The neighborhood built environment and COVID-19 hospitalizations
et al., PLOS ONE, doi:10.1371/journal.pone.0286119, Jun 2023
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
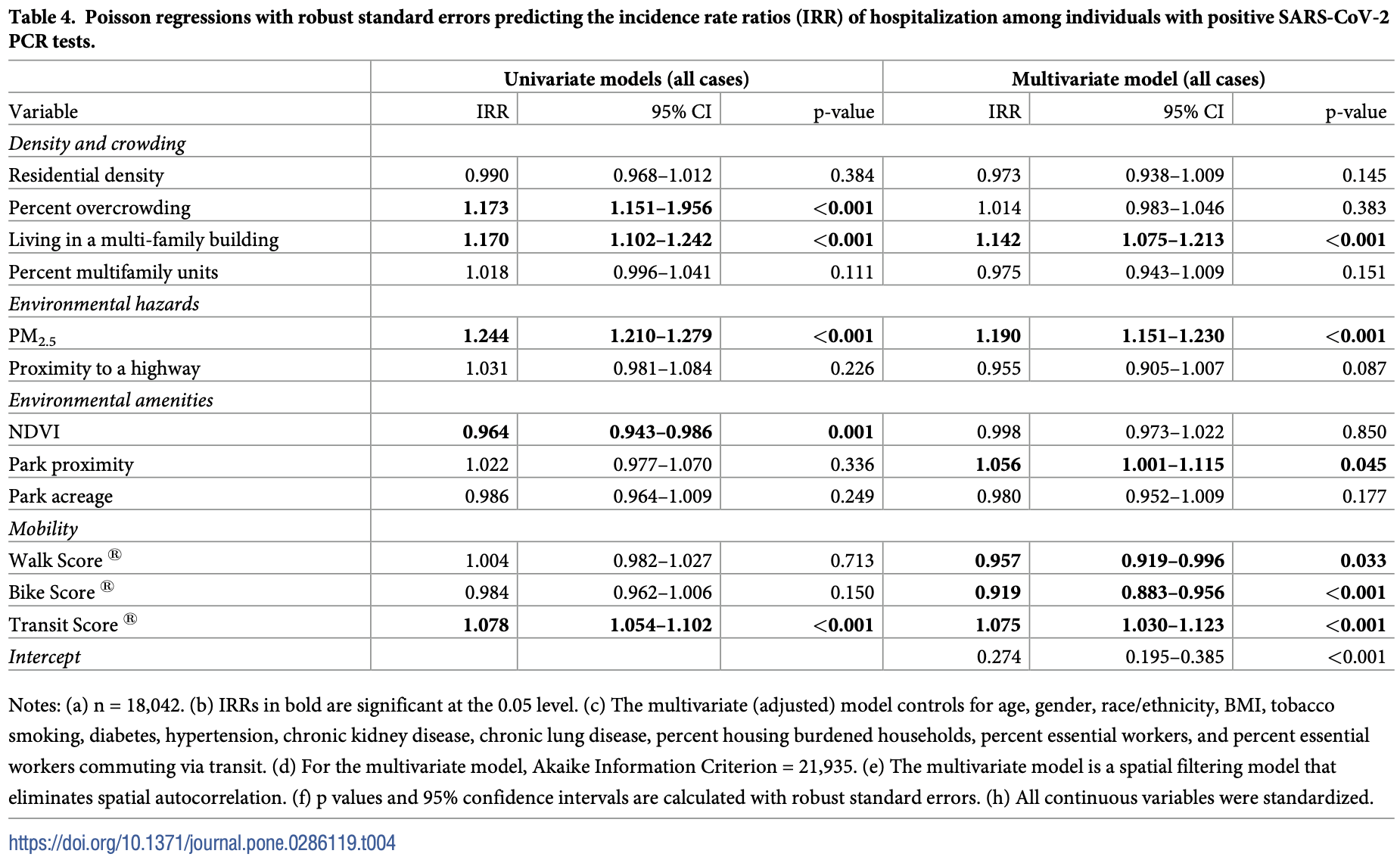
Analysis of neighborhood built environment characteristics in the USA with 18,042 COVID+ individuals, showing lower risk of hospitalization with higher walkability and higher bikeability scores.
Rigolon et al., 14 Jun 2023, retrospective, USA, peer-reviewed, 9 authors, study period 1 May, 2020 - 31 December, 2020.
Contact: alessandro.rigolon@utah.edu, haendel@cuanschutz.edu.
The neighborhood built environment and COVID-19 hospitalizations
PLOS ONE, doi:10.1371/journal.pone.0286119
Research on the associations between the built environment and COVID-19 outcomes has mostly focused on incidence and mortality. Also, few studies on the built environment and COVID-19 have controlled for individual-level characteristics across large samples. In this study, we examine whether neighborhood built environment characteristics are associated with hospitalization in a cohort of 18,042 individuals who tested positive for SARS-CoV-2 between May and December 2020 in the Denver metropolitan area, USA. We use Poisson models with robust standard errors that control for spatial dependence and several individual-level demographic characteristics and comorbidity conditions. In multivariate models, we find that among individuals with SARS-CoV-2 infection, those living in multi-family housing units and/or in places with higher particulate matter (PM 2.5 ) have a higher incident rate ratio (IRR) of hospitalization. We also find that higher walkability, higher bikeability, and lower public transit access are linked to a lower IRR of hospitalization. In multivariate models, we did not find associations between green space measures and the IRR of hospitalization. Results for non-Hispanic white and Latinx individuals highlight substantial differences: higher PM 2.5 levels have stronger positive associations with the IRR of hospitalization for Latinx individuals, and density and overcrowding show stronger associations for non-Hispanic white individuals. Our results show that the neighborhood built environment might pose an independent risk for COVID-19 hospitalization. Our results may inform public health and urban planning initiatives to lower the risk of hospitalization linked to COVID-19 and other respiratory pathogens.
