Low vitamin D levels and increased neutrophil in patients admitted at ICU with COVID-19
et al., Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.05.021, May 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
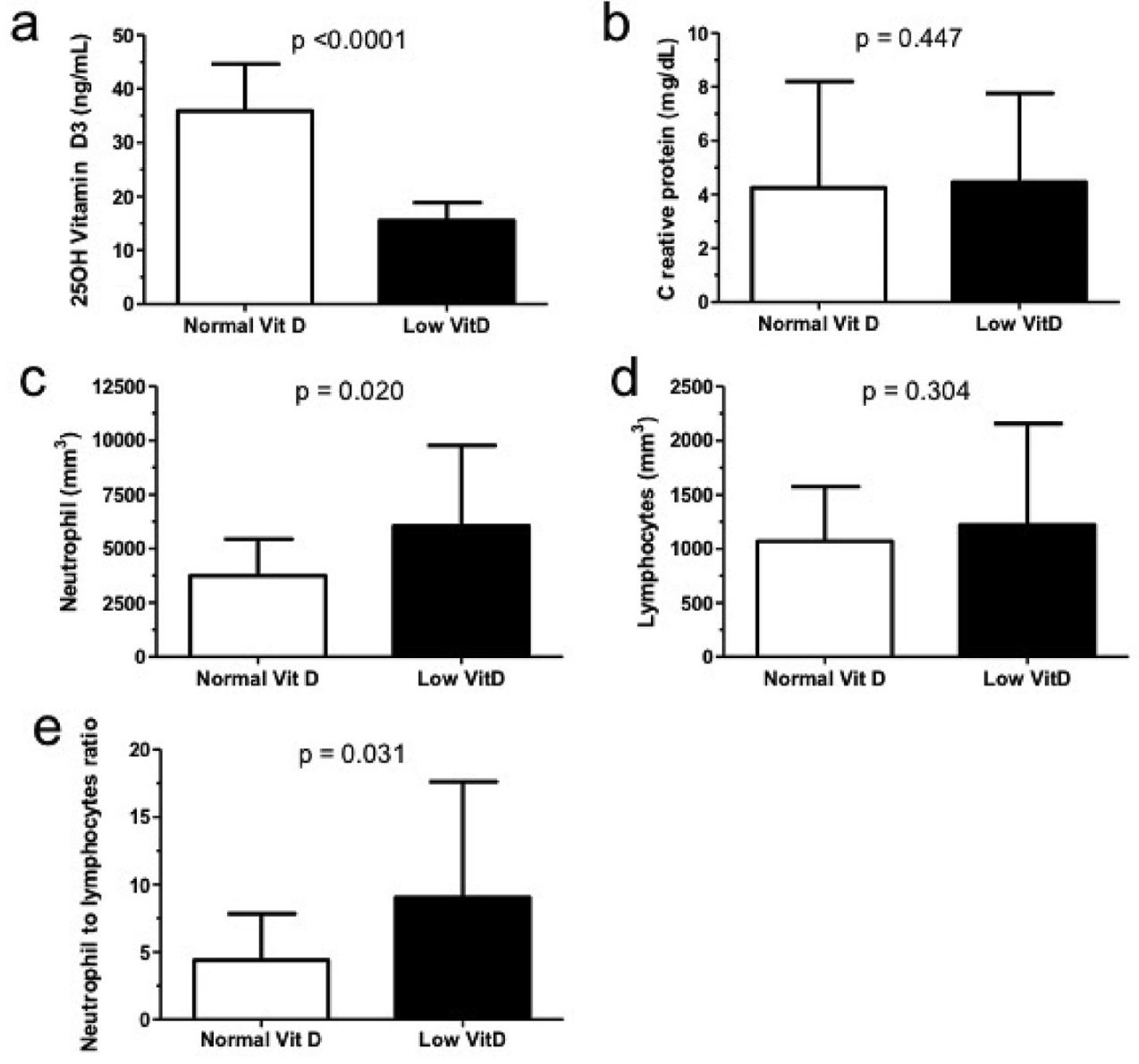
Retrospective 25 ICU patients in Brazil, showing vitamin D deficiency associated with higher neutrophil-lymphocyte ratio. There appears to be a typo in the mortality percentage for vitamin D deficiency (20% is not valid for the group size of 8).
