Estimating the effect of realistic improvements of metformin adherence on COVID-19 mortality using targeted machine learning
et al., Global Epidemiology, doi:10.1016/j.gloepi.2024.100142, Mar 2024
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 61,180 COVID-19 positive patients with chronic metformin prescriptions showing lower COVID-19 mortality with improved metformin adherence, as measured by proportion of days covered.
Qiu et al., 30 Mar 2024, retrospective, Mexico, peer-reviewed, 8 authors, study period 4 October, 2020 - 29 May, 2021.
Estimating the effect of realistic improvements of metformin adherence on COVID-19 mortality using targeted machine learning
Global Epidemiology, doi:10.1016/j.gloepi.2024.100142
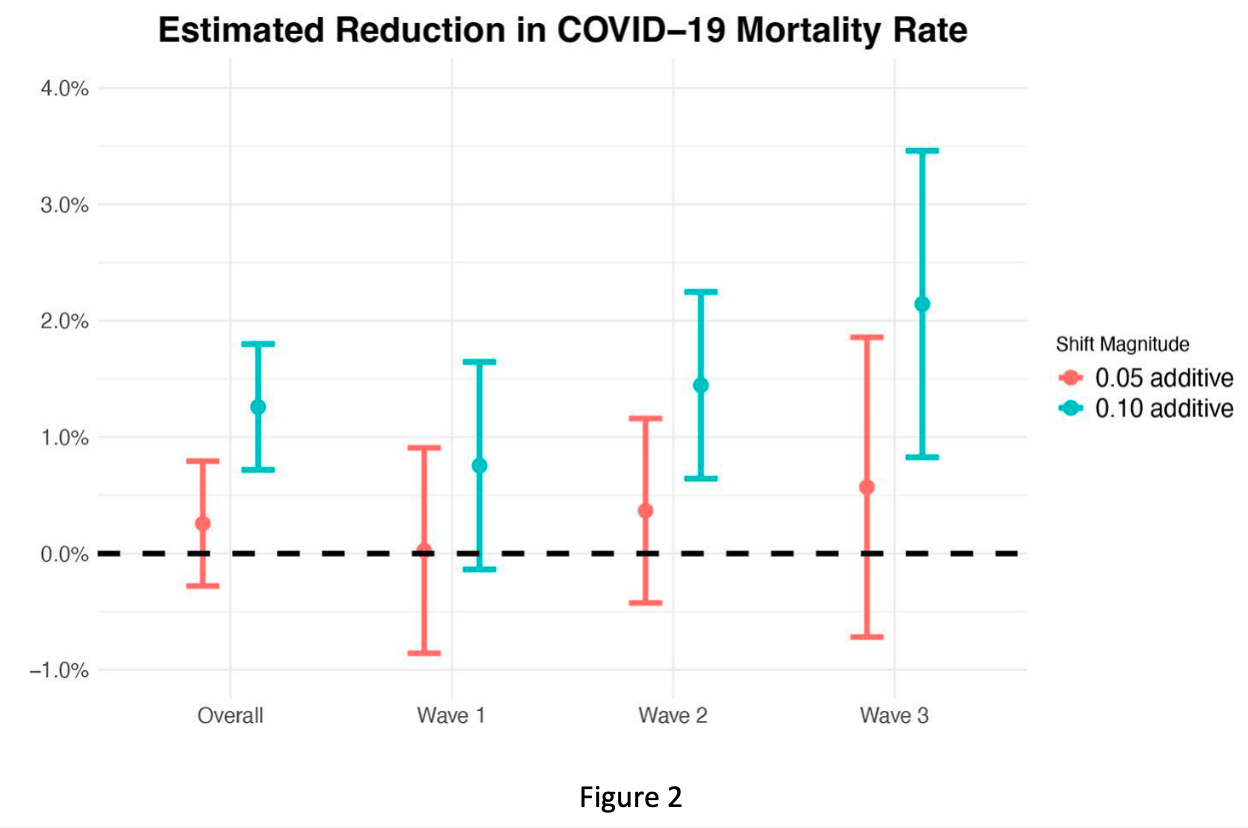
Background: Type 2 diabetes elevates the risk of severe outcomes in COVID-19 patients, with multiple studies reporting higher case fatality rates. Metformin is a widely used medication for glycemic management. We hypothesize that improved adherence to metformin may lower COVID-19 post-infection mortality risk in this group. Utilizing data from the Mexican Social Security Institute (IMSS), we investigate the relationship between metformin adherence and mortality following COVID-19 infection in patients with chronic metformin prescriptions. Methods: This is a retrospective cohort study consisting of 61,180 IMSS beneficiaries who received a positive polymerase chain reaction (PCR) or rapid test for SARS-CoV-2 and had at least two consecutive months of metformin prescriptions prior to the positive test. The hypothetical intervention is improved adherence to metformin, measured by proportion of days covered (PDC), with the comparison being the observed metformin adherence values. The primary outcome is all-cause mortality following COVID-19 infection. We defined the causal parameter using shift intervention, an example of modified treatment policies. We used the targeted learning framework for estimation of the target estimand. Findings: Among COVID-19 positive patients with chronic metformin prescriptions, we found that a 5% and 10% absolute increase in metformin adherence is associated with a respective 0.26% (95% CI: -0.28%, 0.79%) and 1.26% (95% CI: 0.72%, 1.80%) absolute decrease in mortality risk. Interpretation: Subject to the limitations of a real-world data study, our results indicate a causal association between improved metformin adherence and reduced COVID-19 postinfection mortality risk.