Supporting information
S1 Appendix. (DOCX)
Author Contributions
References
Anguelovski, Triguero-Mas, Connolly, Kotsila, Shokry et al., Gentrification and health in two global cities: A call to identify impacts for socially-vulnerable residents, Cities Heal, doi:10.1080/23748834.2019.1636507
Baden, Sahly, Essink, Kotloff, Frey et al., Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine, N Engl J Med, doi:10.1056/NEJMoa2035389
Barajas, Biking where Black: Connecting transportation planning and infrastructure to disproportionate policing, Transp Res Part D Transp Environ, doi:10.1016/j.trd.2021.103027
Bell, Ebisu, Environmental inequality in exposures to airborne particulate matter components in the United States. Environ Heal Perpsectives, doi:10.1289/ehp.1205201
Boterman, Urban-rural polarisation in times of the Corona outbreak? The early demographic and geographic patterns of the SARS-CoV-2 epidemic in the Netherlands, Tijdschr voor Econ en Soc Geogr, doi:10.1111/tesg.12437
Bowe, Xie, Gibson, Cai, Van Donkelaar et al., Ambient fine particulate matter air pollution and the risk of hospitalization among COVID-19 positive individuals: Cohort study, Environ Int, doi:10.1016/j.envint.2021.106564
Braveman, Cubbin, Egerter, Pedregon, None
Bray, Gibson, White, Coronavirus disease 2019 mortality: A multivariate ecological analysis in relation to ethnicity, population density, obesity, deprivation and pollution, Public Health, doi:10.1016/j.puhe.2020.06.056
Browning, Rigolon, Could nature help children rise out of poverty? Green space and future earnings from a cohort in ten U.S. cities, Environ Res, doi:10.1016/j.envres.2019.04.016
Bryan, Sun, Jagai, Horton, Montgomery et al., Coronavirus disease 2019 (COVID-19) mortality and neighborhood characteristics in Chicago, Ann Epidemiol, doi:10.1016/j.annepidem.2020.10.011
Chakrabarty, Beeler, Liu, Goswami, Harvey et al., Ambient PM2.5 exposure and rapid spread of COVID-19 in the United States, Sci Total Environ, doi:10.1016/j.scitotenv.2020.143391
Chaturvedi, Vishwakarma, Singh, COVID-19 and its impact on education, social life and mental health of students: A survey, Child Youth Serv Rev, doi:10.1016/j.childyouth.2020.105866
Chennakesavulu, Reddy, The effect of latitude and PM2.5 on spreading of SARS-CoV-2 in tropical and temperate zone countries, Environ Pollut, doi:10.1016/j.envpol.2020.115176
Chetty, Hendren, Kline, Saez, Where is the land of opportunity? The geography of intergenerational mobility in the United States, Q J Econ, doi:10.1093/qje/qju022
Choi, Denice, Haan, Zajacova, Studying the social determinants of COVID-19 in a data vacuum, Can Rev Sociol, doi:10.1111/cars.12336
Cohen, Brauer, Burnett, Hr, Frostad et al., Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study, Lancet, doi:10.1016/S0140-6736%2817%2930505-6
Copiello, Grillenzoni, Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China, Zhu et al. Sci Total Environ, doi:10.1016/j.scitotenv.2020.141028
Credit, Neighbourhood inequity: Exploring the factors underlying racial and ethnic disparities in COVID-19 testing and infection rates using ZIP code data in Chicago and New York, Reg Sci Policy Pract, doi:10.1111/rsp3.12321
Denver, Health, Center, None
Desouza, Braun, Parks, Schwartz, Dominici et al., Nationwide study of short-term exposure to fine particulate matter and cardiovascular hospitalizations among medicaid enrollees, Epidemiology, doi:10.1097/EDE.0000000000001265
Dominici, Peng, Bell, Pham, Mcdermott et al., Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases, J Am Med Assoc, doi:10.1001/jama.295.10.1127
Drcog, Parks recreation and open space
Faq, None
Field, Discovering statistics using SPSS
Frontera, Cianfanelli, Vlachos, Landoni, Cremona, Severe air pollution links to higher mortality in COVID-19 patients: The "double-hit" hypothesis, J Infect, doi:10.1016/j.jinf.2020.05.031
Fronza, Lusic, Schmidt, Lucic, Spatial-temporal variations in atmospheric factors contribute to SARS-CoV-2 outbreak, Viruses, doi:10.3390/v12060588
Frumkin, COVID-19, the built environment, and health. Environ Heal Perpsectives, doi:10.1289/EHP8888
Gaitens, Condon, Fernandes, Mcdiarmid, COVID-19 and essential workers: A narrative review of health outcomes and moral injury, Int J Environ Res Public Health, doi:10.3390/ijerph18041446
Glencross, Ho, Camiña, Hawrylowicz, Pfeffer, Air pollution and its effects on the immune system, Free Radic Biol Med, doi:10.1016/j.freeradbiomed.2020.01.179
Goldberg, Security information
Griffith, Spatial autocorrelation and spatial filtering: Gaining understanding through theory and scientific visualization
Hamidi, Sabouri, Ewing, Does density aggravate the COVID-19 pandemic?: Early findings and lessons for Planners, J Am Plan Assoc, doi:10.1080/01944363.2020.1777891
Hendryx, Luo, COVID-19 prevalence and fatality rates in association with air pollution emission concentrations and emission sources, Environ Pollut, doi:10.1016/j.envpol.2020.115126
Hernandez, Denver's population grew by more than 115,000 residents in the last decade
Hu, Chen, Who left riding transit? Examining socioeconomic disparities in the impact of COVID-19 on ridership, Transp Res Part D Transp Environ, doi:10.1016/j.trd.2020.102654
Huang, Kwan, Uncertainties in the assessment of COVID-19 risk: A study of people's exposure to high-risk environments using individual-level activity data, Ann Am Assoc Geogr, doi:10.1080/24694452.2021.1943301
Jackman, Tahk, Zeileis, Maimone, Fearon et al., None
Kim, Garg, 'halloran, Whitaker, Pham et al., Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the US Coronavirus disease 2019 (COVID-19)-Associated hospitalization surveillance network (COVID-NET), Clin Infect Dis, doi:10.1093/cid/ciaa1012
Klompmaker, Hart, Holland, Sabath, Wu et al., County-level exposures to greenness and associations with COVID-19 incidence and mortality in the United States, Environ Res, doi:10.1016/j.envres.2021.111331
Knol, Cessie, Algra, Vandenbroucke, Groenwold, Overestimation of risk ratios by odds ratios in trials and cohort studies: Alternatives to logistic regression, C Can Med Assoc J, doi:10.1503/cmaj.101715
Kodera, Rashed, Hirata, Correlation between COVID-19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity, Int J Environ Res Public Health, doi:10.3390/ijerph17155477
Labib, Browning, Rigolon, Helbich, James, Nature's contributions in coping with a pandemic in the 21st century: A narrative review of evidence during COVID-19, Sci Total Environ, doi:10.1016/j.scitotenv.2022.155095
Lewis, Friedrichs, Wagstaff, Sage, Lacross et al., Disparities in COVID-19 incidence, hospitalizations, and testing, by area-level deprivation, Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6938a4
