Very Low Vitamin D Levels are a Strong Independent Predictor of Mortality in Hospitalized Patients with Severe COVID-19
et al., Archives of Medical Research, doi:10.1016/j.arcmed.2021.09.006, Oct 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 2,908 hospitalized patients in Mexico with vitamin D levels measured on admission, showing significantly lower mortality for patients without vitamin D deficiency.
This is the 99th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
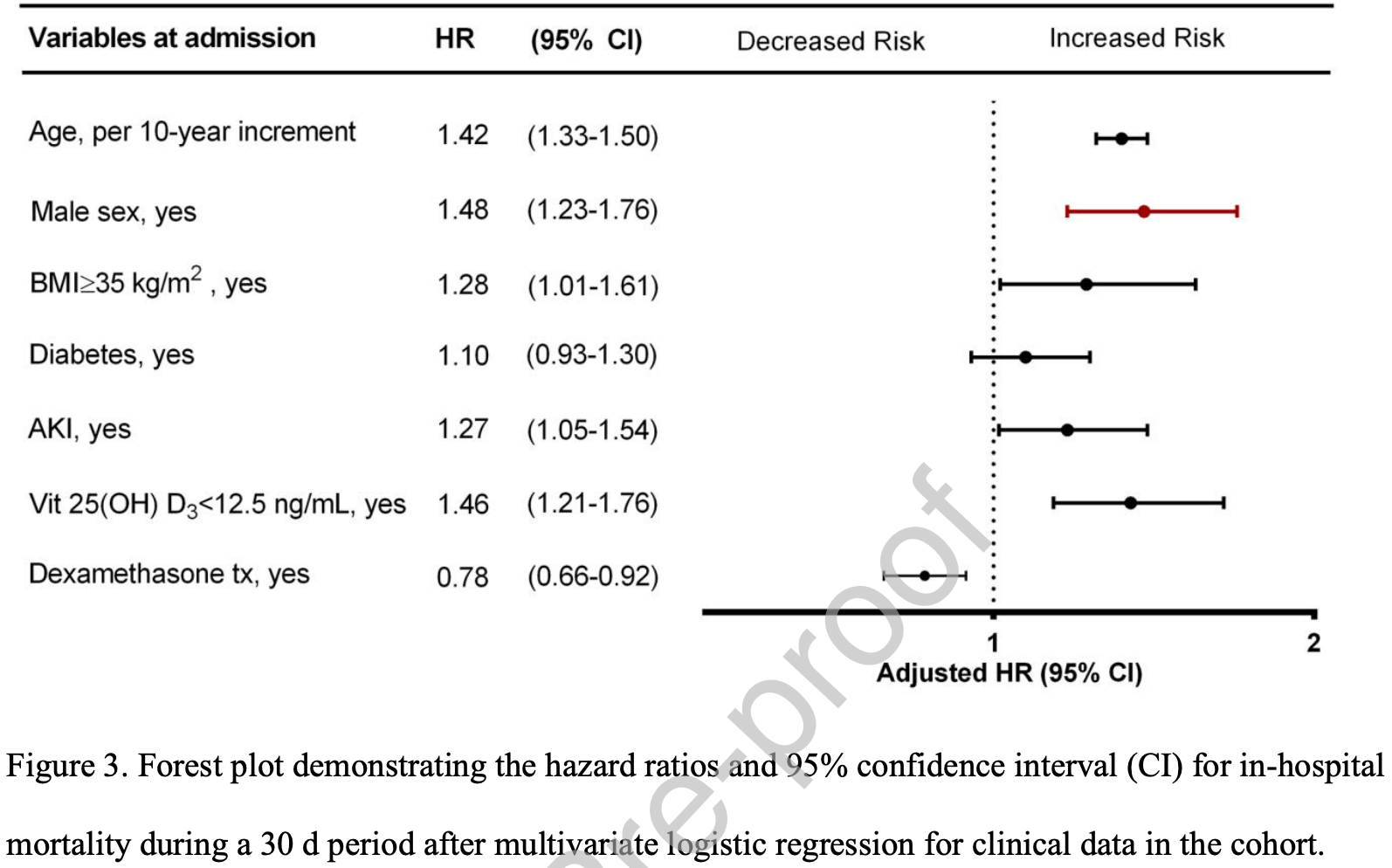
risk of death, 31.5% lower, HR 0.68, p < 0.001, high D levels 2,337, low D levels 571, adjusted per study, inverted to make HR<1 favor high D levels, >12.5ng/mL, 30 day in-hospital mortality.
|
|
hospitalization time, 22.2% lower, relative time 0.78, p < 0.001, high D levels 2,337, low D levels 571.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ramirez-Sandoval et al., 15 Oct 2021, retrospective, Mexico, peer-reviewed, 7 authors.
