Musculoskeletal Disorders, Pain Medication, and in-Hospital Mortality among Patients with COVID-19 in South Korea: A Population-Based Cohort Study
et al., International Journal of Environmental Research and Public Health, doi:10.3390/ijerph18136804, Jun 2021
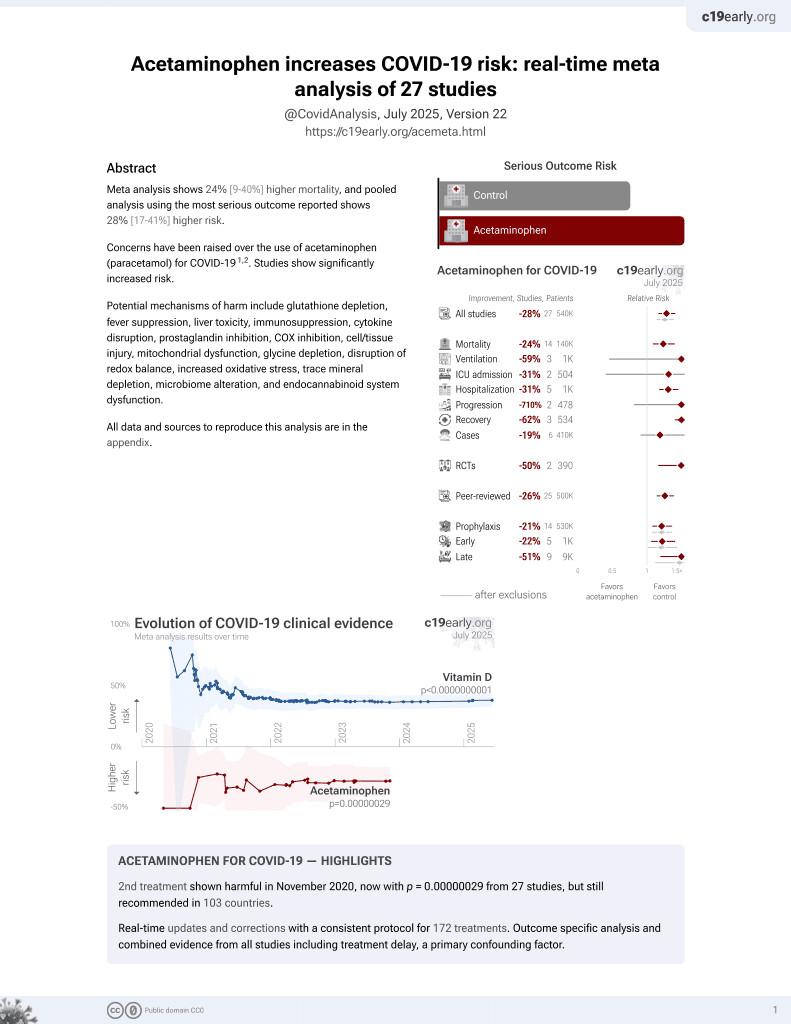
2nd treatment shown to increase risk in
November 2020, now with p = 0.00000029 from 27 studies, but still recommended in 103 countries.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 7,713 COVID-19 patients in Korea, showing no significant difference in mortality with paracetamol use.
Paracetamol is also known as acetaminophen, Tylenol, Panadol, Calpol, Tempra, Calprofen, Doliprane, Efferalgan, Grippostad C, Dolo, Acamol, Fevadol, Crocin, and Perfalgan.
|
risk of death, 1.9% lower, RR 0.98, p = 0.97, treatment 58, control 7,655, adjusted per study, odds ratio converted to relative risk, multivariable, control prevalance approximated with overall prevalence.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Oh et al., 24 Jun 2021, retrospective, South Korea, peer-reviewed, 5 authors, study period 1 January, 2020 - 4 June, 2020.
Contact: uchic@ncc.re.kr (corresponding author), airohtak@hotmail.com, songoficu@outlook.kr, leejoon.com@gmail.com, ytjeon@snubh.org.