This is the 70th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 29.4% lower, RR 0.71, p = 1.00, high D levels 3 of 17 (17.6%), low D levels 2 of 8 (25.0%), NNT 14, >20ng/mL.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Pimental et al., 31 May 2021, retrospective, Brazil, peer-reviewed, 3 authors.
Low vitamin D levels and increased neutrophil in patients admitted at ICU with COVID-19
Clinical Nutrition ESPEN, doi:10.1016/j.clnesp.2021.05.021
Background & aims: Systemic inflammation has been reported as a new predictor for COVID-19 outcomes. Thus, we hypothesized that ICU patients infected by COVID-19 had lower blood vitamin D levels and increased systemic inflammation. Therefore, this is the first Brazilian study to evaluate the vitamin D concentrations and NLR as a systemic inflammation in patients infected by COVID-19 admitted in ICU. Methods: This cross-sectional study selected twenty-six patients from COVID-19 Data Sharing/FAPESP, Brazil. Twenty-five patients were enrolled from a single hospital and those with blood vitamin D and neutrophil and lymphocyte data were included and had all available data analyzed. Patients were divided in two groups: low vitamin D concentration when 20 ng/mL (low Vit D group, n ¼ 8, 5M/3F, 62.7 ± 8.4 years old), and normal vitamin D when > 20 ng/mL (normal Vit D group, n ¼ 17, 9M/8F, 74 ± 8.2 years old). Serum 25-hydroxy-vitamin D, C reactive protein (CRP), and count of neutrophils and lymphocytes concentrations were collected from COVID-19 Data Sharing/FAPESP. Statistical analyses were performed using the Prism version 5.0 and Student T test was applied to verify any difference between the groups. Results: Low vitamin D group had 15.5 ± 3.3 ng/mL of 25OH Vit D concentrations and normal vitamin D group had 35.9 ± 8.8 ng/mL. Although no difference between groups for CRP concentrations (low Vit D: 4.5 ± 3.3 vs. normal Vit D: 4.2 ± 4.0 mg/dL, p ¼ 0.45), we found higher neutrophil count and NLR values in the low Vit D group when compared to normal Vit D group (low Vit D: 6049.8 ± 3719.7 vs. normal Vit D: 3741.8 ± 1704.1 ng/mL, p ¼ 0.02) and (low Vit D: 9.0 ± 8.6 vs. normal Vit D: 4.2 ± 4.0 ng/mL, p ¼ 0.03), respectively. Conclusion: This data sharing-derived cases of COVID-19 in patients admitted at ICU showed that patients infected by COVID-19 had lower serum 25-hydroxy vitamin D and enhanced systemic inflammation when assessed by NLR values.
Authorship GDP, MCMDV, and CP wrote the article and approved the final version of this manuscript.
Funding No funding was received for this work.
Declaration of competing interest None declared.