Lin, Ossola, Alberti, Andersson, Bai et al., Integrating solutions to adapt cities for climate change, Lancet Planet Heal, doi:10.1016/S2542-5196%2821%2900135-2
Liu, Emerging study on the transmission of the Novel Coronavirus (COVID-19) from urban perspective: Evidence from China, Cities, doi:10.1016/j.cities.2020.102759
Liu, Kwan, Integrated analysis of doubly disadvantaged neighborhoods by considering both green space and blue space accessibility and COVID-19 infection risk, PLoS One, doi:10.1371/journal.pone.0273125
Lu, Chen, Liu, Yang, Sullivan et al., Green spaces mitigate racial disparity of health: A higher ratio of green spaces indicates a lower racial disparity in SARS-CoV-2 infection rates in the USA, Environ Int, doi:10.1016/j.envint.2021.106465
Mackey, Ayers, Kondo, Saha, Advani et al., Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review, Ann Intern Med, doi:10.7326/M20-6306
Mahase, Covid-19: What do we know about "long covid, BMJ, doi:10.1136/bmj.m2815
Markevych, Schoierer, Hartig, Chudnovsky, Hystad et al., Exploring pathways linking greenspace to health: Theoretical and methodological guidance, Environ Res, doi:10.1016/j.envres.2017.06.028
Maroko, Nash, Pavilonis, Covid-19 and Inequity: A comparative spatial analysis of New York City and Chicago hot spots, J Urban Heal, doi:10.1007/s11524-020-00468-0
Marquès, Domingo, Positive association between outdoor air pollution and the incidence and severity of COVID-19. A review of the recent scientific evidences, Environ Res, doi:10.1016/j.envres.2021.111930
Mckibbin, Fernando, The economic impact of COVID-19
Megahed, Ghoneim, Antivirus-built environment: Lessons learned from Covid-19 pandemic, Sustain Cities Soc, doi:10.1016/j.scs.2020.102350
Mendy, Wu, Keller, Fassler, Apewokin et al., Long-term exposure to fine particulate matter and hospitalization in COVID-19 patients, Respir Med, doi:10.1016/j.rmed.2021.106313
Nardone, Casey, Morello-Frosch, Mujahid, Balmes et al., Associations between historical residential redlining and current age-adjusted rates of emergency department visits due to asthma across eight cities in California: an ecological study, Lancet Planet Heal, doi:10.1016/S2542-5196%2819%2930241-4
Nardone, Rudolph, Morello-Frosch, Casey, Redlines and greenspace: The Relationship between historical redlining and 2010 greenspace across the United States, Environ Health Perspect, doi:10.1289/EHP7495
Nieuwenhuijsen, Khreis, Integrating human health into urban and transport planning: A framework, doi:10.1007/978-3-319-74983-9
Okoh, Sossou, Dangayach, Meledathu, Phillips et al., Coronavirus disease 19 in minority populations of Newark, New Jersey, Int J Equity Health, doi:10.1186/s12939-020-01208-1
Olusola, Olusola, Onafeso, Ajiola, Adelabu, Early geography of the coronavirus disease outbreak in Nigeria, GeoJournal, doi:10.1007/s10708-020-10278-1
Palm, Allen, Liu, Zhang, Widener et al., Riders who avoided public transit during COVID-19: Personal burdens and implications for social equity, J Am Plan Assoc, doi:10.1080/01944363.2021.1886974
Pandey, Elliott, Suppressor variables in social work research: Ways to identify in multiple regression models, J Soc Social Work Res, doi:10.5243/jsswr.2010.2
Paul, Arif, Pokhrel, Ghosh, The association of social determinants of health with COVID-19 mortality in rural and urban counties, J Rural Heal, doi:10.1111/jrh.12557
Pinheiro, Luı, Nc, COVID-19 could leverage a sustainable built environment, Sustainability, doi:10.3390/su12145863
Polack, Thomas, Kitchin, Absalon, Gurtman et al., Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine, N Engl J Med, doi:10.1056/NEJMoa2034577
Rajagopalan, Landrigan, Pollution and the heart, N Engl J Med, doi:10.1056/NEJMra2030281
Ramı ´rez, Lee, COVID-19 emergence and social and health determinants in Colorado: A rapid spatial analysis, Int J Environ Res Public Health, doi:10.3390/ijerph17113856
Reid, Rieves, Carlson, Perceptions of green space usage, abundance, and quality of green space were associated with better mental health during the COVID-19 pandemic among residents of Denver, PLoS One, doi:10.1371/journal.pone.0263779
Rojas-Rueda, Morales-Zamora, Built environment, transport, and COVID-19: A review, Curr Environ Heal Reports, doi:10.1007/s40572-021-00307-7
Rundle, Bader, Mooney, The disclosure of personally identifiable information in studies of neighborhood contexts and patient outcomes, J Med Internet Res, doi:10.2196/30619
Sallis, Young, Tartof, Sallis, Sall et al., Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Slabaugh, Ne ´meth, Rigolon, Open streets for whom? Toward a just livability revolution, J Am Plan Assoc, doi:10.1080/01944363.2021.1955735
Spotswood, Benjamin, Stoneburner, Wheeler, Beller et al., Nature inequity and higher COVID-19 case rates in less-green neighbourhoods in the United States, Nat Sustain, doi:10.1038/s41893-021-00781-9
Sun, Zhang, Yang, Wan, Wang, Impacts of geographic factors and population density on the COVID-19 spreading under the lockdown policies of China, Sci Total Environ, doi:10.1016/j.scitotenv.2020.141347
Tan S Bin, Desouza, Raifman, Structural racism and COVID-19 in the USA: A county-level empirical analysis, J Racial Ethn Heal Disparities, doi:10.1007/s40615-020-00948-8
Tan S Bin, Desouza, Raifman, Structural racism and COVID-19 in the USA: A county-level empirical analysis. J Racial Ethn Heal Disparities, doi:10.1007/s40615-020-00948-8
Telenti, Arvin, Corey, Corti, Diamond et al., After the pandemic: perspectives on the future trajectory of COVID-19, Nature, doi:10.1038/s41586-021-03792-w
Tessum, Paolella, Chambliss, Apte, Hill et al., PM2.5 polluters disproportionately and systemically affect people of color in the United States, Sci Adv, doi:10.1126/sciadv.abf4491
Tipirneni, Karmakar, Malley, Prescott, Chopra, Contribution of individual-and neighborhood-level social, demographic, and health factors to COVID-19 hospitalization outcomes, Ann Intern Med, doi:10.7326/M21-2615
Tribby, Hartmann, COVID-19 cases and the built environment: Initial evidence from New York City, Prof Geogr, doi:10.1080/00330124.2021.1895851
Walkscore, Walkability, real estate, and public health data
Wang, Piantadosi, Le-Rademacher, Mandrekar, Statistical considerations for subgroup analyses, J Thorac Oncol, doi:10.1016/j.jtho.2020.12.008
Wang, Wu, Wang, He, Li et al., Review of associations between built environment characteristics and severe acute respiratory syndrome coronavirus 2 infection risk, Int J Environ Res Public Health, doi:10.3390/ijerph18147561
Willan, King, Jeffery, Bienz, Challenges for NHS hospitals during COVID-19 epidemic, BMJ, doi:10.1136/bmj.m1117