Musculoskeletal Disorders, Pain Medication, and in-Hospital Mortality among Patients with COVID-19 in South Korea: A Population-Based Cohort Study
International Journal of Environmental Research and Public Health, doi:10.3390/ijerph18136804
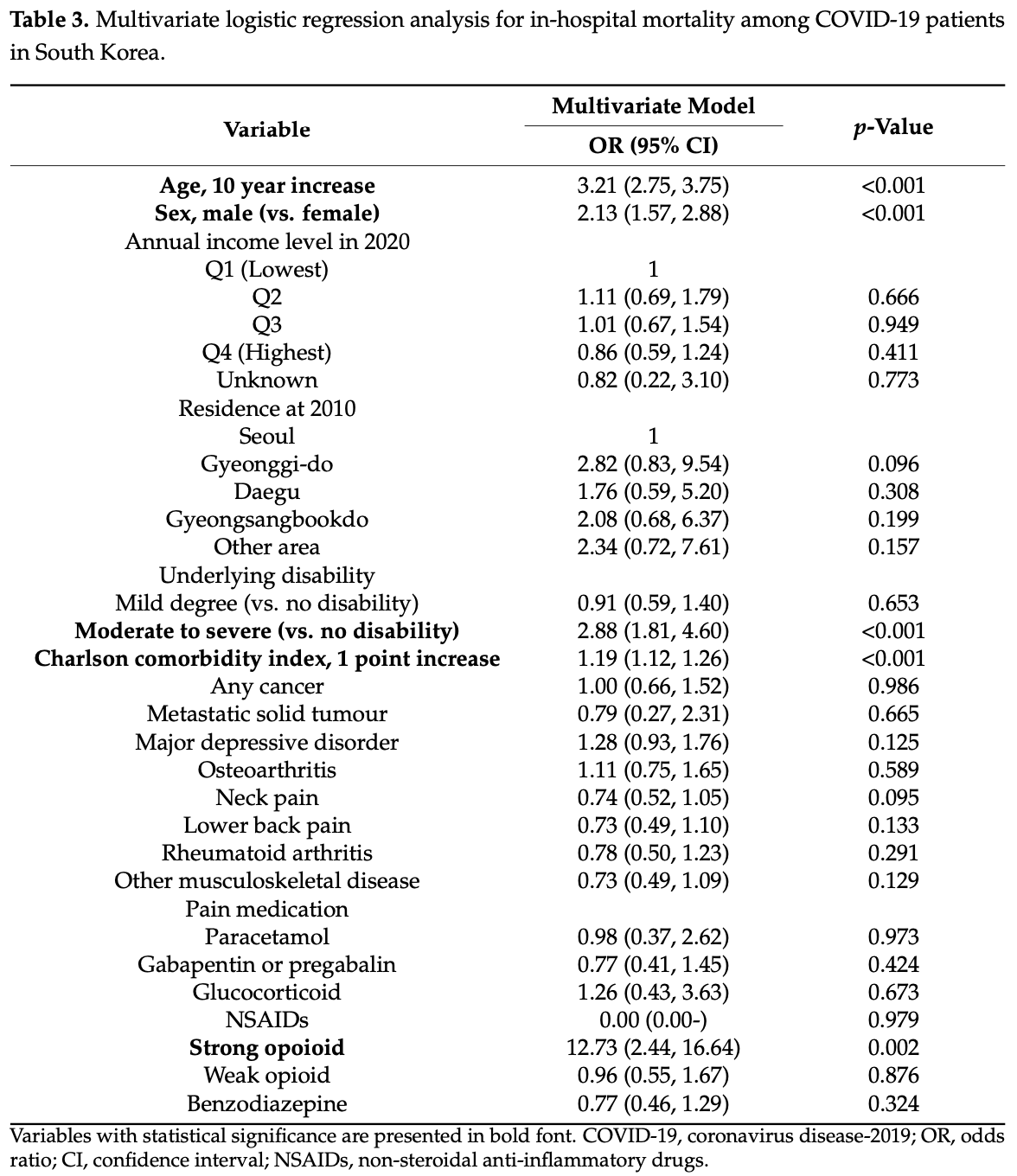
We aimed to investigate whether comorbid musculoskeletal disorders (MSD)s and pain medication use was associated with in-hospital mortality among patients with coronavirus disease 2019 . Adult patients (≥20 years old) with a positive COVID-19 diagnosis until 5 June 2020 were included in this study, based on the National Health Insurance COVID-19 database in South Korea. MSDs included osteoarthritis, neck pain, lower back pain, rheumatoid arthritis, and others, while pain medication included paracetamol, gabapentin, pregabalin, glucocorticoid, nonsteroidal anti-inflammatory drugs (NSAIDs), opioids (strong and weak opioids), and benzodiazepine. Primary endpoint was in-hospital mortality. A total of 7713 patients with COVID-19 were included, and in-hospital mortality was observed in 248 (3.2%) patients. In multivariate logistic regression analysis, no MSDs (p > 0.05) were significantly associated with in-hospital mortality. However, in-hospital mortality was 12.73 times higher in users of strong opioids (odds ratio: 12.73, 95% confidence interval: 2.44-16.64; p = 0.002), while use of paracetamol (p = 0.973), gabapentin or pregabalin (p = 0.424), glucocorticoid (p = 0.673), NSAIDs (p = 0.979), weak opioids (p = 0.876), and benzodiazepine (p = 0.324) was not associated with in-hospital mortality. In South Korea, underlying MSDs were not associated with increased in-hospital mortality among patients with COVID-19. However, use of strong opioids was significantly associated with increased in-hospital mortality among the patients.