Very Low Vitamin D Levels are a Strong Independent Predictor of Mortality in Hospitalized Patients with Severe COVID-19
Archives of Medical Research, doi:10.1016/j.arcmed.2021.09.006
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
Aatsinki, Elkhwanky, Kummu, Fasting-induced transcription factors repress Vitamin D bioactivation, a mechanism for Vitamin D deficiency in diabetes, Diabetes
Autier, Boniol, Pizot, Mullie, Vitamin D status and ill health: A systematic review, Lancet Diabetes Endocrinol
Baktash, Hosack, Patel, Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med J
Bianconi, Mannarino, Figorilli, Prevalence of vitamin D deficiency and its prognostic impact on patients hospitalized with COVID-19, Nutrition
Bouillon, Bikle, Vitamin D Metabolism Revised: Fall of Dogmas, J Bone Miner Res
Charlson, Pompei, Ales, Mc, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis
Demir, Demir, Aygun, Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease, J Med Virol
Ge, Trujillo, Miller, Circulating complexes of the vitamin D binding protein with G-actin induce lung inflammation by targeting endothelial cells, Immunobiology
Grove, Osokogu, Al-Khudairy, Association between vitamin D supplementation or serum vitamin D level and susceptibility to SARS-CoV-2 infection or COVID-19 including clinical course, morbidity and mortality outcomes? A systematic review, BMJ Open
Güven, Gültekin, Association of 25-Hydroxyvitamin D Level with COVID-19-Related in-Hospital Mortality: A Retrospective Cohort Study, J Am Coll Nutr
Harvey, Cooper, Raisi-Estabragh, Vitamin D and COVID-19 disease: don't believe everything you read in the papers! Reply to Dr William B. Grant, Aging Clin Exp Res
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr Clin Res Rev
Hernández, Nan, Fernandez-Ayala, Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection, J Clin Endocrinol Metab
Horby, Lim, Emberson, Effect of Dexamethasone in Hospitalized Patients with COVID-19 -Preliminary Report. Prepr medRxiv, doi:10.1101/2020.06.22.20137273
Khoo, Chai, Koenen, Joosten, Netea et al., Translating the role of vitamin D 3 in infectious diseases, Crit Rev Microbiol
Kuba, Imai, Penninger, Angiotensin-converting enzyme 2 in lung diseases, Curr Opin Pharmacol
Lakkireddy, Gadiga, Malathi, Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease, Sci Rep
Manson, Brannon, Rosen, Vitamin D Deficiency -Is There Really a Pandemic?, N Engl J Med
Martineau, Forouhi, Vitamin D for COVID-19: a case to answer?, Lancet Diabetes Endocrinol
Mazahery, Hurst, Factors affecting 25-hydroxyvitamin D concentration in response to vitamin D supplementation, Nutrients
Munshi, Hussein, Toraih, Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J Med Virol
Murai, Fernandes, Sales, Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients with Moderate to Severe COVID-19: A Randomized Clinical Trial, JAMA
Nimavat, Singh, Singh, Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India, Ann Med Surg
Pan, Sze, Minhas, The impact of ethnicity on clinical outcomes in COVID-19: A systematic review, E Clin Med
Raisi-Estabragh, Martineau, Curtis, Vitamin D and coronavirus disease 2019 (COVID-19): rapid evidence review, Aging Clin Exp Res
Rajan, Dashti, In-hospital Mortality in SARS-CoV-2 stratified by serum 25-Hydroxy-Vitamin D levels: A Retrospective Study, J Med Virol, doi:10.1002/jmv.27133
Reid, Towards a trial-based definition of vitamin D deficiency, Lancet Diabetes Endocrinol
Roizen, Long, Casella, Obesity Decreases Hepatic 25-Hydroxylase Activity Causing Low Serum 25-Hydroxyvitamin D, J Bone Min Res
Rubin, Sorting out Whether Vitamin D Deficiency Raises COVID-19 Risk, JAMA
Shinkyo, Sakaki, Kamakura, Metabolism of vitamin D by human microsomal CYP2R1, Biochem Biophys Res Commun
Snellman, Melhus, Gedeborg, Determining vitamin D status: A comparison between commercially available assays, PLoS One
Vanegas-Cedillo, Bello-Chavolla, Ramírez-Pedraza, Serum Vitamin D levels are associated with increased COVID-19 severity and mortality independent of visceral adiposity, medRxiv
DOI record:
{
"DOI": "10.1016/j.arcmed.2021.09.006",
"ISSN": [
"0188-4409"
],
"URL": "http://dx.doi.org/10.1016/j.arcmed.2021.09.006",
"alternative-id": [
"S0188440921001983"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Very Low Vitamin D Levels are a Strong Independent Predictor of Mortality in Hospitalized Patients with Severe COVID-19"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Archives of Medical Research"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.arcmed.2021.09.006"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Instituto Mexicano del Seguro Social (IMSS). Published by Elsevier Inc. All rights reserved."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-2735-2941",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ramirez-Sandoval",
