Decreased serum vitamin D level as a prognostic marker in patients with COVID-19
et al., arXiv, doi:10.48550/arXiv.2301.02660, Dec 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 719 COVID-19 patients in China, showing higher vitamin D levels associated with faster viral clearance and lower severity.
Qu et al., 25 Dec 2022, retrospective, China, peer-reviewed, median age 76.0, 9 authors, study period 13 April, 2022 - 6 June, 2022.
Contact: 22310050@tongji.edu.cn (corresponding author), 2180129@tongji.edu.cn.
Decreased serum vitamin D level as a prognostic marker in patients with COVID-19
Background: The corona virus disease 2019 (COVID-19) pandemic, which is caused by severe acute respiratory syndrome coronavirus 2, is still localized outbreak and has resulted in a high rate of infection and severe disease in older patients with comorbidities. The vitamin D status of the population has been found to be an important factor that could influence outcome of COVID-19. However, whether vitamin D can lessen the symptoms or severity of COVID-19 still remains controversial.
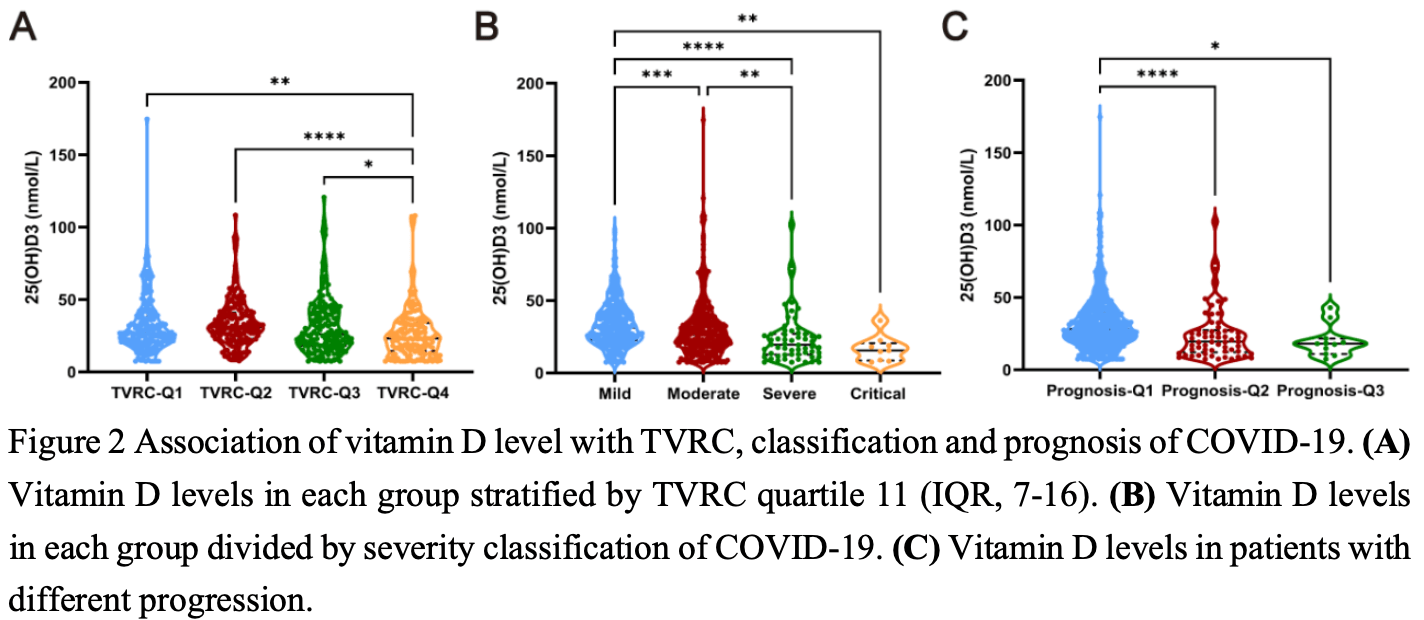
Methods : A total of 719 patients with confirmed COVID-19 were enrolled retrospectively in this study from April 13 to June 6, 2022 at Shanghai Forth People's Hospital. The circulating levels of 25(OH)D3, inflammatory factors, and clinical parameters were assayed. Time to viral RNA clearance (TVRC), classification and prognosis of COVID-19 were used to evaluate the severity of COVID-19 infection. Results: The median age was 76 years (interquartile range, IQR, 64.5-84.6), 44.1% of patients were male, and the TVRC was 11 days (IQR, 7-16) in this population. The median level of 25(OH)D3 was 27.15 (IQR, 19.31-38.89) nmol/L. Patients with lower serum 25(OH)D3 had prolonged time to viral clearance, more obvious inflammatory response, more severe respiratory symptoms and higher risks of impaired hepatic and renal function. Multiple regression analyses revealed that serum 25(OH)D3 level was negatively associated with TVRC independently. ROC curve showed the serum vitamin D level could predict the severity classification and prognosis of COVID-19 significantly. Conclusions: Serum 25(OH)D3 level is independently associated with the severity of COVID-19 in elderly, and it could be used as a predictor of the severity of COVID-19. In addition, supplementation with vitamin D might provide beneficial effects in old patients with COVID-19.
Conflicts of Interest The authors declare no conflict of interest.
References
Amrein, Vitamin D deficiency 2.0: an update on the current status worldwide, Eur J Clin Nutr
Angelidi, Vitamin D Status Is Associated With In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients, Mayo Clin Proc
Bychinin, Effect of vitamin D3 supplementation on cellular immunity and inflammatory markers in COVID-19 patients admitted to the ICU, Sci Rep
Gibbons, Association between vitamin D supplementation and COVID-19 infection and mortality, Sci Rep