Xiao, The road to racial justice: Resolving the disproportionate health burden placed on communities of color by highway pollution. Columbia Human Rights Law Rev
You, Pan, Urban vegetation slows down the spread of coronavirus disease (COVID-19) in the United States, Geophys Res Lett, doi:10.1029/2020GL089286
Zhang, Schwartz, Spatial disparities in coronavirus incidence and mortality in the United States: An ecological analysis as of, J Rural Heal, doi:10.1111/jrh.12476
Zhao, Fang, Feng, Fang, He et al., Emerging role of air pollution and meteorological parameters in COVID-19, J Evid Based Med, doi:10.1111/jebm.12430
Zhu, Maharajan, Liu, Zhang, Role of atmospheric particulate matter exposure in COVID-19 and other health risks in human: A review, Environ Res, doi:10.1016/j.envres.2021.111281
DOI record:
{
"DOI": "10.1371/journal.pone.0286119",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0286119",
"abstract": "<jats:p>Research on the associations between the built environment and COVID-19 outcomes has mostly focused on incidence and mortality. Also, few studies on the built environment and COVID-19 have controlled for individual-level characteristics across large samples. In this study, we examine whether neighborhood built environment characteristics are associated with hospitalization in a cohort of 18,042 individuals who tested positive for SARS-CoV-2 between May and December 2020 in the Denver metropolitan area, USA. We use Poisson models with robust standard errors that control for spatial dependence and several individual-level demographic characteristics and comorbidity conditions. In multivariate models, we find that among individuals with SARS-CoV-2 infection, those living in multi-family housing units and/or in places with higher particulate matter (PM<jats:sub>2.5</jats:sub>) have a higher incident rate ratio (IRR) of hospitalization. We also find that higher walkability, higher bikeability, and lower public transit access are linked to a lower IRR of hospitalization. In multivariate models, we did not find associations between green space measures and the IRR of hospitalization. Results for non-Hispanic white and Latinx individuals highlight substantial differences: higher PM<jats:sub>2.5</jats:sub> levels have stronger positive associations with the IRR of hospitalization for Latinx individuals, and density and overcrowding show stronger associations for non-Hispanic white individuals. Our results show that the neighborhood built environment might pose an independent risk for COVID-19 hospitalization. Our results may inform public health and urban planning initiatives to lower the risk of hospitalization linked to COVID-19 and other respiratory pathogens.</jats:p>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5197-6394",
"affiliation": [],
"authenticated-orcid": true,
"family": "Rigolon",
"given": "Alessandro",
"sequence": "first"
},
{
"affiliation": [],
"family": "Németh",
"given": "Jeremy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Anderson-Gregson",
"given": "Brenn",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Miller",
"given": "Ana Rae",
"sequence": "additional"
},
{
"affiliation": [],
"family": "deSouza",
"given": "Priyanka",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Montague",
"given": "Brian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hussain",
"given": "Cory",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Erlandson",
"given": "Kristine M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rowan",
"given": "Sarah E.",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2023,
6,
14
]
],
"date-time": "2023-06-14T17:21:35Z",
"timestamp": 1686763295000
},
"deposited": {
"date-parts": [
[
2023,
6,
14
]
],
"date-time": "2023-06-14T17:22:50Z",
"timestamp": 1686763370000
},
"editor": [
{
"affiliation": [],
"family": "Wang",
"given": "Yuyan",
"sequence": "first"
}
],
"funder": [
{
"award": [
"EVOLVE 2020"
],
"name": "University of Colorado Denver, College of Architecture and Planning"
}
],
"indexed": {
"date-parts": [
[
2023,
6,
15
]
],
"date-time": "2023-06-15T04:19:00Z",
"timestamp": 1686802740824
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2023,
6,
14
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2023,
6,
14
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
14
]
],
"date-time": "2023-06-14T00:00:00Z",
"timestamp": 1686700800000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0286119",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0286119",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2023,
6,
14
]
]
},
"published-online": {
"date-parts": [
[
2023,
6,
14
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"author": "World Health Organization",
"journal-title": "WHO coronavirus",
"key": "pone.0286119.ref001",
"year": "2022"
},
{
"DOI": "10.1136/bmj.m2815",
"article-title": "Covid-19: What do we know about “long covid”?",
"author": "E. Mahase",
"doi-asserted-by": "crossref",
"first-page": "m2815",
"journal-title": "BMJ",
"key": "pone.0286119.ref002",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1117",
"article-title": "Challenges for NHS hospitals during COVID-19 epidemic",
"author": "J Willan",
"doi-asserted-by": "crossref",
"first-page": "m1117",
"journal-title": "BMJ",
"key": "pone.0286119.ref003",
"volume": "368",
"year": "2020"
},
{
"DOI": "10.1016/j.childyouth.2020.105866",
"article-title": "COVID-19 and its impact on education, social life and mental health of students: A survey",
"author": "K Chaturvedi",
"doi-asserted-by": "crossref",
"first-page": "105866",
"journal-title": "Child Youth Serv Rev",
"key": "pone.0286119.ref004",
"volume": "121",
"year": "2021"
},
{
"author": "W McKibbin",
"first-page": "45",
"key": "pone.0286119.ref005",
"volume-title": "Economics in the time of COVID-19",
"year": "2020"
},
{
"DOI": "10.1038/s41586-021-03792-w",
"article-title": "After the pandemic: perspectives on the future trajectory of COVID-19",
"author": "A Telenti",
"doi-asserted-by": "crossref",
"first-page": "495",
"journal-title": "Nature",
"key": "pone.0286119.ref006",
"volume": "596",
"year": "2021"
},
{
"DOI": "10.1093/cid/ciaa1012",
"article-title": "Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the US Coronavirus disease 2019 (COVID-19)-Associated hospitalization surveillance network (COVID-NET",
"author": "L Kim",
"doi-asserted-by": "crossref",
"first-page": "E206",
"journal-title": "Clin Infect Dis",
"key": "pone.0286119.ref007",
"volume": "72",
"year": "2021"
},
{
"DOI": "10.1111/jrh.12557",
"article-title": "The association of social determinants of health with COVID-19 mortality in rural and urban counties",
"author": "R Paul",
"doi-asserted-by": "crossref",
"first-page": "278",
"journal-title": "J Rural Heal",
"key": "pone.0286119.ref008",
