;40(2):104–10.",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1007/s12603-020-1512-3",
"author": "DM Abdulah",
"doi-asserted-by": "publisher",
"first-page": "1011",
"issue": "9",
"journal-title": "J Nutr Health Aging",
"key": "821_CR30",
"unstructured": "Abdulah DM, Hassan A. Relation of dietary factors with infection and mortality rates of COVID-19 across the world. J Nutr Health Aging. 2020;24(9):1011–8.",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2017.01573",
"author": "MY Bilal",
"doi-asserted-by": "publisher",
"first-page": "1573",
"journal-title": "Front Immunol",
"key": "821_CR31",
"unstructured": "Bilal MY, Dambaeva S, Kwak-Kim J, Gilman-Sachs A, Beaman KD. A role for iodide and thyroglobulin in modulating the function of human immune cells. Front Immunol. 2017;8:1573.",
"volume": "8",
"year": "2017"
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-024-00821-5"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health",
"Nutrition and Dietetics",
"Endocrinology, Diabetes and Metabolism",
"Medicine (miscellaneous)"
],
"subtitle": [],
"title": "Dietary mineral intakes predict Coronavirus-disease 2019 (COVID-19) incidence and hospitalization in older adults",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "10"
}