Heaney, Vitamin D in health and disease, Clin J Am Soc Nephrol
Holick, Vitamin D and sunlight: strategies for cancer prevention and other health benefits, Clin J Am Soc Nephrol
Hossein-Nezhad, Holick, Vitamin D for health: a global perspective, Mayo Clin Proc
Jolliffe, Effect of a test-and-treat approach to vitamin D supplementation on risk of all cause acute respiratory tract infection and covid-19: phase 3 randomised controlled trial (CORONAVIT), BMJ
Jose, Manuel, COVID-19 cytokine storm: the interplay between inflammation and coagulation, The Lancet Respiratory Medicine
Jurutka, The polymorphic N terminus in human vitamin D receptor isoforms influences transcriptional activity by modulating interaction with transcription factor IIB, Mol Endocrinol
Kaufman, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One
Laplana, Royo, Fibla, Vitamin D Receptor polymorphisms and risk of enveloped virus infection: A meta-analysis, Gene
Liang, Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China, The Lancet Oncology
Lips, Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society, Eur J Endocrinol
Liu, Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response, Science
Looker, Serum 25-hydroxyvitamin D status of adolescents and adults in two seasonal subpopulations from NHANES III, Bone
Mangin, Sinha, Fincher, Inflammation and vitamin D: the infection connection, Inflamm Res
Martineau, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ
Mcgonagle, The Role of Cytokines including Interleukin-6 in COVID-19 induced Pneumonia and Macrophage Activation Syndrome-Like Disease, Autoimmun Rev
Mitchell, Vitamin-D and COVID-19: do deficient risk a poorer outcome?, The Lancet Diabetes & Endocrinology
Perico, Immunity, endothelial injury and complement-induced coagulopathy in COVID-19, Nat Rev Nephrol
Pludowski, Vitamin D supplementation guidelines, J Steroid Biochem Mol Biol
Pranata, Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: A systematic review, meta-analysis and meta-regression, J Renin Angiotensin Aldosterone Syst
Rastogi, Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (SHADE study), Postgrad Med J
Rook, Vitamin D3, gamma interferon, and control of proliferation of Mycobacterium tuberculosis by human monocytes, Immunology
Roy, Independent association of severe vitamin D deficiency as a risk of acute myocardial infarction in Indians, Indian Heart J
Shi, Vitamin D/VDR signaling attenuates lipopolysaccharideinduced acute lung injury by maintaining the integrity of the pulmonary epithelial barrier, Mol Med Rep
Singh, Microstructure, pathophysiology, and potential therapeutics of COVID-19: A comprehensive review, J Med Virol
Szeto, Vitamin D Status and COVID-19 Clinical Outcomes in Hospitalized Patients, Endocr Res
Thacher, Clarke, Vitamin D insufficiency, Mayo Clin Proc
Wielen, Serum vitamin D concentrations among elderly people in Europe, Lancet