Supplementary Materials: The following are available online at https://www.mdpi.com/article/10 .3390/ijerph18136804/s1, Table S1 : ICD-10 codes and Table S2 : The ICD-10 codes used by comorbidity to compute the Charlson comorbidity index. Informed Consent Statement: Informed consent was waived by the IRB, as the analyses were performed retrospectively using anonymized data derived from the South Korean NHIS database.
Conflicts of Interest: The authors declare no conflict of interest.
References
Bedford, Enria, Giesecke, Heymann, Ihekweazu et al., COVID-19: Towards controlling of a pandemic, Lancet, doi:10.1016/S0140-6736(20)30673-5
Briggs, Woolf, Dreinhöfer, Homb, Hoy et al., Reducing the global burden of musculoskeletal conditions, Bull. World Heal. Organ, doi:10.2471/BLT.17.204891
Dagan, Barda, Kepten, Miron, Perchik et al., BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting, N. Engl. J. Med, doi:10.1056/NEJMoa2101765
Diasso, Birke, Nielsen, Main, Højsted et al., The effects of long-term opioid treatment on the immune system in chronic non-cancer pain patients: A systematic review, Eur. J. Pain, doi:10.1002/ejp.1506
Elm, Altman, Egger, Pocock, Gøtzsche et al., The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies, Ann. Intern. Med, doi:10.7326/0003-4819-147-8-200710160-00010
Flint, Janowitz, Connell, Roberts, Denton et al., Tumor-Induced IL-6 Reprograms Host Metabolism to Suppress Anti-tumor Immunity, Cell Metab, doi:10.1016/j.cmet.2016.10.010
Fredi, Cavazzana, Moschetti, Andreoli, Franceschini et al., COVID-19 in patients with rheumatic diseases in northern Italy: A single-centre observational and case-control study, Lancet Rheumatol, doi:10.1016/S2665-9913(20)30169-7
Fung, Babik, COVID-19 in Immunocompromised Hosts: What We Know So Far, Clin. Infect. Dis, doi:10.1093/cid/ciaa863
Generaal, Vogelzangs, Macfarlane, Geenen, Smit et al., Basal inflammation and innate immune response in chronic multisite musculoskeletal pain, Pain, doi:10.1016/j.pain.2014.05.007
Gomes, Tadrous, Mamdani, Paterson, Juurlink, The Burden of Opioid-Related Mortality in the United States, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2018.0217
Greenland, Mansournia, Altman, Sparse data bias: A problem hiding in plain sight, BMJ, doi:10.1136/bmj.i1981
Haberman, Axelrad, Chen, Castillo, Yan et al., Covid-19 in Immune-Mediated Inflammatory Diseases-Case Series from New York, N. Engl. J. Med, doi:10.1056/NEJMc2009567
Haberman, Castillo, Chen, Yan, Ramirez et al., COVID-19 in Patients with Inflammatory Arthritis: A Prospective Study on the Effects of Comorbidities and Disease-Modifying Antirheumatic Drugs on Clinical Outcomes, Arthritis Rheumatol, doi:10.1002/art.41456
Kim, Fine, Li, Kimmel, Ngo et al., Disparities in United States hospitalizations for serious infections in patients with and without opioid use disorder: A nationwide observational study, PLoS Med, doi:10.1371/journal.pmed.1003247
Knoll, Wonodi, Oxford-AstraZeneca COVID-19 vaccine efficacy, Lancet, doi:10.1016/S0140-6736(20)32623-4
Mackinnon, Socías, Bardwell, COVID-19 and overdose prevention: Challenges and opportunities for clinical practice in housing settings, J. Subst. Abus Treat, doi:10.1016/j.jsat.2020.108153
Manuel, Estabrook, The American Society of Transplantation Infectious Diseases Community of Practice. RNA respiratory viral infections in solid organ transplant recipients: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice, Clin. Transplant, doi:10.1111/ctr.13511
Oh, Jeon, Choi, Trends in chronic opioid use and association with five-year survival in South Korea: A populationbased cohort study, Br. J. Anaesth, doi:10.1016/j.bja.2019.08.012
Oh, Song, Trends in long-term glucocorticoid use and risk of 5-year mortality: A historical cohort study in South Korea, Endocrine, doi:10.1007/s12020-020-02382-6
Pereira, Lawlor, Vigano, Dorgan, Bruera, Equianalgesic Dose Ratios for Opioids: A Critical Review and Proposals for Long-Term Dosing, J. Pain Symptom Manag, doi:10.1016/S0885-3924(01)00294-9