"volume": "37",
"year": "2021"
},
{
"author": "PA Braveman",
"journal-title": "Neighborhoods and health",
"key": "pone.0286119.ref009",
"year": "2011"
},
{
"DOI": "10.1016/j.envres.2019.04.016",
"article-title": "Could nature help children rise out of poverty? Green space and future earnings from a cohort in ten U.S. cities",
"author": "MHEM Browning",
"doi-asserted-by": "crossref",
"first-page": "108449",
"journal-title": "Environ Res",
"key": "pone.0286119.ref010",
"volume": "176",
"year": "2019"
},
{
"DOI": "10.1093/qje/qju022",
"article-title": "Where is the land of opportunity? The geography of intergenerational mobility in the United States",
"author": "R Chetty",
"doi-asserted-by": "crossref",
"first-page": "1553",
"journal-title": "Q J Econ",
"key": "pone.0286119.ref011",
"volume": "129",
"year": "2014"
},
{
"DOI": "10.1016/j.envpol.2020.115176",
"article-title": "The effect of latitude and PM2.5 on spreading of SARS-CoV-2 in tropical and temperate zone countries",
"author": "K Chennakesavulu",
"doi-asserted-by": "crossref",
"first-page": "115176",
"journal-title": "Environ Pollut",
"key": "pone.0286119.ref012",
"volume": "266",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.05.031",
"article-title": "Severe air pollution links to higher mortality in COVID-19 patients: The “double-hit” hypothesis",
"author": "A Frontera",
"doi-asserted-by": "crossref",
"first-page": "255",
"journal-title": "J Infect",
"key": "pone.0286119.ref013",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.3390/v12060588",
"article-title": "Spatial–temporal variations in atmospheric factors contribute to SARS-CoV-2 outbreak",
"author": "R Fronza",
"doi-asserted-by": "crossref",
"first-page": "588",
"journal-title": "Viruses",
"key": "pone.0286119.ref014",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.envpol.2020.115126",
"article-title": "COVID-19 prevalence and fatality rates in association with air pollution emission concentrations and emission sources",
"author": "M Hendryx",
"doi-asserted-by": "crossref",
"first-page": "115126",
"journal-title": "Environ Pollut",
"key": "pone.0286119.ref015",
"volume": "265",
"year": "2020"
},
{
"DOI": "10.1016/j.envint.2021.106564",
"article-title": "Ambient fine particulate matter air pollution and the risk of hospitalization among COVID-19 positive individuals: Cohort study",
"author": "B Bowe",
"doi-asserted-by": "crossref",
"first-page": "106564",
"journal-title": "Environ Int",
"key": "pone.0286119.ref016",
"volume": "154",
"year": "2021"
},
{
"DOI": "10.1016/j.envres.2021.111331",
"article-title": "County-level exposures to greenness and associations with COVID-19 incidence and mortality in the United States",
"author": "JO Klompmaker",
"doi-asserted-by": "crossref",
"first-page": "111331",
"journal-title": "Environ Res",
"key": "pone.0286119.ref017",
"volume": "199",
"year": "2021"
},
{
"DOI": "10.1016/j.scitotenv.2022.155095",
"article-title": "Nature’s contributions in coping with a pandemic in the 21st century: A narrative review of evidence during COVID-19",
"author": "SM Labib",
"doi-asserted-by": "crossref",
"first-page": "155095",
"journal-title": "Sci Total Environ",
"key": "pone.0286119.ref018",
"volume": "833",
"year": "2022"
},
{
"DOI": "10.1016/j.cities.2020.102759",
"article-title": "Emerging study on the transmission of the Novel Coronavirus (COVID-19) from urban perspective: Evidence from China",
"author": "L. Liu",
"doi-asserted-by": "crossref",
"first-page": "102759",
"journal-title": "Cities",
"key": "pone.0286119.ref019",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.3390/ijerph18147561",
"article-title": "Review of associations between built environment characteristics and severe acute respiratory syndrome coronavirus 2 infection risk",
"author": "J Wang",
"doi-asserted-by": "crossref",
"first-page": "7561",
"journal-title": "Int J Environ Res Public Health",
"key": "pone.0286119.ref020",
"volume": "18",
"year": "2021"
},
{
"article-title": "Urban vegetation slows down the spread of coronavirus disease (COVID-19) in the United States",
"author": "Y You",
"first-page": "e2020GL089286",
"journal-title": "Geophys Res Lett",
"key": "pone.0286119.ref021",
"volume": "47",
"year": "2020"
},
{
"DOI": "10.1016/j.puhe.2020.06.056",
"article-title": "Coronavirus disease 2019 mortality: A multivariate ecological analysis in relation to ethnicity, population density, obesity, deprivation and pollution",
"author": "I Bray",
"doi-asserted-by": "crossref",
"first-page": "261",
"journal-title": "Public Health",
"key": "pone.0286119.ref022",
"volume": "185",
"year": "2020"
},
{
"DOI": "10.1111/cars.12336",
"article-title": "Studying the social determinants of COVID-19 in a data vacuum",
"author": "KH Choi",
"doi-asserted-by": "crossref",
"first-page": "146",
"journal-title": "Can Rev Sociol",
"key": "pone.0286119.ref023",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.1016/j.scitotenv.2020.141028",
"article-title": "The spread of 2019-nCoV in China was primarily driven by population density. Comment on “Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China” by Zhu et al.",
"author": "S Copiello",
"doi-asserted-by": "crossref",
"first-page": "141028",
"journal-title": "Sci Total Environ",
"key": "pone.0286119.ref024",
"volume": "744",
"year": "2020"
},
{
"DOI": "10.3390/ijerph17155477",
"article-title": "Correlation between COVID-19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity",
"author": "S Kodera",
"doi-asserted-by": "crossref",
"first-page": "5477",
"journal-title": "Int J Environ Res Public Health",
"key": "pone.0286119.ref025",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.7326/M20-6306",
"article-title": "Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review",
"author": "K Mackey",
"doi-asserted-by": "crossref",
"first-page": "362",
"journal-title": "Ann Intern Med",
"key": "pone.0286119.ref026",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1186/s12939-020-01208-1",
"article-title": "Coronavirus disease 19 in minority populations of Newark, New Jersey",
"author": "AK Okoh",
"doi-asserted-by": "crossref",
"first-page": "93",
"journal-title": "Int J Equity Health",
"key": "pone.0286119.ref027",
"volume": "19",
"year": "2020"
},
{
"article-title": "Early geography of the coronavirus disease outbreak in Nigeria",
"author": "A Olusola",
"journal-title": "GeoJournal",
"key": "pone.0286119.ref028",
"year": "2020"
},
{
"DOI": "10.3390/ijerph17113856",
"article-title": "COVID-19 emergence and social and health determinants in Colorado: A rapid spatial analysis",
"author": "IJ Ramírez",
"doi-asserted-by": "crossref",
"first-page": "3856",
"journal-title": "Int J Environ Res Public Health",
