Impact of Cannabis Use, Substance Use Disorders, and Psychiatric Diagnoses on COVID-19 Outcomes
et al., The Journal of Clinical Psychiatry, doi:10.4088/JCP.21m14332, Aug 2022
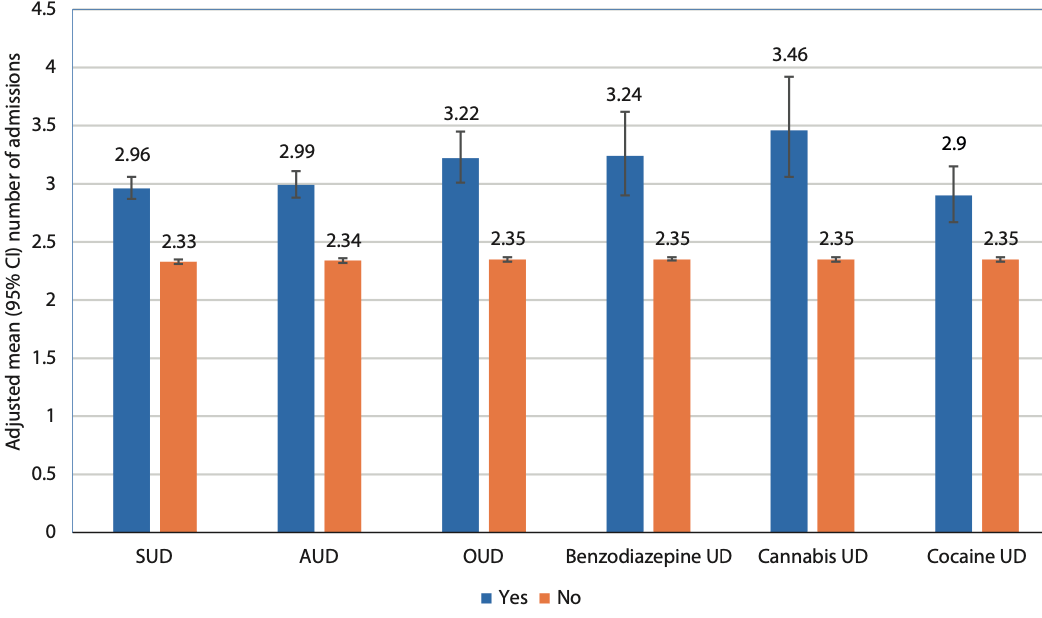
Retrospective 6,291 COVID-19 patients in the USA, showing higher mean hospital admissions and higher maximum length of hospitalization with cannabis use disorder.
Results for cannabis use disorder patients may differ from other use of cannabis.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization, 47.2% higher, RR 1.47, p < 0.001, treatment 20, control 6,271, mean number of admissions.
|
|
hospitalization time, 60.1% higher, relative time 1.60, p = 0.004, treatment 20, control 6,271, maximum length of hospitalization.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ramakrishnan et al., 29 Aug 2022, retrospective, USA, peer-reviewed, 4 authors, study period January 2020 - December 2020.
Contact: rajiv.radhakrishnan@yale.edu.
Impact of Cannabis Use, Substance Use Disorders, and Psychiatric Diagnoses on COVID-19 Outcomes
The Journal of Clinical Psychiatry, doi:10.4088/jcp.21m14332
Early Career Psychiatrists CME Background Articles are selected for credit designation based on an assessment of the educational needs of CME participants, with the purpose of providing readers with a curriculum of CME articles on a variety of topics throughout each volume. Activities are planned using a process that links identified needs with desired results. To obtain credit, read the article, correctly answer the questions in the Posttest, and complete the Evaluation.
CME Objective After studying this article, you should be able to: • Understand which SUDs and other psychiatric patient subgroups may be more susceptible to severe COVID-19 infections and outcomes and better direct needed medical attention to these patients.
Accreditation Statement The CME Institute of Physicians Postgraduate Press, Inc., is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Credit Designation The CME Institute of Physicians Postgraduate Press, Inc., designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Note: The American Nurses Credentialing Center (ANCC) and the American Academy of Physician Assistants (AAPA) accept certificates of participation for educational activities certified for AMA PRA Category 1 Credit™ from organizations accredited by the ACCME.
For reprints or permissions, contact permissions@psychiatrist.com. ♦ © 2022 Copyright Physicians Postgraduate Press, Inc. It is illegal to post this copyrighted PDF on any website.