Declaration of interests ☒ The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. ☐ The author is an Editorial Board Member/Editor-in-Chief/Associate Editor/Guest Editor for [Journal name] and was not involved in the editorial review or the decision to publish this article. ☐ The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
References
Ascencio-Montiel, Od, Pacheco, Comparative epidemiology of five waves of COVID-19 in Mexico, March 2020-August 2022, BMC infectious diseases
Barron, Bakhai, Kar, Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study, The Lancet Diabetes & Endocrinology
Baumgartner, Haynes, Hersberger, Arnet, A Systematic review of medication adherence thresholds dependent of clinical outcomes, Frontiers in pharmacology
Bautista-González, Werner-Sunderland, Mp, Health-care guidelines and policies during the COVID-19 pandemic in Mexico: a case of health inequalities, Health Policy OPEN
Bezie, Molina, Hernandez, Batista, Niang et al., Therapeutic compliance: a prospective analysis of various factors involved in the adherence rate in type 2 diabetes, Diabetes & metabolism
Bode, Garrett, Messler, Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States Journal of diabetes science and technology
Bramante, Buse, Liebovitz, Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10 months (COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial, The Lancet infectious diseases
Bramante, Huling, Tignanelli, Randomized trial of Metformin, Ivermectin, and Fluvoxamine for COVID-19, New England Journal of Medicine
Cooray, Tsakos, Heilmann, Impact of teeth on social participation: modified treatment policy approach, Journal of dental research
Denicolo, Perco, Thoeni, Mayer, Non-adherence to antidiabetic and cardiovascular drugs in type 2 diabetes mellitus and its association with renal and cardiovascular outcomes: a narrative review, Journal of diabetes and its complications
Díaz, Williams, Hoffman, Schenck, Nonparametric causal effects based on longitudinal modified treatment policies, Journal of the American Statistical Association
Egede, Lynch, Gebregziabher, Differential Impact of Longitudinal Medication Non-Adherence on Mortality by Race/Ethnicity among Veterans with Diabetes Journal of general internal medicine, JGIM
Gatwood, Chisholm-Burns, Differences in health outcomes associated with initial adherence to oral antidiabetes medications among veterans with uncomplicated type 2 diabetes: a 5-year survival analysis, Diabetic medicine
Gutiérrez, Bertozzi, Non-communicable diseases and inequalities increase risk of death among COVID-19 patients in Mexico, PloS one
Gutiérrez, López, Ascencio, Changes in the epidemiological profile of SARS-CoV-2-positive individuals in Mexico across pandemic waves as an explanation of fatality reduction: a retrospective observational study, BMJ open
Haneuse, Rotnitzky, Estimation of the effect of interventions that modify the received treatment, Statistics in medicine
Hejazi, Benkeser, Díaz, Van Der Laan, Efficient estimation of modified treatment policy effects based on the generalized propensity score
Hejazi, Coyle, Van Der Laan, tmle3shift: Targeted Learning of the Causal Effects of Stochastic Interventions
Hill-Briggs, Adler, Berkowitz, Social determinants of health and diabetes: A scientific review, Diabetes care
Ho, Rumsfeld, Masoudi, Effect of Medication Nonadherence on Hospitalization and Mortality Among Patients With Diabetes Mellitus, Archives of internal medicine
Hoffman, Salazar-Barreto, Rudolph, Díaz, Introducing longitudinal modified treatment policies: a unified framework for studying complex exposures
Hong, Kang, Relationship between oral antihyperglycemic medication adherence and hospitalization, mortality, and healthcare costs in adult ambulatory care patients with type 2 diabetes in South Korea, Medical care