"key": "pone.0286119.ref029",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.annepidem.2020.10.011",
"article-title": "Coronavirus disease 2019 (COVID-19) mortality and neighborhood characteristics in Chicago",
"author": "M Scannell Bryan",
"doi-asserted-by": "crossref",
"first-page": "47",
"journal-title": "Ann Epidemiol",
"key": "pone.0286119.ref030",
"volume": "56",
"year": "2021"
},
{
"DOI": "10.1111/jrh.12476",
"article-title": "Spatial disparities in coronavirus incidence and mortality in the United States: An ecological analysis as of May 2020",
"author": "CH Zhang",
"doi-asserted-by": "crossref",
"first-page": "433",
"journal-title": "J Rural Heal",
"key": "pone.0286119.ref031",
"volume": "36",
"year": "2020"
},
{
"DOI": "10.1111/tesg.12437",
"article-title": "Urban-rural polarisation in times of the Corona outbreak? The early demographic and geographic patterns of the SARS-CoV-2 epidemic in the Netherlands",
"author": "WR Boterman",
"doi-asserted-by": "crossref",
"first-page": "513",
"journal-title": "Tijdschr voor Econ en Soc Geogr",
"key": "pone.0286119.ref032",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.1080/01944363.2020.1777891",
"article-title": "Does density aggravate the COVID-19 pandemic?: Early findings and lessons for Planners",
"author": "S Hamidi",
"doi-asserted-by": "crossref",
"first-page": "495",
"journal-title": "J Am Plan Assoc",
"key": "pone.0286119.ref033",
"volume": "86",
"year": "2020"
},
{
"DOI": "10.1007/s11524-020-00468-0",
"article-title": "Covid-19 and Inequity: A comparative spatial analysis of New York City and Chicago hot spots",
"author": "A Maroko",
"doi-asserted-by": "crossref",
"first-page": "461",
"journal-title": "J Urban Heal",
"key": "pone.0286119.ref034",
"volume": "97",
"year": "2020"
},
{
"DOI": "10.1016/j.scitotenv.2020.141347",
"article-title": "Impacts of geographic factors and population density on the COVID-19 spreading under the lockdown policies of China",
"author": "Z Sun",
"doi-asserted-by": "crossref",
"first-page": "141347",
"journal-title": "Sci Total Environ",
"key": "pone.0286119.ref035",
"volume": "746",
"year": "2020"
},
{
"DOI": "10.1016/j.envint.2021.106465",
"article-title": "Green spaces mitigate racial disparity of health: A higher ratio of green spaces indicates a lower racial disparity in SARS-CoV-2 infection rates in the USA",
"author": "Y Lu",
"doi-asserted-by": "crossref",
"first-page": "106465",
"journal-title": "Environ Int",
"key": "pone.0286119.ref036",
"volume": "152",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0273125",
"article-title": "Integrated analysis of doubly disadvantaged neighborhoods by considering both green space and blue space accessibility and COVID-19 infection risk",
"author": "D Liu",
"doi-asserted-by": "crossref",
"first-page": "e0273125",
"journal-title": "PLoS One",
"key": "pone.0286119.ref037",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1007/s40615-020-00948-8",
"article-title": "Structural racism and COVID-19 in the USA: A county-level empirical analysis",
"author": "Bin Tan S",
"doi-asserted-by": "crossref",
"first-page": "236",
"journal-title": "J Racial Ethn Heal Disparities",
"key": "pone.0286119.ref038",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1038/s41893-021-00781-9",
"article-title": "Nature inequity and higher COVID-19 case rates in less-green neighbourhoods in the United States",
"author": "EN Spotswood",
"doi-asserted-by": "crossref",
"first-page": "1092",
"journal-title": "Nat Sustain",
"key": "pone.0286119.ref039",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0263779",
"article-title": "Perceptions of green space usage, abundance, and quality of green space were associated with better mental health during the COVID-19 pandemic among residents of Denver",
"author": "CE Reid",
"doi-asserted-by": "crossref",
"first-page": "e0263779",
"journal-title": "PLoS One",
"key": "pone.0286119.ref040",
"volume": "17",
"year": "2022"
},
{
"author": "Center for Disease Control and Prevention",
"journal-title": "Risk for COVID-19 infection, hospitalization, and death by race/ethnicity",
"key": "pone.0286119.ref041",
"year": "2021"
},
{
"author": "Denver Health Medical Center",
"first-page": "1",
"key": "pone.0286119.ref042"
},
{
"key": "pone.0286119.ref043",
"unstructured": "DRCOG. DRCOG FAQ. Available: https://drcog.org/about-drcog/drcog-faq."
},
{
"article-title": "Denver’s population grew by more than 115,000 residents in the last decade. In: Denverite",
"author": "EL Hernandez",
"key": "pone.0286119.ref044",
"year": "2021"
},
{
"author": "Urban Displacement Project.",
"journal-title": "Denver–gentrification and displacement",
"key": "pone.0286119.ref045",
"year": "2021"
},
{
"author": "Centers for Disease Control and Prevention",
"journal-title": "Underlying medical conditions associated with higher risk for severe COVID-19: Information for healthcare professionals",
"key": "pone.0286119.ref046",
"year": "2022"
},
{
"author": "Centers for Disease Control and Prevention",
"journal-title": "Science brief: Evidence used to update the list of underlying medical conditions associated with higher risk for severe COVID-19",
"key": "pone.0286119.ref047",
"year": "2022"
},
{
"author": "Centers for Disease Control and Prevention",
"journal-title": "Body measurements. In: National Center for Health Statistics",
"key": "pone.0286119.ref048",
"year": "2021"
},
{
"DOI": "10.1080/23748834.2019.1636507",
"article-title": "Gentrification and health in two global cities: A call to identify impacts for socially-vulnerable residents",
"author": "I Anguelovski",
"doi-asserted-by": "crossref",
"first-page": "40",
"journal-title": "Cities Heal",
"key": "pone.0286119.ref049",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1289/EHP8888",
"article-title": "COVID-19, the built environment, and health",
"author": "H. Frumkin",
"doi-asserted-by": "crossref",
"first-page": "075001",
"journal-title": "Environ Heal Perpsectives",
"key": "pone.0286119.ref050",
"volume": "129",
"year": "2021"
},
{
"DOI": "10.1016/j.scs.2020.102350",
"article-title": "Antivirus-built environment: Lessons learned from Covid-19 pandemic",
"author": "NA Megahed",
"doi-asserted-by": "crossref",
"first-page": "102350",
"journal-title": "Sustain Cities Soc",
"key": "pone.0286119.ref051",
"volume": "61",
"year": "2020"
},
{
"author": "MD Pinheiro",
"first-page": "5863",
"journal-title": "COVID-19 could leverage a sustainable built environment. Sustainability",
"key": "pone.0286119.ref052",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1007/s40572-021-00307-7",
"article-title": "Built environment, transport, and COVID-19: A review",
"author": "D Rojas-Rueda",
"doi-asserted-by": "crossref",
"first-page": "138",