Posttest To obtain credit, go to CMEInstitute.com to take this Posttest and complete the Evaluation.
References
Allen, Shahawy, Rogers, Association of substance use disorders and drug overdose with adverse COVID-19 outcomes in New York City: January-October 2020, J Public Health (Oxf)
Baillargeon, Polychronopoulou, Kuo, The impact of substance use disorder on COVID-19 outcomes, Psychiatr Serv
Egede, Dawson, Walker, Relationship between mental health diagnoses and COVID-19 test positivity, hospitalization, and mortality in Southeast Wisconsin, Psychol Med, doi:10.1017/S0033291721002312
Fond, Nemani, Etchecopar-Etchart, Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: a systematic review and metaanalysis, JAMA Psychiatry, doi:10.1001/jamapsychiatry.2021.2274
Fond, Pauly, Leone, Disparities in intensive care unit admission and mortality among patients with schizophrenia and COVID-19: a national cohort study, Schizophr Bull
Jeon, Kwon, Park, Association of mental disorders with SARS-CoV-2 infection and severe health outcomes: nationwide cohort study, Br J Psychiatry, doi:10.1192/bjp.2020.251
Lee, Yang, Moon, Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study, Lancet Psychiatry, doi:10.1016/S2215-0366(20)30421-1
Li, Li, Fortunati, Association of a prior psychiatric diagnosis with mortality among hospitalized patients with coronavirus disease 2019 (COVID-19) infection, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.23282
Nemani, Li, Olfson, Association of psychiatric disorders with mortality among patients with COVID-19, JAMA Psychiatry, doi:10.1001/jamapsychiatry.2020.4442
P U B M E D C R O S S R E F ; King, Jt, Yoon, Rentsch, None, doi:10.1080/10826084.2020.1791184
P U B M E D C R O S S R E F, None, doi:10.1002/wps.20806
P U B M E D C R O S S R E F, None, doi:10.1038/s41380-020-00880-7
P U B M E D C R O S S R E F, None, doi:10.1093/schbul/sbaa158
P U B M E D C R O S S R E F, None, doi:10.1176/appi.ps.202000534
Schimmel, Manini, Opioid use disorder and COVID-19: biological plausibility for worsened outcomes, Subst Use Misuse
Vai, Mazza, Colli, Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and metaanalysis, Lancet Psychiatry, doi:10.1016/S2215-0366(21)00232-7
Wang, Kaelber, Xu, COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States, Mol Psychiatry
Wang, Xu, Volkow, Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States, World Psychiatry
DOI record:
{
"DOI": "10.4088/jcp.21m14332",
"ISSN": [
"1555-2101"
],
"URL": "http://dx.doi.org/10.4088/JCP.21m14332",
"author": [
{
"affiliation": [],
"family": "Ramakrishnan",
"given": "Divya",
"sequence": "first"
},
{
"affiliation": [],
"family": "Sureshanand",
"given": "Soundari",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pittman",
"given": "Brian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Radhakrishnan",
"given": "Rajiv",
"sequence": "additional"
}
],
"container-title": "The Journal of Clinical Psychiatry",
"container-title-short": "J. Clin. Psychiatry",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
29
]
],
"date-time": "2022-08-29T13:02:55Z",
"timestamp": 1661778175000
},
"deposited": {
"date-parts": [
[
2022,
8,
29
]
],
"date-time": "2022-08-29T13:02:55Z",
"timestamp": 1661778175000
},
"indexed": {
"date-parts": [
[
2022,
8,
29
]
],
"date-time": "2022-08-29T13:41:42Z",
"timestamp": 1661780502465
},
"is-referenced-by-count": 0,
"issue": "5",
"issued": {
"date-parts": [
[
2022,
8,
29
]
]
},
"journal-issue": {
"issue": "5",
"published-online": {
"date-parts": [
[
2022,
8,
29
]
]
}
},
"member": "2558",
"original-title": [],
"prefix": "10.4088",
"published": {
"date-parts": [
[
2022,
8,
29
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
29
]
]
},
"publisher": "Physicians Postgraduate Press, Inc",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.psychiatrist.com/jcp/covid-19/impact-of-sud-on-covid-19-outcomes/"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Psychiatry and Mental health"
],
"subtitle": [
"A Retrospective Cohort Study"
],
"title": "Impact of Cannabis Use, Substance Use Disorders, and Psychiatric Diagnoses on COVID-19 Outcomes",
"type": "journal-article",
"volume": "83"
}