Association of Vitamin D Status and COVID-19-Related Hospitalization and Mortality
et al., Journal of General Internal Medicine, doi:10.1007/s11606-021-07170-0, Jan 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
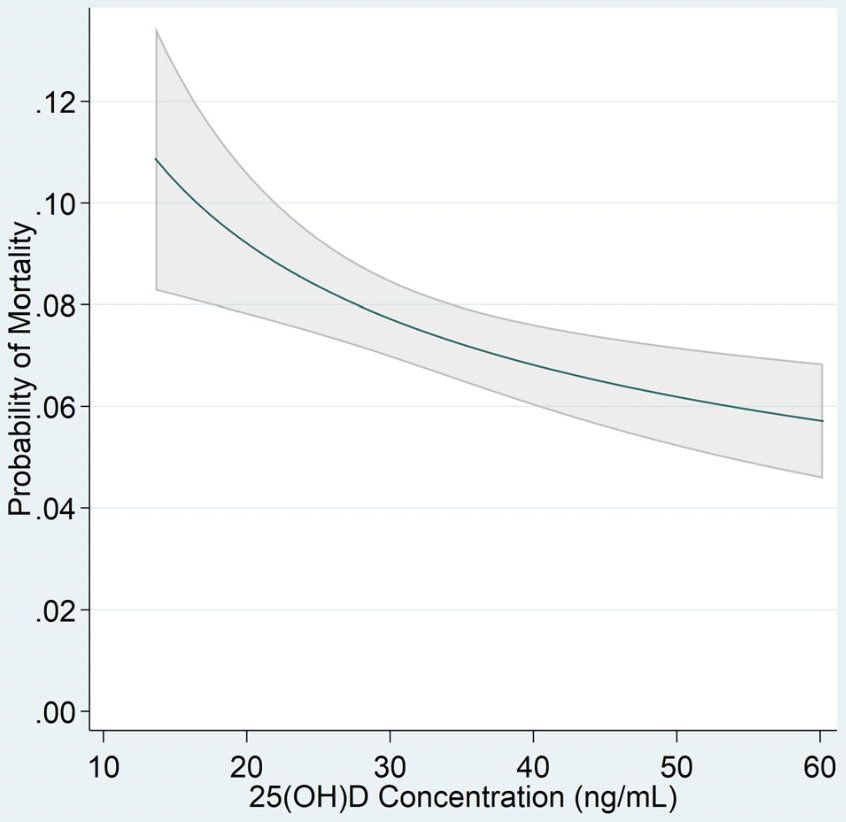
Retrospective 4,599 COVID+ veterans in the USA with vitamin D levels measured 15 to 90 days prior to testing positive, showing a significant independent inverse dose-response relationship between vitamin D levels (from 15 to 60ng/mL) and decreasing risk of hospitalization (24.1% to 18.7%, p = 0.009) and mortality (10.4% to 5.7%, p = 0.001).
This is the 112th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 45.1% lower, RR 0.55, p = 0.001, adjusted per study, inverted to make RR<1 favor high D levels, 60ng/mL vs. 15 ng/mL.
|
|
risk of death, 40.5% lower, RR 0.60, p = 0.001, adjusted per study, inverted to make RR<1 favor high D levels, 50ng/mL vs. 15 ng/mL.
|
|
risk of death, 34.6% lower, RR 0.65, p = 0.001, adjusted per study, inverted to make RR<1 favor high D levels, 40ng/mL vs. 15 ng/mL.
|
|
risk of death, 25.9% lower, RR 0.74, p = 0.001, adjusted per study, inverted to make RR<1 favor high D levels, 30ng/mL vs. 15 ng/mL.
|
|
risk of death, 20.0% lower, RR 0.80, p = 0.001, adjusted per study, inverted to make RR<1 favor high D levels, 25ng/mL vs. 15 ng/mL.
|
|
risk of death, 11.5% lower, RR 0.88, p = 0.001, adjusted per study, inverted to make RR<1 favor high D levels, 20ng/mL vs. 15 ng/mL.
|
|
risk of hospitalization, 22.5% lower, RR 0.78, p = 0.01, adjusted per study, inverted to make RR<1 favor high D levels, 60ng/mL vs. 15 ng/mL.
|
|
risk of hospitalization, 20.0% lower, RR 0.80, p = 0.009, adjusted per study, inverted to make RR<1 favor high D levels, 50ng/mL vs. 15 ng/mL.
|
|
risk of hospitalization, 16.7% lower, RR 0.83, p = 0.007, adjusted per study, inverted to make RR<1 favor high D levels, 40ng/mL vs. 15 ng/mL.
|
|
risk of hospitalization, 12.3% lower, RR 0.88, p = 0.008, adjusted per study, inverted to make RR<1 favor high D levels, 30ng/mL vs. 15 ng/mL.
|
|
risk of hospitalization, 9.1% lower, RR 0.91, p = 0.01, adjusted per study, inverted to make RR<1 favor high D levels, 25ng/mL vs. 15 ng/mL.
|
|
risk of hospitalization, 4.8% lower, RR 0.95, p = 0.02, adjusted per study, inverted to make RR<1 favor high D levels, 20ng/mL vs. 15 ng/mL.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Seal et al., 1 Jan 2022, retrospective, USA, peer-reviewed, 6 authors.