Iuga, Mcguire, Adherence and health care costs, Risk Management and Healthcare Policy
J O U R N A L P R E, None
J O U R N A L P R E, p r o o f Journal Pre-proof
J O U R N A L P R E, p r o o f Journal Pre-proof
Juárez-Flores, Ascencio-Montiel, Gutiérrez, COVID-19 in the Mexican Social Security Institute (IMSS) population. Prevalent symptoms
Kim, Lee, Kang, Park, Effect of medication adherence on long-term allcause-mortality and hospitalization for cardiovascular disease in 65,067 newly diagnosed type 2 diabetes patients, Scientific Reports
Li, Yang, Yan, Sun, Zeng et al., Metformin in patients with COVID-19: a systematic review and meta-analysis, Frontiers in medicine
Liao, Hubbard, Gutiérrez, Who is most at risk of dying if infected with SARS-CoV-2? A mortality risk factor analysis using machine learning of patients with COVID-19 over time: a large population-based cohort study in Mexico, BMJ open
Muñoz, Der Laan, Population intervention causal effects based on stochastic interventions, Biometrics
Nugent, Balzer, A demonstration of modified treatment policies to evaluate shifts in mobility and COVID-19 case rates in US counties, American journal of epidemiology
Osterberg, Blaschke, Adherence to medication, The New England Journal of Medicine
Parthasarathy, Tandel, Siddiqui, Harshan, Metformin suppresses SARS-CoV-2 in cell culture, Virus research
Petersen, Porter, Gruber, Wang, Van Der Laan, Diagnosing and responding to violations in the positivity assumption, Statistical methods in medical research
Raebel, Schmittdiel, Karter, Konieczny, Steiner, Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases, Medical care
Rawshani, Kjölhede, Rawshani, Severe COVID-19 in people with type 1 and type 2 diabetes in Sweden: A nationwide retrospective cohort study, The Lancet regional health
Reis, Silva, Silva, Effect of early treatment with metformin on risk of emergency care and hospitalization among patients with COVID-19: the TOGETHER randomized platform clinical trial, Lancet Regional Health. Americas
Rhee, Herrick, Ziemer, Many americans have pre-diabetes and should be considered for metformin therapy, Diabetes Care
Rojas, Gomes, Metformin: an old but still the best treatment for type 2 diabetes, Diabetology & Metabolic Syndrome
Rubin, Causal inference using potential outcomes: design, modeling, decisions, Journal of the American Statistical Association
Samuel, Varghese, Büsselberg, Therapeutic Potential of Metformin in COVID-19: Reasoning for Its Protective Role, Trends in microbiology
Simard, Presse, Roy, Association between metformin adherence and allcause mortality among new users of metformin: a nested case-control study, The Annals of pharmacotherapy
Troughton, Felker, Januzzi, Natriuretic peptide-guided heart failure management, European heart journal
Van Der Laan, Daniel, Targeted Maximum Likelihood Learning The International, Journal of Biostatistics
Van Der Laan, Polley, Hubbard, Super Learner Statistical Applications in, Genetics and Molecular Biology
Van Der Laan, Rose, Targeted learning in data science: causal inference for complex longitudinal studies
Van Der Laan, Rose, Targeted learning: causal inference for observational and experimental data
DOI record:
{
"DOI": "10.1016/j.gloepi.2024.100142",
"ISSN": [
"2590-1133"
],
"URL": "http://dx.doi.org/10.1016/j.gloepi.2024.100142",
"alternative-id": [
"S2590113324000087"
],
"article-number": "100142",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Estimating the effect of realistic improvements of metformin adherence on COVID-19 mortality using targeted machine learning"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Global Epidemiology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.gloepi.2024.100142"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2024 The Authors. Published by Elsevier Inc."