"journal-title": "Curr Environ Heal Reports",
"key": "pone.0286119.ref053",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.2196/30619",
"article-title": "The disclosure of personally identifiable information in studies of neighborhood contexts and patient outcomes",
"author": "AG Rundle",
"doi-asserted-by": "crossref",
"first-page": "e30619",
"journal-title": "J Med Internet Res",
"key": "pone.0286119.ref054",
"volume": "24",
"year": "2022"
},
{
"article-title": "Texas A&M Geoservices",
"author": "Security information",
"key": "pone.0286119.ref055",
"year": "2022"
},
{
"author": "A. Field",
"key": "pone.0286119.ref056",
"volume-title": "Discovering statistics using SPSS",
"year": "2013"
},
{
"author": "U.S. Census Bureau",
"journal-title": "American Community Survey data",
"key": "pone.0286119.ref057",
"year": "2020"
},
{
"author": "U.S. Environmental Protection Agency",
"journal-title": "Download EJSCREEN Data.",
"key": "pone.0286119.ref058"
},
{
"author": "Colorado Department of Transportation",
"journal-title": "Highways",
"key": "pone.0286119.ref059",
"year": "2021"
},
{
"author": "U.S. Geological Survey",
"journal-title": "Earth explorer.",
"key": "pone.0286119.ref060"
},
{
"author": "DRCOG",
"journal-title": "Parks recreation and open space",
"key": "pone.0286119.ref061",
"year": "2019"
},
{
"author": "WalkScore",
"journal-title": "Walkability, real estate, and public health data",
"key": "pone.0286119.ref062",
"year": "2021"
},
{
"author": "U.S. Department of Homeland Security",
"journal-title": "Guidance on essential infrastructure workforce: Ensuring community and national resilience in COVID-19 response",
"key": "pone.0286119.ref063",
"year": "2020"
},
{
"DOI": "10.3390/ijerph18041446",
"article-title": "COVID-19 and essential workers: A narrative review of health outcomes and moral injury",
"author": "J Gaitens",
"doi-asserted-by": "crossref",
"first-page": "1446",
"journal-title": "Int J Environ Res Public Health",
"key": "pone.0286119.ref064",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1016/j.trd.2020.102654",
"article-title": "Who left riding transit? Examining socioeconomic disparities in the impact of COVID-19 on ridership",
"author": "S Hu",
"doi-asserted-by": "crossref",
"first-page": "102654",
"journal-title": "Transp Res Part D Transp Environ",
"key": "pone.0286119.ref065",
"volume": "90",
"year": "2021"
},
{
"DOI": "10.15585/mmwr.mm6938a4",
"article-title": "Disparities in COVID-19 incidence, hospitalizations, and testing, by area-level deprivation—Utah, March 3 –July 9, 2020",
"author": "NM Lewis",
"doi-asserted-by": "crossref",
"first-page": "1369",
"journal-title": "Morb Mortal Wkly Rep",
"key": "pone.0286119.ref066",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.7326/M21-2615",
"article-title": "Contribution of individual- and neighborhood-level social, demographic, and health factors to COVID-19 hospitalization outcomes",
"author": "R Tipirneni",
"doi-asserted-by": "crossref",
"first-page": "505",
"journal-title": "Ann Intern Med",
"key": "pone.0286119.ref067",
"volume": "175",
"year": "2022"
},
{
"DOI": "10.1503/cmaj.101715",
"article-title": "Overestimation of risk ratios by odds ratios in trials and cohort studies: Alternatives to logistic regression",
"author": "MJ Knol",
"doi-asserted-by": "crossref",
"first-page": "895",
"journal-title": "C Can Med Assoc J",
"key": "pone.0286119.ref068",
"volume": "184",
"year": "2012"
},
{
"article-title": "Package ‘pscl",
"author": "S Jackman",
"journal-title": "CRAN",
"key": "pone.0286119.ref069",
"year": "2022"
},
{
"DOI": "10.5243/jsswr.2010.2",
"article-title": "Suppressor variables in social work research: Ways to identify in multiple regression models",
"author": "S Pandey",
"doi-asserted-by": "crossref",
"first-page": "28",
"journal-title": "J Soc Social Work Res",
"key": "pone.0286119.ref070",
"volume": "1",
"year": "2010"
},
{
"DOI": "10.1289/ehp.1205201",
"article-title": "Environmental inequality in exposures to airborne particulate matter components in the United States",
"author": "ML Bell",
"doi-asserted-by": "crossref",
"first-page": "1699",
"journal-title": "Environ Heal Perpsectives",
"key": "pone.0286119.ref071",
"volume": "120",
"year": "2012"
},
{
"author": "DA Griffith",
"key": "pone.0286119.ref072",
"volume-title": ": Gaining understanding through theory and scientific visualization",
"year": "2003"
},
{
"DOI": "10.1016/j.envres.2021.111930",
"article-title": "Positive association between outdoor air pollution and the incidence and severity of COVID-19. A review of the recent scientific evidences",
"author": "M Marquès",
"doi-asserted-by": "crossref",
"first-page": "111930",
"journal-title": "Environ Res",
"key": "pone.0286119.ref073",
"volume": "203",
"year": "2022"
},
{
"DOI": "10.1056/NEJMra2030281",
"article-title": "Pollution and the heart",
"author": "S Rajagopalan",
"doi-asserted-by": "crossref",
"first-page": "1881",
"journal-title": "N Engl J Med",
"key": "pone.0286119.ref074",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1016/j.scitotenv.2020.143391",
"article-title": "Ambient PM2.5 exposure and rapid spread of COVID-19 in the United States",
"author": "RK Chakrabarty",
"doi-asserted-by": "crossref",
"first-page": "143391",
"journal-title": "Sci Total Environ",
"key": "pone.0286119.ref075",
"volume": "760",
"year": "2021"
},
{
"DOI": "10.1016/j.rmed.2021.106313",
"article-title": "Long-term exposure to fine particulate matter and hospitalization in COVID-19 patients",
"author": "A Mendy",
"doi-asserted-by": "crossref",
"first-page": "106313",
"journal-title": "Respir Med",
"key": "pone.0286119.ref076",
"volume": "178",
"year": "2020"
},
{
"DOI": "10.1016/j.freeradbiomed.2020.01.179",
"article-title": "Air pollution and its effects on the immune system",
"author": "DA Glencross",
"doi-asserted-by": "crossref",
"first-page": "56",
"journal-title": "Free Radic Biol Med",
"key": "pone.0286119.ref077",
"volume": "151",
"year": "2020"
},
{
"DOI": "10.1111/jebm.12430",
"article-title": "Emerging role of air pollution and meteorological parameters in COVID-19",
"author": "C Zhao",
"doi-asserted-by": "crossref",
"first-page": "123",
"journal-title": "J Evid Based Med",
"key": "pone.0286119.ref078",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1016/j.envres.2021.111281",
"article-title": "Role of atmospheric particulate matter exposure in COVID-19 and other health risks in human: A review",
"author": "C Zhu",
"doi-asserted-by": "crossref",
"first-page": "111281",
"journal-title": "Environ Res",
"key": "pone.0286119.ref079",
"volume": "198",
"year": "2021"
},
{
"DOI": "10.1126/sciadv.abf4491",
"article-title": "PM2.5 polluters disproportionately and systemically affect people of color in the United States",