Association of Vitamin D Status and COVID-19-Related Hospitalization and Mortality
Journal of General Internal Medicine, doi:10.1007/s11606-021-07170-0
BACKGROUND: The relationship between vitamin D status and COVID-19-related clinical outcomes is controversial. Prior studies have been conducted in smaller, singlesite, or homogeneous populations limiting adjustments for social determinants of health (race/ethnicity and poverty) common to both vitamin D deficiency and COVID-19 outcomes. OBJECTIVE: To evaluate the dose-response relationship between continuous 25(OH)D and risk for COVID-19related hospitalization and mortality after adjusting for covariates associated with both vitamin D deficiency and COVID-19 outcomes. DESIGN: Retrospective cohort study. PATIENTS: Veteran patients receiving care in US Department of Veteran Affairs (VA) health care facilities with a positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) test and a blood 25(OH)D test between February 20, 2020, and November 8, 2020, followed for up to 60 days. MAIN MEASURES: Exposure was blood 25(OH)D concentration ascertained closest to and within 15 to 90 days preceding an index positive SARS-CoV-2 test. Co-primary study outcomes were COVID-19-related inpatient hospitalization requiring airborne, droplet, contact, or other isolation and mortality ascertained within 60 days of an index positive SARS-CoV-2 test. KEY RESULTS: Of 4,599 veterans with a positive SARS-CoV-2 test, vitamin D deficiency (< 20 ng/mL) was identified in 665 (14.5%); 964 (21.0%) were hospitalized; and 340 (7.4%) died. After adjusting for all covariates, including race/ethnicity and poverty, there was a significant independent inverse dose-response relationship between increasing continuous 25(OH)D concentrations (from 15 to 60 ng/mL) and decreasing probability of COVID-19related hospitalization (from 24.1 to 18.7%, p=0.009) and mortality (from 10.4 to 5.7%, p=0.001). In modeling 25(OH)D as a log-transformed continuous variable, the greatest risk for hospitalization and death was observed at lower 25(OH)D concentrations. CONCLUSIONS: Continuous blood 25(OH)D concentrations are independently associated with COVID-19related hospitalization and mortality in an inverse doseresponse relationship in this large racially and ethnically diverse cohort of VA patients. Randomized controlled trials are needed to evaluate the impact of vitamin D supplementation on COVID-19-related outcomes.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s11606-021-07170-0.
References
Angelidi, Belanger, Lorinsky, Vitamin D Status Is Associated With In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients, Mayo Clin Proc
Bikle, Schwartz, Vitamin D Binding Protein, Total and Free Vitamin D Levels in Different Physiological and Pathophysiological Conditions, Frontiers in Endocrinology
Bikle, Vitamin D and cancer: the promise not yet fulfilled, Endocrine
Bilezikian, Bikle, Hewison, MECHANISMS IN ENDOCRI-NOLOGY: Vitamin D and COVID-19, Eur J Endocrinol
Binkley, Carter, Toward Clarity in Clinical Vitamin D Status Assessment: 25(OH)D Assay Standardization, Endocrinol Metab Clin North Am
Boccardi, Lapenna, Gaggi, A Disease Marker in Hospitalized Very Old Persons at Risk of Malnutrition, Nutrients
Burstrom, Tao, Social determinants of health and inequalities in COVID-19, Eur J Public Health
Castillo, Costa, Barrios, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J Steroid Biochem Mol Biol
Census, Bureau, American Community Survey
Cummings, Estimating Adjusted Risk Ratios for Matched and Unmatched Data: An Update, The Stata Journal
Dawson-Hughes, Mithal, Bonjour, IOF position statement: vitamin D recommendations for older adults, Osteoporos Int
Deluccia, Clegg, Sukumar, The implications of vitamin D deficiency on COVID-19 for at-risk populations, Nutr Rev
Emanuel, Luna, Schaefer, Tan, Wolff, Enhancing the WHO's Proposed Framework for Distributing COVID-19 Vaccines Among Countries, Am J Public Health
Emanuel, Persad, Kern, An ethical framework for global vaccine allocation, Science
Forrest, Stuhldreher, Prevalence and correlates of vitamin D deficiency in US adults, Nutr Res
Gandhi, Lynch, Rio, Mild or Moderate Covid-19, N Engl J Med
Gerberding, Measuring Pandemic Impact: Vital Signs From Vital Statistics, Ann Intern Med
Hamilton, Edelman, Weinberger, Jackson, Concordance between self-reportedrace/ethnicity and that recorded in a Veteran Affairs electronic medical record, N C Med J
Holick, Binkley, Bischoff-Ferrari, Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline, J Clin Endocrinol Metab
Hooper, Napoles, Perez-Stable, COVID-19 and Racial/ Ethnic Disparities, JAMA
Karahan, Katkat, Impact of Serum Vitamin D Level on in Patients with COVID-19 in Turkey, J Nutr Health Aging