}
],
"author": [
{
"affiliation": [],
"family": "Qiu",
"given": "Sky",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hubbard",
"given": "Alan E.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gutiérrez",
"given": "Juan Pablo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pimpale",
"given": "Ganesh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Juárez-Flores",
"given": "Arturo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ghosh",
"given": "Rakesh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "de Jesús Ascencio-Montiel",
"given": "Iván",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bertozzi",
"given": "Stefano M.",
"sequence": "additional"
}
],
"container-title": "Global Epidemiology",
"container-title-short": "Global Epidemiology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2024,
3,
30
]
],
"date-time": "2024-03-30T16:49:00Z",
"timestamp": 1711817340000
},
"deposited": {
"date-parts": [
[
2024,
3,
30
]
],
"date-time": "2024-03-30T17:37:11Z",
"timestamp": 1711820231000
},
"funder": [
{
"DOI": "10.13039/100000865",
"doi-asserted-by": "publisher",
"name": "Bill & Melinda Gates Foundation"
},
{
"DOI": "10.13039/100020457",
"doi-asserted-by": "publisher",
"name": "C3.ai Digital Transformation Institute"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
31
]
],
"date-time": "2024-03-31T00:39:18Z",
"timestamp": 1711845558482
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
3
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
3,
1
]
],
"date-time": "2024-03-01T00:00:00Z",
"timestamp": 1709251200000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 26,
"start": {
"date-parts": [
[
2024,
3,
27
]
],
"date-time": "2024-03-27T00:00:00Z",
"timestamp": 1711497600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2590113324000087?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2590113324000087?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "100142",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2024,
3
]
]
},
"published-print": {
"date-parts": [
[
2024,
3
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"article-title": "Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study",
"author": "Barron",
"doi-asserted-by": "crossref",
"first-page": "813",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.1016/j.gloepi.2024.100142_bb0005",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1177/1932296820924469",
"article-title": "Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States",
"author": "Bode",
"doi-asserted-by": "crossref",
"first-page": "813",
"journal-title": "J Diabetes Sci Technol",
"key": "10.1016/j.gloepi.2024.100142_bb0010",
"volume": "14",
"year": "2020"
},
{
"article-title": "Severe COVID-19 in people with type 1 and type 2 diabetes in Sweden: a nationwide retrospective cohort study",
"author": "Rawshani",
"journal-title": "Lancet Reg Health Eur",
"key": "10.1016/j.gloepi.2024.100142_bb0015",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1136/bmjopen-2023-072436",
"article-title": "Who is most at risk of dying if infected with SARS-CoV-2? A mortality risk factor analysis using machine learning of patients with COVID-19 over time: a large population-based cohort study in Mexico",
"author": "Liao",
"doi-asserted-by": "crossref",
"journal-title": "BMJ Open",
"key": "10.1016/j.gloepi.2024.100142_bb0020",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1371/journal.pone.0240394",
"article-title": "Non-communicable diseases and inequalities increase risk of death among COVID-19 patients in Mexico",
"author": "Gutiérrez",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "10.1016/j.gloepi.2024.100142_bb0025",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1001/archinte.166.17.1836",
"article-title": "Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus",
"author": "Ho",
"doi-asserted-by": "crossref",