"given": "Juan C.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Castillos-Ávalos",
"given": "Valeria Jocelyne",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Paz-Cortés",
"given": "Armando",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Santillan-Ceron",
"given": "Airy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hernandez-Jimenez",
"given": "Sergio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mehta",
"given": "Roopa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Correa-Rotter",
"given": "Ricardo",
"sequence": "additional"
}
],
"container-title": "Archives of Medical Research",
"container-title-short": "Archives of Medical Research",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.fr",
"clinicalkey.com.au",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
10,
15
]
],
"date-time": "2021-10-15T23:04:27Z",
"timestamp": 1634339067000
},
"deposited": {
"date-parts": [
[
2023,
1,
12
]
],
"date-time": "2023-01-12T11:57:36Z",
"timestamp": 1673524656000
},
"indexed": {
"date-parts": [
[
2024,
3,
2
]
],
"date-time": "2024-03-02T03:19:54Z",
"timestamp": 1709349594750
},
"is-referenced-by-count": 10,
"issue": "2",
"issued": {
"date-parts": [
[
2022,
2
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2022,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
2,
1
]
],
"date-time": "2022-02-01T00:00:00Z",
"timestamp": 1643673600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0188440921001983?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0188440921001983?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "215-222",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
2
]
]
},
"published-print": {
"date-parts": [
[
2022,
2
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/S2213-8587(20)30268-0",
"article-title": "Vitamin D for COVID-19: a case to answer?",
"author": "Martineau",
"doi-asserted-by": "crossref",
"first-page": "735",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.1016/j.arcmed.2021.09.006_bib0001",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26360",
"article-title": "Vitamin D insufficiency as a potential culprit in critical COVID-19 patients",
"author": "Munshi",
"doi-asserted-by": "crossref",
"first-page": "733",
"journal-title": "J Med Virol",
"key": "10.1016/j.arcmed.2021.09.006_bib0002",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26832",
"article-title": "Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease",
"author": "Demir",
"doi-asserted-by": "crossref",
"first-page": "2992",
"journal-title": "J Med Virol",
"key": "10.1016/j.arcmed.2021.09.006_bib0003",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(13)70165-7",
"article-title": "Vitamin D status and ill health: A systematic review",
"author": "Autier",
"doi-asserted-by": "crossref",
"first-page": "76",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.1016/j.arcmed.2021.09.006_bib0004",
"volume": "2",
"year": "2014"
},
{
"DOI": "10.3109/1040841X.2011.622716",
"article-title": "Translating the role of vitamin D 3 in infectious diseases",
"author": "Khoo",
"doi-asserted-by": "crossref",
"first-page": "122",
"journal-title": "Crit Rev Microbiol",
"key": "10.1016/j.arcmed.2021.09.006_bib0005",
"volume": "38",
"year": "2012"
},
{
"DOI": "10.1210/clinem/dgaa733",
"article-title": "Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection",
"author": "Hernández",
"doi-asserted-by": "crossref",
"first-page": "e1343",
"journal-title": "J Clin Endocrinol Metab",
"key": "10.1016/j.arcmed.2021.09.006_bib0006",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients with Moderate to Severe COVID-19: A Randomized Clinical Trial",
"author": "Murai",
"doi-asserted-by": "crossref",
"first-page": "1053",
"journal-title": "JAMA",
"key": "10.1016/j.arcmed.2021.09.006_bib0007",
"volume": "325",
"year": "2021"
},
{
"article-title": "Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease",
"author": "Lakkireddy",
"first-page": "1",
"journal-title": "Sci Rep",
"key": "10.1016/j.arcmed.2021.09.006_bib0008",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.24127",
"article-title": "Sorting out Whether Vitamin D Deficiency Raises COVID-19 Risk",
"author": "Rubin",
"doi-asserted-by": "crossref",
"first-page": "329",