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One
Kressin, Chang, Hendricks, Kazis, Agreement between administrative data and patients' self-reports of race/ethnicity, Am J Public Health
Lopez, Hart, Katz, Racial and Ethnic Health Disparities Related to COVID-19, JAMA
Mackey, Ayers, Kondo, Racial and Ethnic Disparities in COVID-19-Related Infections, Hospitalizations, and Deaths : A Systematic Review, Ann Intern Med
Maclaughlin, Holick, Aging decreases the capacity of human skin to produce vitamin D3, J Clin Invest
Mccabe, Hammershaimb, Cheng, Unraveling Attributes of COVID-19 Vaccine Hesitancy in the U.S.: A Large Nationwide Study
Mehta, Mcauley, Brown, COVID-19: consider cytokine s t o r m s y n d r o m e s a n d i m m u n o s u p p r e s s i o n . L a n c e t
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results, JAMA Netw Open
Merzon, Tworowski, Gorohovski, Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J
Mithal, Wahl, Bonjour, Global vitamin D status and determinants of hypovitaminosis D, Osteoporos Int
Murai, Fernandes, Sales, Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Se v e re C OV ID -1 9: A R a nd om i z e d C l i ni c a l Tr i a l, J A M A
Palacios, Gonzalez, Is vitamin D deficiency a major global public health problem?, J Steroid Biochem Mol Biol
Peterson, Anderson, Boundy, Ferguson, Mccleery et al., Mortality Disparities in Racial/Ethnic Minority Groups in the Veterans Health Administration: An Evidence Review and Map, Am J Public Health
Pittas, Jorde, Kawahara, Hughes, Vitamin D Supplementation for Prevention of Type 2 Diabetes Mellitus: To D or Not to D?, J Clin Endocrinol Metab
Rastogi, Bhansali, Khare, Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study), Postgrad Med J
Rhodes, Subramanian, Laird, Griffin, Kenny, Perspective: Vitamin D deficiency and COVID-19 severity -plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, J Intern Med
Saha, Freeman, Toure, Tippens, Weeks, Racial and ethnic disparities in the VA health care system: a systematic review, J Gen Intern Med
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality, Am J Clin Pathol
Thebault, Are we entering a 'fourth wave' of the pandemic? Experts disagree
Thienpont, Stepman, Vesper, Standardization of measurements of 25-hydroxyvitamin D3 and D2, Scand J Clin Lab Invest Suppl
Thompson, Burgess, Naleway, Interim Estimates of Vaccine Effectiveness of BNT162b2 and mRNA-1273 COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Health Care Personnel, First Responders, and Other Essential and Frontline Workers -Eight U.S. Locations, MMWR Morb Mortal Wkly Rep
Waldron, Ashby, Cornes, Vitamin D: a negative acute phase reactant, J Clin Pathol
Webb, Kline, Holick, Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin, J Clin Endocrinol Metab
Yetley, Assessing the vitamin D status of the US population, Am J Clin Nutr
Young, Morgan, Ho, Melanin has a Small Inhibitory Effect on Cutaneous Vitamin D Synthesis: A Comparison of Extreme Phenotypes, J Invest Dermatol
Zittermann, Pilz, Vitamin D and Cardiovascular Disease: An Update, Anticancer Res
Zou, A modified poisson regression approach to prospective studies with binary data, Am J Epidemiol
DOI record:
{
"DOI": "10.1007/s11606-021-07170-0",
"ISSN": [
"0884-8734",
"1525-1497"
],
"URL": "http://dx.doi.org/10.1007/s11606-021-07170-0",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>The relationship between vitamin D status and COVID-19-related clinical outcomes is controversial. Prior studies have been conducted in smaller, single-site, or homogeneous populations limiting adjustments for social determinants of health (race/ethnicity and poverty) common to both vitamin D deficiency and COVID-19 outcomes.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Objective</jats:title>\n <jats:p>To evaluate the dose-response relationship between continuous 25(OH)D and risk for COVID-19-related hospitalization and mortality after adjusting for covariates associated with both vitamin D deficiency and COVID-19 outcomes.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Design</jats:title>\n <jats:p>Retrospective cohort study.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Patients</jats:title>\n <jats:p>Veteran patients receiving care in US Department of Veteran Affairs (VA) health care facilities with a positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) test and a blood 25(OH)D test between February 20, 2020, and November 8, 2020, followed for up to 60 days.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Main Measures</jats:title>\n <jats:p>Exposure was blood 25(OH)D concentration ascertained closest to and within 15 to 90 days preceding an index positive SARS-CoV-2 test. Co-primary study outcomes were COVID-19-related inpatient hospitalization requiring airborne, droplet, contact, or other isolation and mortality ascertained within 60 days of an index positive SARS-CoV-2 test.