"first-page": "1836",
"issue": "166",
"journal-title": "Arch Intern Med (1960)",
"key": "10.1016/j.gloepi.2024.100142_bb0030",
"year": "2006"
},
{
"DOI": "10.1097/MLR.0b013e31820292d1",
"article-title": "Relationship between oral antihyperglycemic medication adherence and hospitalization, mortality, and healthcare costs in adult ambulatory care patients with type 2 diabetes in South Korea",
"author": "Hong",
"doi-asserted-by": "crossref",
"first-page": "378",
"journal-title": "Med Care",
"key": "10.1016/j.gloepi.2024.100142_bb0035",
"volume": "49",
"year": "2011"
},
{
"DOI": "10.1007/s11606-012-2200-8",
"article-title": "Differential impact of longitudinal medication non-adherence on mortality by race/ethnicity among veterans with diabetes",
"author": "Egede",
"doi-asserted-by": "crossref",
"first-page": "208",
"journal-title": "J General Internal Med: JGIM",
"key": "10.1016/j.gloepi.2024.100142_bb0040",
"volume": "28",
"year": "2013"
},
{
"DOI": "10.1111/dme.13775",
"article-title": "Differences in health outcomes associated with initial adherence to oral antidiabetes medications among veterans with uncomplicated type 2 diabetes: a 5-year survival analysis",
"author": "Gatwood",
"doi-asserted-by": "crossref",
"journal-title": "Diabet Med",
"key": "10.1016/j.gloepi.2024.100142_bb0045",
"volume": "35",
"year": "2018"
},
{
"DOI": "10.1038/s41598-018-30740-y",
"article-title": "Effect of medication adherence on long-term allcause-mortality and hospitalization for cardiovascular disease in 65,067 newly diagnosed type 2 diabetes patients",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "12190",
"journal-title": "Sci Rep",
"key": "10.1016/j.gloepi.2024.100142_bb0050",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1177/1060028017743517",
"article-title": "Association between metformin adherence and allcause mortality among new users of metformin: a nested case-control study",
"author": "Simard",
"doi-asserted-by": "crossref",
"first-page": "305",
"journal-title": "Ann Pharmacother",
"key": "10.1016/j.gloepi.2024.100142_bb0055",
"volume": "52",
"year": "2018"
},
{
"DOI": "10.1016/j.tim.2021.03.004",
"article-title": "Therapeutic potential of metformin in COVID-19: reasoning for its protective role",
"author": "Samuel",
"doi-asserted-by": "crossref",
"first-page": "894",
"journal-title": "Trends Microbiol (Regul ed)",
"key": "10.1016/j.gloepi.2024.100142_bb0060",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1016/j.virusres.2022.199010",
"article-title": "Metformin suppresses SARS-CoV-2 in cell culture",
"author": "Parthasarathy",
"doi-asserted-by": "crossref",
"journal-title": "Virus Res",
"key": "10.1016/j.gloepi.2024.100142_bb0065",
"volume": "323",
"year": "2023"
},
{
"DOI": "10.1016/S1262-3636(07)70316-6",
"article-title": "Therapeutic compliance: a prospective analysis of various factors involved in the adherence rate in type 2 diabetes",
"author": "Bezie",
"doi-asserted-by": "crossref",
"first-page": "611",
"journal-title": "Diabetes Metab",
"key": "10.1016/j.gloepi.2024.100142_bb0070",
"volume": "32",
"year": "2006"
},
{
"article-title": "Adherence and health care costs",
"author": "Iuga",
"first-page": "35",
"journal-title": "Risk ManageHealthcare Policy",
"key": "10.1016/j.gloepi.2024.100142_bb0075",
"volume": "7",
"year": "2014"
},
{
"DOI": "10.2337/dci20-0053",
"article-title": "Social determinants of health and diabetes: a scientific review",
"author": "Hill-Briggs",
"doi-asserted-by": "crossref",
"first-page": "258",
"journal-title": "Diabetes Care",
"key": "10.1016/j.gloepi.2024.100142_bb0080",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.2202/1557-4679.1043",
"doi-asserted-by": "crossref",
"key": "10.1016/j.gloepi.2024.100142_bb0085",
"unstructured": "van der Laan MJ, Rubin Daniel. Targeted maximum likelihood learning Int J Biostat 2006;2:11-."