"author": "CW Tessum",
"doi-asserted-by": "crossref",
"first-page": "eabf4491",
"journal-title": "Sci Adv",
"key": "pone.0286119.ref080",
"volume": "7",
"year": "2021"
},
{
"article-title": "Structural racism and COVID-19 in the USA: A county-level empirical analysis",
"author": "Bin Tan S",
"journal-title": "J Racial Ethn Heal Disparities",
"key": "pone.0286119.ref081",
"year": "2021"
},
{
"DOI": "10.1111/rsp3.12321",
"article-title": "Neighbourhood inequity: Exploring the factors underlying racial and ethnic disparities in COVID-19 testing and infection rates using ZIP code data in Chicago and New York",
"author": "K. Credit",
"doi-asserted-by": "crossref",
"first-page": "1249",
"journal-title": "Reg Sci Policy Pract",
"key": "pone.0286119.ref082",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1080/00330124.2021.1895851",
"article-title": "COVID-19 cases and the built environment: Initial evidence from New York City",
"author": "CP Tribby",
"doi-asserted-by": "crossref",
"first-page": "365",
"journal-title": "Prof Geogr",
"key": "pone.0286119.ref083",
"volume": "73",
"year": "2021"
},
{
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients",
"author": "R Sallis",
"journal-title": "Br J Sports Med",
"key": "pone.0286119.ref084",
"year": "2021"
},
{
"DOI": "10.1080/01944363.2021.1886974",
"article-title": "Riders who avoided public transit during COVID-19: Personal burdens and implications for social equity",
"author": "M Palm",
"doi-asserted-by": "crossref",
"first-page": "455",
"journal-title": "J Am Plan Assoc",
"key": "pone.0286119.ref085",
"volume": "87",
"year": "2021"
},
{
"DOI": "10.1016/j.jtho.2020.12.008",
"article-title": "Statistical considerations for subgroup analyses",
"author": "X Wang",
"doi-asserted-by": "crossref",
"first-page": "375",
"journal-title": "J Thorac Oncol",
"key": "pone.0286119.ref086",
"volume": "16",
"year": "2021"
},
{
"article-title": "Uncertainties in the assessment of COVID-19 risk: A study of people’s exposure to high-risk environments using individual-level activity data",
"author": "J Huang",
"journal-title": "Ann Am Assoc Geogr",
"key": "pone.0286119.ref087",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2034577",
"article-title": "Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine",
"author": "FP Polack",
"doi-asserted-by": "crossref",
"first-page": "2603",
"journal-title": "N Engl J Med",
"key": "pone.0286119.ref088",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2035389",
"article-title": "Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine",
"author": "LR Baden",
"doi-asserted-by": "crossref",
"first-page": "403",
"journal-title": "N Engl J Med",
"key": "pone.0286119.ref089",
"volume": "384",
"year": "2021"
},
{
"author": "National Institutes of Health",
"journal-title": "COVID-19 treatment guidelines",
"key": "pone.0286119.ref090",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(17)30505-6",
"article-title": "Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015",
"author": "AJ Cohen",
"doi-asserted-by": "crossref",
"first-page": "1907",
"journal-title": "Lancet",
"key": "pone.0286119.ref091",
"volume": "389",
"year": "2017"
},
{
"DOI": "10.1097/EDE.0000000000001265",
"article-title": "Nationwide study of short-term exposure to fine particulate matter and cardiovascular hospitalizations among medicaid enrollees",
"author": "P deSouza",
"doi-asserted-by": "crossref",
"first-page": "6",
"journal-title": "Epidemiology.",
"key": "pone.0286119.ref092",
"volume": "32",
"year": "2021"
},
{
"DOI": "10.1001/jama.295.10.1127",
"article-title": "Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases",
"author": "F Dominici",
"doi-asserted-by": "crossref",
"first-page": "1127",
"journal-title": "J Am Med Assoc",
"key": "pone.0286119.ref093",
"volume": "295",
"year": "2006"
},
{
"DOI": "10.1016/S2542-5196(19)30241-4",
"article-title": "Associations between historical residential redlining and current age-adjusted rates of emergency department visits due to asthma across eight cities in California: an ecological study",
"author": "A Nardone",
"doi-asserted-by": "crossref",
"first-page": "e24",
"journal-title": "Lancet Planet Heal",
"key": "pone.0286119.ref094",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1289/EHP7495",
"article-title": "Redlines and greenspace: The Relationship between historical redlining and 2010 greenspace across the United States",
"author": "A Nardone",
"doi-asserted-by": "crossref",
"first-page": "017006",
"journal-title": "Environ Health Perspect",
"key": "pone.0286119.ref095",
"volume": "129",
"year": "2021"
},
{
"article-title": "The road to racial justice: Resolving the disproportionate health burden placed on communities of color by highway pollution",
"author": "WQ Xiao",
"first-page": "911",
"journal-title": "Columbia Human Rights Law Rev",
"key": "pone.0286119.ref096",
"volume": "52",
"year": "2021"
},
{
"DOI": "10.1016/j.envres.2017.06.028",
"article-title": "Exploring pathways linking greenspace to health: Theoretical and methodological guidance",
"author": "I Markevych",
"doi-asserted-by": "crossref",
"first-page": "301",
"journal-title": "Environ Res",
"key": "pone.0286119.ref097",
"volume": "158",
"year": "2017"
},
{
"DOI": "10.1080/01944363.2021.1955735",
"article-title": "Open streets for whom? Toward a just livability revolution",
"author": "D Slabaugh",
"doi-asserted-by": "crossref",
"first-page": "253",
"journal-title": "J Am Plan Assoc",
"key": "pone.0286119.ref098",
"volume": "88",
"year": "2022"
},
{
"DOI": "10.1016/j.trd.2021.103027",
"article-title": "Biking where Black: Connecting transportation planning and infrastructure to disproportionate policing",
"author": "JM Barajas",
"doi-asserted-by": "crossref",
"first-page": "103027",
"journal-title": "Transp Res Part D Transp Environ",
"key": "pone.0286119.ref099",
"volume": "99",
"year": "2021"
},
{
"DOI": "10.1016/S2542-5196(21)00135-2",
"article-title": "Integrating solutions to adapt cities for climate change",
"author": "BB Lin",
"doi-asserted-by": "crossref",
"first-page": "e479",
"journal-title": "Lancet Planet Heal",
"key": "pone.0286119.ref100",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1007/978-3-319-74983-9",
"author": "M Nieuwenhuijsen",
"doi-asserted-by": "crossref",
"key": "pone.0286119.ref101",
"volume-title": "Integrating human health into urban and transport planning: A framework",
"year": "2019"
}
],
"reference-count": 101,
"references-count": 101,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0286119"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "The neighborhood built environment and COVID-19 hospitalizations",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "18"
}