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Key Results</jats:title>\n <jats:p>Of 4,599 veterans with a positive SARS-CoV-2 test, vitamin D deficiency (< 20 ng/mL) was identified in 665 (14.5%); 964 (21.0%) were hospitalized; and 340 (7.4%) died. After adjusting for all covariates, including race/ethnicity and poverty, there was a significant independent inverse dose-response relationship between increasing continuous 25(OH)D concentrations (from 15 to 60 ng/mL) and decreasing probability of COVID-19-related hospitalization (from 24.1 to 18.7%, <jats:italic>p</jats:italic>=0.009) and mortality (from 10.4 to 5.7%, <jats:italic>p</jats:italic>=0.001). In modeling 25(OH)D as a log-transformed continuous variable, the greatest risk for hospitalization and death was observed at lower 25(OH)D concentrations.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>Continuous blood 25(OH)D concentrations are independently associated with COVID-19-related hospitalization and mortality in an inverse dose-response relationship in this large racially and ethnically diverse cohort of VA patients. Randomized controlled trials are needed to evaluate the impact of vitamin D supplementation on COVID-19-related outcomes.</jats:p>\n </jats:sec>",
"alternative-id": [
"7170"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "9 June 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "24 September 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "1 January 2022"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-6676-9117",
"affiliation": [],
"authenticated-orcid": false,
"family": "Seal",
"given": "Karen H.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Bertenthal",
"given": "Daniel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Carey",
"given": "Evan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Grunfeld",
"given": "Carl",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bikle",
"given": "Daniel D.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lu",
"given": "Chuanyi M.",
"sequence": "additional"
}
],
"container-title": [
"Journal of General Internal Medicine"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
1,
4
]
],
"date-time": "2022-01-04T01:02:27Z",
"timestamp": 1641258147000
},
"deposited": {
"date-parts": [
[
2022,
1,
4
]
],
"date-time": "2022-01-04T01:13:18Z",
"timestamp": 1641258798000
},
"funder": [
{
"DOI": "10.13039/100008460",
"award": [
"UG3AT009765",
"UH3AT009765"
],
"doi-asserted-by": "publisher",
"name": "National Center for Complementary and Integrative Health"
},
{
"DOI": "10.13039/100000063",
"award": [
"Administrative Supplement"
],
"doi-asserted-by": "publisher",
"name": "Office of Dietary Supplements"
},
{
"DOI": "10.13039/100000002",
"award": [
"U24AT009769"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
}
],
"indexed": {
"date-parts": [
[
2022,
1,
4
]
],
"date-time": "2022-01-04T06:11:34Z",
"timestamp": 1641276694349
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0884-8734"
},
{
"type": "electronic",
"value": "1525-1497"
}
],
"issued": {
"date-parts": [
[
2022,
1,
1
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
1
]
],
"date-time": "2022-01-01T00:00:00Z",
"timestamp": 1640995200000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
1
]
],
"date-time": "2022-01-01T00:00:00Z",
"timestamp": 1640995200000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11606-021-07170-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s11606-021-07170-0/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11606-021-07170-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2022,
1,
1
]
]
},
"published-online": {
"date-parts": [
[
2022,
1,
1
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "7170_CR1",
"unstructured": "United Nations Development Program (UNDP). Coronavirus disease COVID-19 pandemic"
},
{
"DOI": "10.7326/M20-6348",
"author": "JL Gerberding",
"doi-asserted-by": "publisher",
"first-page": "1022",
"issue": "12",
"journal-title": "Ann Intern Med.",
"key": "7170_CR2",
"unstructured": "Gerberding JL. Measuring Pandemic Impact: Vital Signs From Vital Statistics. Ann Intern Med. 2020;173(12):1022-1023.",
"volume": "173",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm7013e3",
"doi-asserted-by": "crossref",
"key": "7170_CR3",
"unstructured": "Thompson, MG, Burgess JL, Naleway AL, al. e. Interim Estimates of Vaccine Effectiveness of BNT162b2 and mRNA-1273 COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Health Care Personnel, First Responders, and Other Essential and Frontline Workers — Eight U.S. Locations, December 2020–March 2021. MMWR Morb Mortal Wkly Rep 2021. 2021;70:495-500."