},
{
"DOI": "10.2202/1544-6115.1309",
"article-title": "Super learner",
"author": "van der Laan",
"doi-asserted-by": "crossref",
"journal-title": "Stat Appl Genet Mol Biol",
"key": "10.1016/j.gloepi.2024.100142_bb0090",
"volume": "6",
"year": "2007"
},
{
"DOI": "10.1007/978-1-4419-9782-1",
"article-title": "Targeted learning: causal inference for observational and experimental data",
"author": "van der Laan",
"doi-asserted-by": "crossref",
"journal-title": "Spring Ser Statist",
"key": "10.1016/j.gloepi.2024.100142_bb0095",
"year": "2011"
},
{
"author": "van der Laan",
"key": "10.1016/j.gloepi.2024.100142_bb0100",
"series-title": "Targeted learning in data science: Causal inference for complex longitudinal studies. Springer series in statistics",
"year": "2018"
},
{
"article-title": "COVID-19 in the Mexican Social Security Institute (IMSS) population. Prevalent symptoms",
"author": "Juárez-Flores",
"journal-title": "medRxiv",
"key": "10.1016/j.gloepi.2024.100142_bb0105",
"year": "2022"
},
{
"DOI": "10.1186/s12879-022-07800-w",
"article-title": "Comparative epidemiology of five waves of COVID-19 in Mexico, March 2020–August 2022",
"author": "Ascencio-Montiel",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "BMC Infect Dis",
"key": "10.1016/j.gloepi.2024.100142_bb0110",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1056/NEJMra050100",
"article-title": "Adherence to medication",
"author": "Osterberg",
"doi-asserted-by": "crossref",
"first-page": "487",
"journal-title": "N Engl J Med",
"key": "10.1016/j.gloepi.2024.100142_bb0115",
"volume": "353",
"year": "2005"
},
{
"DOI": "10.1097/MLR.0b013e31829b1d2a",
"article-title": "Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases",
"author": "Raebel",
"doi-asserted-by": "crossref",
"first-page": "S11",
"journal-title": "Med Care",
"key": "10.1016/j.gloepi.2024.100142_bb0120",
"volume": "51",
"year": "2013"
},
{
"author": "Pharmacy Quality Alliance Adherence Measures",
"key": "10.1016/j.gloepi.2024.100142_bb0125"
},
{
"DOI": "10.3389/fphar.2018.01290",
"article-title": "A systematic review of medication adherence thresholds dependent of clinical outcomes",
"author": "Baumgartner",
"doi-asserted-by": "crossref",
"first-page": "1290",
"journal-title": "Front Pharmacol",
"key": "10.1016/j.gloepi.2024.100142_bb0130",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1177/0962280210386207",
"article-title": "Diagnosing and responding to violations in the positivity assumption",
"author": "Petersen",
"doi-asserted-by": "crossref",
"first-page": "31",
"journal-title": "Stat Methods Med Res",
"key": "10.1016/j.gloepi.2024.100142_bb0135",
"volume": "21",
"year": "2012"
},
{
"DOI": "10.1111/j.1541-0420.2011.01685.x",
"article-title": "Population intervention causal effects based on stochastic interventions",
"author": "Muñoz",
"doi-asserted-by": "crossref",
"first-page": "541",
"journal-title": "Biometrics",
"key": "10.1016/j.gloepi.2024.100142_bb0140",
"volume": "68",
"year": "2012"
},
{
"DOI": "10.1002/sim.5907",
"article-title": "Estimation of the effect of interventions that modify the received treatment",
"author": "Haneuse",
"doi-asserted-by": "crossref",
"first-page": "5260",
"journal-title": "Stat Med",
"key": "10.1016/j.gloepi.2024.100142_bb0145",
"volume": "32",
"year": "2013"
},
{
"DOI": "10.1093/aje/kwad005",
"article-title": "A demonstration of modified treatment policies to evaluate shifts in mobility and COVID-19 case rates in US counties",
"author": "Nugent",
"doi-asserted-by": "crossref",
"first-page": "762",
"journal-title": "Am J Epidemiol",
"key": "10.1016/j.gloepi.2024.100142_bb0150",
"volume": "192",
"year": "2023"
},
{
"author": "Hejazi",
"key": "10.1016/j.gloepi.2024.100142_bb0155"
},
{
"DOI": "10.1198/016214504000001880",
"article-title": "Causal inference using potential outcomes: design, modeling, decisions",
"author": "Rubin",
"doi-asserted-by": "crossref",
"first-page": "322",
"journal-title": "J Am Stat Assoc",
"key": "10.1016/j.gloepi.2024.100142_bb0160",
"volume": "100",
"year": "2005"
},
{
"DOI": "10.1016/j.hpopen.2020.100025",
"article-title": "Health-care guidelines and policies during the COVID-19 pandemic in Mexico: a case of health inequalities",
"author": "Bautista-González",
"doi-asserted-by": "crossref",
"journal-title": "Health Policy OPEN",
"key": "10.1016/j.gloepi.2024.100142_bb0165",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1080/01621459.2021.1955691",