References
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J Infect Publ Health, doi:10.1016/j.jiph.2020.06.021
Bergman, The link between Vitamin D and Covid-19: distinguishing facts from fiction, J Intern Med, doi:10.1111/joim.13158
Biesalski, Obesity, vitamin D deficiency and old age a serious combination with respect to coronavirus disease-2019 severity and outcome, Curr Opin Clin Nutr Metab Care, doi:10.1097/MCO.0000000000000700
Daoust, Pilon, Marette, Perspective: nutritional strategies targeting the gut microbiome to mitigate COVID-19 outcomes, Adv Nutr, doi:10.1093/advances/nmab031
Evans, Lippman, Shining light on the COVID-19 pandemic: a vitamin D receptor checkpoint in defense of unregulated wound healing, Cell Metabol, doi:10.1016/j.cmet.2020.09.007
Gomes, Fernandes, Vieira, Schincaglia, Mota et al., Low vitamin D at ICU admission is associated with cancer, infections, acute respiratory insufficiency, and liver failure, Nutrition, doi:10.1016/j.nut.2018.10.018
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PloS One, doi:10.1371/journal.pone.0239252
Liao, Zhou, Luo, Xu, Wang et al., Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study, Lancet Haematol, doi:10.1016/S2352-3026(20)30217-9
Liu, Du, Chen, Jin, Peng et al., Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19, J Infect, doi:10.1016/j.jinf.2020.04.002
Pimentel, Vega, Laviano, High neutrophil to lymphocyte ratio as a prognostic marker in COVID-19 patients, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2020.08.004
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area, Jama, doi:10.1001/jama.2020.6775
Richardson, Lovegrove, Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective, Br J Nutr, doi:10.1017/S000711452000330X
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review, JAMA, doi:10.1001/jama.2020.12839
Zhou, Luo, Qin, The association between vitamin D deficiency and community-acquired pneumonia: a meta-analysis of observational studies, Medicine, doi:10.1097/MD.000000000001725
DOI record:
{
"DOI": "10.1016/j.clnesp.2021.05.021",
"ISSN": [
"2405-4577"
],
"URL": "http://dx.doi.org/10.1016/j.clnesp.2021.05.021",
"alternative-id": [
"S2405457721002011"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Low vitamin D levels and increased neutrophil in patients admitted at ICU with COVID-19"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Clinical Nutrition ESPEN"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.clnesp.2021.05.021"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 European Society for Clinical Nutrition and Metabolism. Published by Elsevier Ltd. All rights reserved."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-2979-9819",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pimentel",
"given": "Gustavo D.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Dela Vega",
"given": "Maria C.M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pichard",
"given": "Claude",
"sequence": "additional"
}
],
"container-title": "Clinical Nutrition ESPEN",
"container-title-short": "Clinical Nutrition ESPEN",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.com.au",
"clinicalkey.es",
"clinicalkey.com",
"clinicalnutritionespen.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
5,
31
]
],
"date-time": "2021-05-31T16:30:38Z",
"timestamp": 1622478638000
},
"deposited": {
"date-parts": [
[
2022,
7,
23
]
],
"date-time": "2022-07-23T07:44:18Z",
"timestamp": 1658562258000
},
"funder": [
{
"DOI": "10.13039/501100003593",
"award": [
"312252/2019-6"
],
"doi-asserted-by": "publisher",
"name": "Conselho Nacional de Desenvolvimento Científico e Tecnológico"
}
],
"indexed": {
"date-parts": [
[
2024,
4,
8
]
],
"date-time": "2024-04-08T23:33:09Z",
"timestamp": 1712619189931
},
"is-referenced-by-count": 11,
"issued": {
"date-parts": [
[
2021,
8
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
1
]
],
"date-time": "2021-08-01T00:00:00Z",
"timestamp": 1627776000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2405457721002011?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2405457721002011?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "466-468",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
8
]
]
},
"published-print": {
"date-parts": [
[
2021,
8
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1001/jama.2020.12839",
"article-title": "Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review",
"author": "Wiersinga",
"doi-asserted-by": "crossref",
"first-page": "782",
"issue": "8",
"journal-title": "JAMA",
"key": "10.1016/j.clnesp.2021.05.021_bib1",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6775",