},
{
"DOI": "10.1101/2021.04.05.21254918",
"doi-asserted-by": "crossref",
"key": "7170_CR4",
"unstructured": "McCabe SD, Hammershaimb EA, Cheng D, et al. Unraveling Attributes of COVID-19 Vaccine Hesitancy in the U.S.: A Large Nationwide Study. medRxiv. 2021."
},
{
"DOI": "10.2105/AJPH.2020.306098",
"author": "EJ Emanuel",
"doi-asserted-by": "publisher",
"first-page": "371",
"issue": "3",
"journal-title": "Am J Public Health.",
"key": "7170_CR5",
"unstructured": "Emanuel EJ, Luna F, Schaefer GO, Tan KC, Wolff J. Enhancing the WHO’s Proposed Framework for Distributing COVID-19 Vaccines Among Countries. Am J Public Health. 2021;111(3):371-373.",
"volume": "111",
"year": "2021"
},
{
"DOI": "10.1126/science.abe2803",
"author": "EJ Emanuel",
"doi-asserted-by": "publisher",
"first-page": "1309",
"issue": "6509",
"journal-title": "Science.",
"key": "7170_CR6",
"unstructured": "Emanuel EJ, Persad G, Kern A, et al. An ethical framework for global vaccine allocation. Science. 2020;369(6509):1309-1312.",
"volume": "369",
"year": "2020"
},
{
"key": "7170_CR7",
"unstructured": "Thebault R. Are we entering a ‘fourth wave’ of the pandemic? Experts disagree. Washington Post2021."
},
{
"DOI": "10.7326/M20-6306",
"author": "K Mackey",
"doi-asserted-by": "publisher",
"first-page": "362",
"issue": "3",
"journal-title": "Ann Intern Med.",
"key": "7170_CR8",
"unstructured": "Mackey K, Ayers CK, Kondo KK, et al. Racial and Ethnic Disparities in COVID-19-Related Infections, Hospitalizations, and Deaths : A Systematic Review. Ann Intern Med. 2021;174(3):362-373.",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.8598",
"author": "M Webb Hooper",
"doi-asserted-by": "publisher",
"first-page": "2466",
"issue": "24",
"journal-title": "JAMA.",
"key": "7170_CR9",
"unstructured": "Webb Hooper M, Napoles AM, Perez-Stable EJ. COVID-19 and Racial/Ethnic Disparities. JAMA. 2020;323(24):2466-2467.",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1007/s00198-010-1285-3",
"author": "B Dawson-Hughes",
"doi-asserted-by": "publisher",
"first-page": "1151",
"issue": "7",
"journal-title": "Osteoporos Int.",
"key": "7170_CR10",
"unstructured": "Dawson-Hughes B, Mithal A, Bonjour JP, et al. IOF position statement: vitamin D recommendations for older adults. Osteoporos Int. 2010;21(7):1151-1154.",
"volume": "21",
"year": "2010"
},
{
"key": "7170_CR11",
"unstructured": "Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, D.C.2011."
},
{
"DOI": "10.1007/s00198-009-0954-6",
"author": "A Mithal",
"doi-asserted-by": "publisher",
"first-page": "1807",
"issue": "11",
"journal-title": "Osteoporos Int.",
"key": "7170_CR12",
"unstructured": "Mithal A, Wahl DA, Bonjour JP, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. 2009;20(11):1807-1820.",
"volume": "20",
"year": "2009"
},
{
"DOI": "10.1016/j.jsbmb.2013.11.003",
"author": "C Palacios",
"doi-asserted-by": "publisher",
"first-page": "138",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "7170_CR13",
"unstructured": "Palacios C, Gonzalez L. Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol. 2014;144 Pt A:138-145.",
"volume": "144 Pt A",
"year": "2014"
},
{
"DOI": "10.1172/JCI112134",
"author": "J MacLaughlin",
"doi-asserted-by": "publisher",
"first-page": "1536",
"issue": "4",
"journal-title": "J Clin Invest.",
"key": "7170_CR14",
"unstructured": "MacLaughlin J, Holick MF. Aging decreases the capacity of human skin to produce vitamin D3. J Clin Invest. 1985;76(4):1536-1538.",
"volume": "76",
"year": "1985"
},
{
"DOI": "10.1016/j.nutres.2010.12.001",
"author": "KY Forrest",
"doi-asserted-by": "publisher",
"first-page": "48",
"issue": "1",
"journal-title": "Nutr Res.",
"key": "7170_CR15",
"unstructured": "Forrest KY, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res. 2011;31(1):48-54.",
"volume": "31",
"year": "2011"
},
{
"DOI": "10.1093/ajcn/88.2.558S",
"author": "EA Yetley",
"doi-asserted-by": "publisher",
"first-page": "558S",
"issue": "2",
"journal-title": "Am J Clin Nutr.",
"key": "7170_CR16",
"unstructured": "Yetley EA. Assessing the vitamin D status of the US population. Am J Clin Nutr. 2008;88(2):558S-564S.",
"volume": "88",
"year": "2008"
},
{
"DOI": "10.1210/jcem-67-2-373",
"author": "AR Webb",
"doi-asserted-by": "publisher",
"first-page": "373",
"issue": "2",