"journal-title": "JAMA",
"key": "10.1016/j.arcmed.2021.09.006_bib0009",
"volume": "325",
"year": "2021"
},
{
"article-title": "Vitamin D and COVID-19 disease: don't believe everything you read in the papers! Reply to Dr William B. Grant",
"author": "Harvey",
"first-page": "1",
"journal-title": "Aging Clin Exp Res",
"key": "10.1016/j.arcmed.2021.09.006_bib0010",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1136/bmjopen-2020-043737",
"article-title": "Association between vitamin D supplementation or serum vitamin D level and susceptibility to SARS-CoV-2 infection or COVID-19 including clinical course, morbidity and mortality outcomes? A systematic review",
"author": "Grove",
"doi-asserted-by": "crossref",
"journal-title": "BMJ Open",
"key": "10.1016/j.arcmed.2021.09.006_bib0011",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1080/07315724.2021.1935361",
"article-title": "Association of 25-Hydroxyvitamin D Level with COVID-19-Related in-Hospital Mortality: A Retrospective Cohort Study",
"author": "Güven",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J Am Coll Nutr",
"key": "10.1016/j.arcmed.2021.09.006_bib0012",
"volume": "0",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27133",
"article-title": "In-hospital Mortality in SARS-CoV-2 stratified by serum 25-Hydroxy-Vitamin D levels: A Retrospective Study",
"author": "Al-Jarallah",
"doi-asserted-by": "crossref",
"first-page": "5880",
"journal-title": "J Med Virol",
"key": "10.1016/j.arcmed.2021.09.006_bib0013",
"volume": "93",
"year": "2021"
},
{
"article-title": "Prevalence of vitamin D deficiency and its prognostic impact on patients hospitalized with COVID-19",
"author": "Bianconi",
"journal-title": "Nutrition",
"key": "10.1016/j.arcmed.2021.09.006_bib0014",
"volume": "91–92",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"article-title": "Vitamin D concentrations and COVID-19 infection in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "561",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "10.1016/j.arcmed.2021.09.006_bib0015",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"article-title": "Vitamin D status and outcomes for hospitalised older patients with COVID-19",
"author": "Baktash",
"doi-asserted-by": "crossref",
"first-page": "442",
"journal-title": "Postgrad Med J",
"key": "10.1016/j.arcmed.2021.09.006_bib0016",
"volume": "97",
"year": "2021"
},
{
"DOI": "10.1016/j.amsu.2021.102661",
"article-title": "Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India",
"author": "Nimavat",
"doi-asserted-by": "crossref",
"journal-title": "Ann Med Surg",
"key": "10.1016/j.arcmed.2021.09.006_bib0017",
"volume": "68",
"year": "2021"
},
{
"key": "10.1016/j.arcmed.2021.09.006_bib0018",
"unstructured": "COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. Available at https://www.covid19treatmentguidelines.nih.gov/. (Accessed June 22, 2021)."
},
{
"DOI": "10.1056/NEJMp1608005",
"article-title": "Vitamin D Deficiency - Is There Really a Pandemic?",
"author": "Manson",
"doi-asserted-by": "crossref",
"first-page": "1817",
"journal-title": "N Engl J Med",
"key": "10.1016/j.arcmed.2021.09.006_bib0019",
"volume": "375",
"year": "2016"
},
{
"DOI": "10.1016/S2213-8587(16)00079-6",
"article-title": "Towards a trial-based definition of vitamin D deficiency",
"author": "Reid",
"doi-asserted-by": "crossref",
"first-page": "376",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.1016/j.arcmed.2021.09.006_bib0020",
"volume": "4",
"year": "2016"
},
{
"DOI": "10.1002/jbmr.3884",
"article-title": "Vitamin D Metabolism Revised: Fall of Dogmas",
"author": "Bouillon",
"doi-asserted-by": "crossref",
"first-page": "1985",
"journal-title": "J Bone Miner Res",
"key": "10.1016/j.arcmed.2021.09.006_bib0021",
"volume": "34",
"year": "2019"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"article-title": "A new method of classifying prognostic comorbidity in longitudinal studies: development and validation",
"author": "Charlson",
"doi-asserted-by": "crossref",
"first-page": "373",
"journal-title": "J Chronic Dis",
"key": "10.1016/j.arcmed.2021.09.006_bib0022",
"volume": "40",
"year": "1987"
},
{
"key": "10.1016/j.arcmed.2021.09.006_bib0023",
"unstructured": "Vanegas-Cedillo PE, Bello-Chavolla OY, Ramírez-Pedraza N, et al. Serum Vitamin D levels are associated with increased COVID-19 severity and mortality independent of visceral adiposity. medRxiv 2021;52:2021.03.12.21253490. Available from: http://medrxiv.org/content/early/2021/03/14/2021.03.12.21253490. abstract. (Accessed August 30, 2021)."