"article-title": "Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area",
"author": "Richardson",
"doi-asserted-by": "crossref",
"first-page": "2052",
"issue": "20",
"journal-title": "Jama",
"key": "10.1016/j.clnesp.2021.05.021_bib2",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1097/MD.0000000000017252",
"article-title": "The association between vitamin D deficiency and community-acquired pneumonia: a meta-analysis of observational studies",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "e17252",
"issue": "38",
"journal-title": "Medicine",
"key": "10.1016/j.clnesp.2021.05.021_bib3",
"volume": "98",
"year": "2019"
},
{
"DOI": "10.1016/j.jiph.2020.06.021",
"article-title": "Role of vitamin D in preventing of COVID-19 infection, progression and severity",
"author": "Ali",
"doi-asserted-by": "crossref",
"first-page": "1373",
"issue": "10",
"journal-title": "J Infect Publ Health",
"key": "10.1016/j.clnesp.2021.05.021_bib4",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1016/j.nut.2018.10.018",
"article-title": "Low vitamin D at ICU admission is associated with cancer, infections, acute respiratory insufficiency, and liver failure",
"author": "Gomes",
"doi-asserted-by": "crossref",
"first-page": "235",
"journal-title": "Nutrition",
"key": "10.1016/j.clnesp.2021.05.021_bib5",
"volume": "60",
"year": "2019"
},
{
"DOI": "10.1111/joim.13158",
"article-title": "The link between Vitamin D and Covid-19: distinguishing facts from fiction",
"author": "Bergman",
"doi-asserted-by": "crossref",
"first-page": "131",
"issue": "1",
"journal-title": "J Intern Med",
"key": "10.1016/j.clnesp.2021.05.021_bib6",
"volume": "289",
"year": "2020"
},
{
"DOI": "10.1016/S2352-3026(20)30217-9",
"article-title": "Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study",
"author": "Liao",
"doi-asserted-by": "crossref",
"first-page": "E671",
"issue": "9",
"journal-title": "Lancet Haematol",
"key": "10.1016/j.clnesp.2021.05.021_bib7",
"volume": "7",
"year": "2020"
},
{
"article-title": "Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19",
"author": "Liu",
"first-page": "e6",
"issue": "1",
"journal-title": "J Infect",
"key": "10.1016/j.clnesp.2021.05.021_bib8",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239252",
"article-title": "SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels",
"author": "Kaufman",
"doi-asserted-by": "crossref",
"first-page": "e0239252",
"issue": "9",
"journal-title": "PloS One",
"key": "10.1016/j.clnesp.2021.05.021_bib9",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.09.007",
"article-title": "Shining light on the COVID-19 pandemic: a vitamin D receptor checkpoint in defense of unregulated wound healing",
"author": "Evans",
"doi-asserted-by": "crossref",
"first-page": "704",
"issue": "5",
"journal-title": "Cell Metabol",
"key": "10.1016/j.clnesp.2021.05.021_bib10",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1097/MCO.0000000000000700",
"article-title": "Obesity, vitamin D deficiency and old age a serious combination with respect to coronavirus disease-2019 severity and outcome",
"author": "Biesalski",
"doi-asserted-by": "crossref",
"first-page": "18",
"issue": "1",
"journal-title": "Curr Opin Clin Nutr Metab Care",
"key": "10.1016/j.clnesp.2021.05.021_bib11",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1017/S000711452000330X",
"article-title": "Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective",
"author": "Richardson",
"doi-asserted-by": "crossref",
"first-page": "678",
"issue": "6",
"journal-title": "Br J Nutr",
"key": "10.1016/j.clnesp.2021.05.021_bib12",
"volume": "125",
"year": "2020"
},
{
"DOI": "10.1093/advances/nmab031",
"article-title": "Perspective: nutritional strategies targeting the gut microbiome to mitigate COVID-19 outcomes",
"author": "Daoust",
"doi-asserted-by": "crossref",
"journal-title": "Adv Nutr",
"key": "10.1016/j.clnesp.2021.05.021_bib13",
"year": "2021"
},
{
"DOI": "10.1016/j.clnesp.2020.08.004",
"article-title": "High neutrophil to lymphocyte ratio as a prognostic marker in COVID-19 patients",
"author": "Pimentel",
"doi-asserted-by": "crossref",
"first-page": "101",
"journal-title": "Clin Nutr ESPEN",
"key": "10.1016/j.clnesp.2021.05.021_fur14",
"volume": "40",
"year": "2020"
}
],
"reference-count": 14,
"references-count": 14,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2405457721002011"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Low vitamin D levels and increased neutrophil in patients admitted at ICU with COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "44"
}