"journal-title": "J Clin Endocrinol Metab.",
"key": "7170_CR17",
"unstructured": "Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67(2):373-378.",
"volume": "67",
"year": "1988"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"author": "DO Meltzer",
"doi-asserted-by": "publisher",
"first-page": "e2019722",
"issue": "9",
"journal-title": "JAMA Netw Open.",
"key": "7170_CR18",
"unstructured": "Meltzer DO, Best TJ, Zhang H, Vokes T, Arora V, Solway J. Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results. JAMA Netw Open. 2020;3(9):e2019722.",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1111/febs.15495",
"author": "E Merzon",
"doi-asserted-by": "publisher",
"first-page": "3693",
"issue": "17",
"journal-title": "FEBS J.",
"key": "7170_CR19",
"unstructured": "Merzon E, Tworowski D, Gorohovski A, et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J. 2020;287(17):3693-3702.",
"volume": "287",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239252",
"author": "HW Kaufman",
"doi-asserted-by": "publisher",
"first-page": "e0239252",
"issue": "9",
"journal-title": "PLoS One.",
"key": "7170_CR20",
"unstructured": "Kaufman HW, Niles JK, Kroll MH, Bi C, Holick MF. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One. 2020;15(9):e0239252.",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"author": "D De Smet",
"doi-asserted-by": "publisher",
"first-page": "381",
"issue": "3",
"journal-title": "Am J Clin Pathol.",
"key": "7170_CR21",
"unstructured": "De Smet D, De Smet K, Herroelen P, Gryspeerdt S, Martens GA. Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality. Am J Clin Pathol. 2021;155(3):381-388.",
"volume": "155",
"year": "2021"
},
{
"DOI": "10.1007/s12603-020-1479-0",
"author": "S Karahan",
"doi-asserted-by": "publisher",
"first-page": "189",
"issue": "2",
"journal-title": "J Nutr Health Aging.",
"key": "7170_CR22",
"unstructured": "Karahan S, Katkat F. Impact of Serum 25(OH) Vitamin D Level on Mortality in Patients with COVID-19 in Turkey. J Nutr Health Aging. 2021;25(2):189-196.",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"author": "AM Angelidi",
"doi-asserted-by": "publisher",
"first-page": "875",
"issue": "4",
"journal-title": "Mayo Clin Proc.",
"key": "7170_CR23",
"unstructured": "Angelidi AM, Belanger MJ, Lorinsky MK, et al. Vitamin D Status Is Associated With In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients. Mayo Clin Proc. 2021;96(4):875-886.",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"author": "M Entrenas Castillo",
"doi-asserted-by": "publisher",
"first-page": "105751",
"journal-title": "J Steroid Biochem Mol Biol.",
"key": "7170_CR24",
"unstructured": "Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, et al. \"Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study\". J Steroid Biochem Mol Biol. 2020;203:105751.",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.1136/postgradmedj-2020-139065",
"doi-asserted-by": "crossref",
"key": "7170_CR25",
"unstructured": "Rastogi A, Bhansali A, Khare N, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study). Postgrad Med J. 2020."
},
{
"DOI": "10.1001/jama.2020.26848",
"author": "IH Murai",
"doi-asserted-by": "publisher",
"first-page": "1053",
"issue": "11",
"journal-title": "JAMA.",
"key": "7170_CR26",
"unstructured": "Murai IH, Fernandes AL, Sales LP, et al. Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial. JAMA. 2021;325(11):1053-1060.",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgaa594",
"doi-asserted-by": "crossref",
"key": "7170_CR27",
"unstructured": "Pittas AG, Jorde R, Kawahara T, Dawson-Hughes B. Vitamin D Supplementation for Prevention of Type 2 Diabetes Mellitus: To D or Not to D? J Clin Endocrinol Metab. 2020;105(12)."
},
{
"DOI": "10.21873/anticanres.13643",
"author": "A Zittermann",
"doi-asserted-by": "publisher",
"first-page": "4627",
"issue": "9",
"journal-title": "Anticancer Res.",
"key": "7170_CR28",
"unstructured": "Zittermann A, Pilz S. Vitamin D and Cardiovascular Disease: An Update. Anticancer Res. 2019;39(9):4627-4635.",
"volume": "39",
"year": "2019"
},
{
"DOI": "10.1007/s12020-013-0146-1",
"doi-asserted-by": "crossref",
"key": "7170_CR29",
"unstructured": "Bikle DD. Vitamin D and cancer: the promise not yet fulfilled. Endocrine. 2014;46(1):29-38."