"article-title": "Nonparametric causal effects based on longitudinal modified treatment policies",
"author": "Díaz",
"doi-asserted-by": "crossref",
"first-page": "846",
"journal-title": "J Am Stat Assoc",
"key": "10.1016/j.gloepi.2024.100142_bb0170",
"volume": "118",
"year": "2023"
},
{
"author": "Hejazi",
"key": "10.1016/j.gloepi.2024.100142_bb0175",
"series-title": "Efficient estimation of modified treatment policy effects based on the generalized propensity score",
"year": "2022"
},
{
"author": "Hoffman",
"key": "10.1016/j.gloepi.2024.100142_bb0180",
"series-title": "Introducing longitudinal modified treatment policies: A unified framework for studying complex exposures",
"year": "2023"
},
{
"DOI": "10.1177/00220345231164106",
"article-title": "Impact of teeth on social participation: modified treatment policy approach",
"author": "Cooray",
"doi-asserted-by": "crossref",
"journal-title": "J Dent Res",
"key": "10.1016/j.gloepi.2024.100142_bb0185",
"year": "2023"
},
{
"DOI": "10.1136/bmjopen-2022-063211",
"article-title": "Changes in the epidemiological profile of SARS-CoV-2-positive individuals in Mexico across pandemic waves as an explanation of fatality reduction: a retrospective observational study",
"author": "Gutiérrez",
"doi-asserted-by": "crossref",
"journal-title": "BMJ Open",
"key": "10.1016/j.gloepi.2024.100142_bb0190",
"volume": "13",
"year": "2023"
},
{
"article-title": "Metformin in patients with COVID-19: a systematic review and meta-analysis",
"author": "Li",
"journal-title": "Front Med",
"key": "10.1016/j.gloepi.2024.100142_bb0195",
"volume": "8",
"year": "2021"
},
{
"article-title": "Effect of early treatment with metformin on risk of emergency care and hospitalization among patients with COVID-19: the TOGETHER randomized platform clinical trial",
"author": "Reis",
"journal-title": "Lancet Reg Health Am",
"key": "10.1016/j.gloepi.2024.100142_bb0200",
"volume": "6",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2201662",
"article-title": "Randomized trial of metformin, Ivermectin, and fluvoxamine for COVID-19",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "599",
"journal-title": "N Engl J Med",
"key": "10.1016/j.gloepi.2024.100142_bb0205",
"volume": "387",
"year": "2022"
},
{
"DOI": "10.1016/S1473-3099(23)00299-2",
"article-title": "Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10 months (COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "1119",
"journal-title": "Lancet Infect Dis",
"key": "10.1016/j.gloepi.2024.100142_bb0210",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.2337/dc09-0341",
"article-title": "Many americans have pre-diabetes and should be considered for metformin therapy",
"author": "Rhee",
"doi-asserted-by": "crossref",
"first-page": "49",
"journal-title": "Diabetes Care",
"key": "10.1016/j.gloepi.2024.100142_bb0215",
"volume": "33",
"year": "2010"
},
{
"DOI": "10.1186/1758-5996-5-6",
"article-title": "Metformin: an old but still the best treatment for type 2 diabetes",
"author": "Rojas",
"doi-asserted-by": "crossref",
"first-page": "6",
"journal-title": "Diabetol Metab Syndr",
"key": "10.1016/j.gloepi.2024.100142_bb0220",
"volume": "5",
"year": "2013"
},
{
"DOI": "10.1016/j.jdiacomp.2021.107931",
"article-title": "Non-adherence to antidiabetic and cardiovascular drugs in type 2 diabetes mellitus and its association with renal and cardiovascular outcomes: a narrative review",
"author": "Denicolo",
"doi-asserted-by": "crossref",
"journal-title": "J Diabetes Complicat",
"key": "10.1016/j.gloepi.2024.100142_bb0225",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1093/eurheartj/eht463",
"article-title": "Natriuretic peptide-guided heart failure management",
"author": "Troughton",
"doi-asserted-by": "crossref",
"first-page": "16",
"journal-title": "Eur Heart J",
"key": "10.1016/j.gloepi.2024.100142_bb0230",
"volume": "35",
"year": "2014"
}
],
"reference-count": 46,
"references-count": 46,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2590113324000087"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Public Health, Environmental and Occupational Health",
"Epidemiology"
],
"subtitle": [],
"title": "Estimating the effect of realistic improvements of metformin adherence on COVID-19 mortality using targeted machine learning",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}