},
{
"article-title": "The impact of ethnicity on clinical outcomes in COVID-19: A systematic review",
"author": "Pan",
"journal-title": "E Clin Med",
"key": "10.1016/j.arcmed.2021.09.006_bib0024",
"volume": "23",
"year": "2020"
},
{
"key": "10.1016/j.arcmed.2021.09.006_bib0025",
"unstructured": "Horby P, Lim WS, Emberson J, et al. Effect of Dexamethasone in Hospitalized Patients with COVID-19 – Preliminary Report. Prepr medRxiv. Published online 2020. Available from: doi:https://www.medrxiv.org/content/10.1101/2020.06.22.20137273v1.full.pdf. (Accessed August 30, 2021)."
},
{
"DOI": "10.1016/j.coph.2006.03.001",
"article-title": "Angiotensin-converting enzyme 2 in lung diseases",
"author": "Kuba",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Curr Opin Pharmacol",
"key": "10.1016/j.arcmed.2021.09.006_bib0026",
"volume": "6",
"year": "2006"
},
{
"DOI": "10.3390/nu7075111",
"article-title": "Factors affecting 25-hydroxyvitamin D concentration in response to vitamin D supplementation",
"author": "Mazahery",
"doi-asserted-by": "crossref",
"first-page": "5111",
"journal-title": "Nutrients",
"key": "10.1016/j.arcmed.2021.09.006_bib0027",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.1016/j.bbrc.2004.09.073",
"article-title": "Metabolism of vitamin D by human microsomal CYP2R1",
"author": "Shinkyo",
"doi-asserted-by": "crossref",
"first-page": "451",
"journal-title": "Biochem Biophys Res Commun",
"key": "10.1016/j.arcmed.2021.09.006_bib0028",
"volume": "324",
"year": "2004"
},
{
"DOI": "10.2337/db18-1050",
"article-title": "Fasting-induced transcription factors repress Vitamin D bioactivation, a mechanism for Vitamin D deficiency in diabetes",
"author": "Aatsinki",
"doi-asserted-by": "crossref",
"first-page": "918",
"journal-title": "Diabetes",
"key": "10.1016/j.arcmed.2021.09.006_bib0029",
"volume": "68",
"year": "2019"
},
{
"DOI": "10.1002/jbmr.3686",
"article-title": "Obesity Decreases Hepatic 25-Hydroxylase Activity Causing Low Serum 25-Hydroxyvitamin D",
"author": "Roizen",
"doi-asserted-by": "crossref",
"first-page": "1068",
"journal-title": "J Bone Min Res",
"key": "10.1016/j.arcmed.2021.09.006_bib0030",
"volume": "34",
"year": "2019"
},
{
"DOI": "10.1016/j.imbio.2013.10.001",
"article-title": "Circulating complexes of the vitamin D binding protein with G-actin induce lung inflammation by targeting endothelial cells",
"author": "Ge",
"doi-asserted-by": "crossref",
"first-page": "198",
"journal-title": "Immunobiology",
"key": "10.1016/j.arcmed.2021.09.006_bib0031",
"volume": "219",
"year": "2014"
},
{
"DOI": "10.1007/s40520-021-01894-z",
"article-title": "Vitamin D and coronavirus disease 2019 (COVID-19): rapid evidence review",
"author": "Raisi-Estabragh",
"doi-asserted-by": "crossref",
"first-page": "2031",
"journal-title": "Aging Clin Exp Res",
"key": "10.1016/j.arcmed.2021.09.006_bib0032",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1371/annotation/23307aa4-726e-4f11-86c0-8a292be33517",
"article-title": "Determining vitamin D status: A comparison between commercially available assays",
"author": "Snellman",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "PLoS One",
"key": "10.1016/j.arcmed.2021.09.006_bib0033",
"volume": "5",
"year": "2010"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0188440921001983"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Very Low Vitamin D Levels are a Strong Independent Predictor of Mortality in Hospitalized Patients with Severe COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "53"
}