},
{
"DOI": "10.3390/nu11010128",
"doi-asserted-by": "crossref",
"key": "7170_CR30",
"unstructured": "Boccardi V, Lapenna M, Gaggi L, et al. Hypovitaminosis D: A Disease Marker in Hospitalized Very Old Persons at Risk of Malnutrition. Nutrients. 2019;11(1)."
},
{
"DOI": "10.1056/NEJMcp2009249",
"author": "RT Gandhi",
"doi-asserted-by": "publisher",
"first-page": "1757",
"issue": "18",
"journal-title": "N Engl J Med.",
"key": "7170_CR31",
"unstructured": "Gandhi RT, Lynch JB, Del Rio C. Mild or Moderate Covid-19. N Engl J Med. 2020;383(18):1757-1766.",
"volume": "383",
"year": "2020"
},
{
"key": "7170_CR32",
"unstructured": "National Institutes of Health. COVID-19 Treatment Guidelines: Vitamin D. In:July 17, 2020."
},
{
"DOI": "10.1136/jclinpath-2012-201301",
"author": "JL Waldron",
"doi-asserted-by": "publisher",
"first-page": "620",
"issue": "7",
"journal-title": "J Clin Pathol.",
"key": "7170_CR33",
"unstructured": "Waldron JL, Ashby HL, Cornes MP, et al. Vitamin D: a negative acute phase reactant. J Clin Pathol. 2013;66(7):620-622.",
"volume": "66",
"year": "2013"
},
{
"key": "7170_CR34",
"unstructured": "SAS System [computer program]. Version 9.4. Cary, North Carolina, U.S.A.: SAS Institute; 2013."
},
{
"key": "7170_CR35",
"unstructured": "Stata: Release 15 Statistical Software. [computer program]. College Station, Texas, U.S.A.: StataCorp LLC; 2017."
},
{
"author": "LM Thienpont",
"first-page": "41",
"journal-title": "Scand J Clin Lab Invest Suppl.",
"key": "7170_CR36",
"unstructured": "Thienpont LM, Stepman HC, Vesper HW. Standardization of measurements of 25-hydroxyvitamin D3 and D2. Scand J Clin Lab Invest Suppl. 2012;243:41-49.",
"volume": "243",
"year": "2012"
},
{
"DOI": "10.1016/j.ecl.2017.07.012",
"author": "N Binkley",
"doi-asserted-by": "publisher",
"first-page": "885",
"issue": "4",
"journal-title": "Endocrinol Metab Clin North Am.",
"key": "7170_CR37",
"unstructured": "Binkley N, Carter GD. Toward Clarity in Clinical Vitamin D Status Assessment: 25(OH)D Assay Standardization. Endocrinol Metab Clin North Am. 2017;46(4):885-899.",
"volume": "46",
"year": "2017"
},
{
"DOI": "10.1210/jc.2011-0385",
"author": "MF Holick",
"doi-asserted-by": "publisher",
"first-page": "1911",
"issue": "7",
"journal-title": "J Clin Endocrinol Metab.",
"key": "7170_CR38",
"unstructured": "Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-1930.",
"volume": "96",
"year": "2011"
},
{
"key": "7170_CR39",
"unstructured": "U.S. Census Bureau. American Community Survey. American Community Survey 5-Year Estimates. Table 1901. . 2018."
},
{
"DOI": "10.1093/eurpub/ckaa095",
"author": "B Burstrom",
"doi-asserted-by": "publisher",
"first-page": "617",
"issue": "4",
"journal-title": "Eur J Public Health.",
"key": "7170_CR40",
"unstructured": "Burstrom B, Tao W. Social determinants of health and inequalities in COVID-19. Eur J Public Health. 2020;30(4):617-618.",
"volume": "30",
"year": "2020"
},
{
"key": "7170_CR41",
"unstructured": "https://www.research.va.gov/resources/CIPHER.pdf. Accessed."
},
{
"DOI": "10.1093/aje/kwh090",
"author": "G Zou",
"doi-asserted-by": "publisher",
"first-page": "702",
"issue": "7",
"journal-title": "Am J Epidemiol.",
"key": "7170_CR42",
"unstructured": "Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702-706.",
"volume": "159",
"year": "2004"
},
{
"DOI": "10.3389/fendo.2019.00317",
"doi-asserted-by": "crossref",
"key": "7170_CR43",
"unstructured": "Bikle DD, Schwartz J. Vitamin D Binding Protein, Total and Free Vitamin D Levels in Different Physiological and Pathophysiological Conditions. Frontiers in Endocrinology. 2019;10(317)."