Zhen, Serum vitamin D levels of the natural population in eastern China, Chinese Journal of Endocrinology and Metabolism
Zhou, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, The Lancet
Zhu, Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes, Cell Metab
DOI record:
{
"DOI": "10.48550/ARXIV.2301.02660",
"URL": "https://arxiv.org/abs/2301.02660",
"abstract": "Background: The corona virus disease 2019 (COVID-19) pandemic, which is caused by severe acute respiratory syndrome coronavirus 2, is still localized outbreak and has resulted in a high rate of infection and severe disease in older patients with comorbidities. The vitamin D status of the population has been found to be an important factor that could influence outcome of COVID-19. However, whether vitamin D can lessen the symptoms or severity of COVID-19 still remains controversial. Methods: A total of 719 patients with confirmed COVID-19 were enrolled retrospectively in this study from April 13 to June 6, 2022 at Shanghai Forth People's Hospital. The circulating levels of 25(OH)D3, inflammatory factors, and clinical parameters were assayed. Time to viral RNA clearance (TVRC), classification and prognosis of COVID-19 were used to evaluate the severity of COVID-19 infection. Results: The median age was 76 years (interquartile range, IQR, 64.5-84.6), 44.1% of patients were male, and the TVRC was 11 days (IQR, 7-16) in this population. The median level of 25(OH)D3 was 27.15 (IQR, 19.31-38.89) nmol/L. Patients with lower serum 25(OH)D3 had prolonged time to viral clearance, more obvious inflammatory response, more severe respiratory symptoms and higher risks of impaired hepatic and renal function. Multiple regression analyses revealed that serum 25(OH)D3 level was negatively associated with TVRC independently. ROC curve showed the serum vitamin D level could predict the severity classification and prognosis of COVID-19 significantly.Conclusions: Serum 25(OH)D3 level is independently associated with the severity of COVID-19 in elderly, and it could be used as a predictor of the severity of COVID-19. In addition, supplementation with vitamin D might provide beneficial effects in old patients with COVID-19.",
"author": [
{
"family": "Qu",
"given": "Ruyi"
},
{
"family": "Yang",
"given": "Qiuji"
},
{
"family": "Bi",
"given": "Yingying"
},
{
"family": "Cheng",
"given": "Jiajing"
},
{
"family": "He",
"given": "Mengna"
},
{
"family": "Wei",
"given": "Xin"
},
{
"family": "Yuan",
"given": "Yiqi"
},
{
"family": "Yang",
"given": "Yuxin"
},
{
"family": "Qin",
"given": "Jinlong"
}
],
"categories": [
"Tissues and Organs (q-bio.TO)",
"FOS: Biological sciences",
"FOS: Biological sciences"
],
"copyright": "Creative Commons Attribution 4.0 International",
"id": "https://doi.org/10.48550/arxiv.2301.02660",
"issued": {
"date-parts": [
[
2023
]
]
},
"publisher": "arXiv",
"title": "Decreased serum vitamin D level as a prognostic marker in patients with COVID-19",
"type": "article",
"version": "1"
}