},
{
"DOI": "10.1177/1536867X1101100208",
"author": "P Cummings",
"doi-asserted-by": "publisher",
"first-page": "290",
"issue": "2",
"journal-title": "The Stata Journal.",
"key": "7170_CR44",
"unstructured": "Cummings P. Estimating Adjusted Risk Ratios for Matched and Unmatched Data: An Update. The Stata Journal. 2011;11(2):290-298.",
"volume": "11",
"year": "2011"
},
{
"DOI": "10.1530/EJE-20-0665",
"author": "JP Bilezikian",
"doi-asserted-by": "publisher",
"first-page": "R133",
"issue": "5",
"journal-title": "Eur J Endocrinol.",
"key": "7170_CR45",
"unstructured": "Bilezikian JP, Bikle D, Hewison M, et al. MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19. Eur J Endocrinol. 2020;183(5):R133-R147.",
"volume": "183",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"author": "P Mehta",
"doi-asserted-by": "publisher",
"first-page": "1033",
"issue": "10229",
"journal-title": "Lancet.",
"key": "7170_CR46",
"unstructured": "Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-1034.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1111/joim.13149",
"doi-asserted-by": "crossref",
"key": "7170_CR47",
"unstructured": "Rhodes JM, Subramanian S, Laird E, Griffin G, Kenny RA. Perspective: Vitamin D deficiency and COVID-19 severity - plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis. J Intern Med. 2020."
},
{
"DOI": "10.1016/j.jid.2019.11.019",
"author": "AR Young",
"doi-asserted-by": "publisher",
"first-page": "1418",
"issue": "7",
"journal-title": "J Invest Dermatol.",
"key": "7170_CR48",
"unstructured": "Young AR, Morgan KA, Ho TW, et al. Melanin has a Small Inhibitory Effect on Cutaneous Vitamin D Synthesis: A Comparison of Extreme Phenotypes. J Invest Dermatol. 2020;140(7):1418-1426 e1411.",
"volume": "140",
"year": "2020"
},
{
"DOI": "10.1093/nutrit/nuaa092",
"author": "R DeLuccia",
"doi-asserted-by": "publisher",
"first-page": "227",
"issue": "2",
"journal-title": "Nutr Rev.",
"key": "7170_CR49",
"unstructured": "DeLuccia R, Clegg D, Sukumar D. The implications of vitamin D deficiency on COVID-19 for at-risk populations. Nutr Rev. 2021;79(2):227-234.",
"volume": "79",
"year": "2021"
},
{
"DOI": "10.1007/s11606-008-0521-4",
"author": "S Saha",
"doi-asserted-by": "publisher",
"first-page": "654",
"issue": "5",
"journal-title": "J Gen Intern Med.",
"key": "7170_CR50",
"unstructured": "Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J Gen Intern Med. 2008;23(5):654-671.",
"volume": "23",
"year": "2008"
},
{
"DOI": "10.2105/AJPH.2017.304246",
"author": "K Peterson",
"doi-asserted-by": "publisher",
"first-page": "e1",
"issue": "3",
"journal-title": "Am J Public Health.",
"key": "7170_CR51",
"unstructured": "Peterson K, Anderson J, Boundy E, Ferguson L, McCleery E, Waldrip K. Mortality Disparities in Racial/Ethnic Minority Groups in the Veterans Health Administration: An Evidence Review and Map. Am J Public Health. 2018;108(3):e1-e11.",
"volume": "108",
"year": "2018"
},
{
"DOI": "10.1001/jama.2020.26443",
"doi-asserted-by": "crossref",
"key": "7170_CR52",
"unstructured": "Lopez L, Hart LH, Katz MH. Racial and Ethnic Health Disparities Related to COVID-19. JAMA. 2021."
},
{
"DOI": "10.2105/AJPH.93.10.1734",
"author": "NR Kressin",
"doi-asserted-by": "publisher",
"first-page": "1734",
"issue": "10",
"journal-title": "Am J Public Health.",
"key": "7170_CR53",
"unstructured": "Kressin NR, Chang BH, Hendricks A, Kazis LE. Agreement between administrative data and patients’ self-reports of race/ethnicity. Am J Public Health. 2003;93(10):1734-1739.",
"volume": "93",
"year": "2003"
},
{
"author": "NS Hamilton",
"first-page": "296",
"issue": "4",
"journal-title": "N C Med J.",
"key": "7170_CR54",
"unstructured": "Hamilton NS, Edelman D, Weinberger M, Jackson GL. Concordance between self-reportedrace/ethnicity and that recorded in a Veteran Affairs electronic medical record. N C Med J. 2009;70(4):296-300.",
"volume": "70",
"year": "2009"
}
],
"reference-count": 54,
"references-count": 54,
"relation": {},
"score": 1,
"short-container-title": [
"J GEN INTERN MED"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Internal Medicine"
],
"subtitle": [],
"title": [
"Association of Vitamin D Status and COVID-19-Related Hospitalization and Mortality"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}