Pierce, Bird, Hickman, Millar, National record linkage study of mortality for a large cohort of opioid users ascertained by drug treatment or criminal justice sources in England, 2005-2009, Drug Alcohol Depend, doi:10.1016/j.drugalcdep.2014.09.782
Ray, Chung, Murray, Hall, Stein, Prescription of Long-Acting Opioids and Mortality in Patients with Chronic Noncancer Pain, JAMA, doi:10.1001/jama.2016.7789
Salas, Hotman, Stricker, Confounding by Indication: An Example of Variation in the Use of Epidemiologic Terminology, Am. J. Epidemiol, doi:10.1093/oxfordjournals.aje.a009758
Schimmel, Manini, Opioid Use Disorder and COVID-19: Biological Plausibility for Worsened Outcomes, Subst. Use Misuse, doi:10.1080/10826084.2020.1791184
Schwetz, Calder, Rosenthal, Kattakuzhy, Fauci, Opioids and Infectious Diseases: A Converging Public Health Crisis, J. Infect. Dis, doi:10.1093/infdis/jiz133
Shah, Kuo, Baillargeon, Raji, The impact of long-term opioid use on the risk and severity of COVID-19, J. Opioid Manag, doi:10.5055/jom.2020.0597
Shi, Wang, Shao, Huang, Gan et al., COVID-19 infection: The perspectives on immune responses, Cell Death Differ, doi:10.1038/s41418-020-0530-3
Waghmare, Englund, Boeckh, How I treat respiratory viral infections in the setting of intensive chemotherapy or hematopoietic cell transplantation, Blood, doi:10.1182/blood-2016-01-634873
Wang, Kaelber, Xu, Volkow, COVID-19 risk and outcomes in patients with substance use disorders: Analyses from electronic health records in the United States, Mol. Psychiatry, doi:10.1038/s41380-020-00880-7
Weisberg, Gordon, Barry, Becker, Crystal et al., Long-term Prescription of Opioids and/or Benzodiazepines and Mortality Among HIV-Infected and Uninfected Patients, J. Acquir. Immune Defic. Syndr, doi:10.1097/QAI.0000000000000591
Wilson, Ramage, Fagan, A Primary Care Response to COVID-19 for Patients with an Opioid Use Disorder, J. Rural. Heal, doi:10.1111/jrh.12438
Wolfe, Caplan, Michaud, Treatment for rheumatoid arthritis and the risk of hospitalization for pneumonia: Associations with prednisone, disease-modifying antirheumatic drugs, and anti-tumor necrosis factor therapy, Arthritis Rheum, doi:10.1002/art.21568
DOI record:
{
"DOI": "10.3390/ijerph18136804",
"ISSN": [
"1660-4601"
],
"URL": "http://dx.doi.org/10.3390/ijerph18136804",
"abstract": "<jats:p>We aimed to investigate whether comorbid musculoskeletal disorders (MSD)s and pain medication use was associated with in-hospital mortality among patients with coronavirus disease 2019 (COVID-19). Adult patients (≥20 years old) with a positive COVID-19 diagnosis until 5 June 2020 were included in this study, based on the National Health Insurance COVID-19 database in South Korea. MSDs included osteoarthritis, neck pain, lower back pain, rheumatoid arthritis, and others, while pain medication included paracetamol, gabapentin, pregabalin, glucocorticoid, nonsteroidal anti-inflammatory drugs (NSAIDs), opioids (strong and weak opioids), and benzodiazepine. Primary endpoint was in-hospital mortality. A total of 7713 patients with COVID-19 were included, and in-hospital mortality was observed in 248 (3.2%) patients. In multivariate logistic regression analysis, no MSDs (p > 0.05) were significantly associated with in-hospital mortality. However, in-hospital mortality was 12.73 times higher in users of strong opioids (odds ratio: 12.73, 95% confidence interval: 2.44–16.64; p = 0.002), while use of paracetamol (p = 0.973), gabapentin or pregabalin (p = 0.424), glucocorticoid (p = 0.673), NSAIDs (p = 0.979), weak opioids (p = 0.876), and benzodiazepine (p = 0.324) was not associated with in-hospital mortality. In South Korea, underlying MSDs were not associated with increased in-hospital mortality among patients with COVID-19. However, use of strong opioids was significantly associated with increased in-hospital mortality among the patients.</jats:p>",
"alternative-id": [
"ijerph18136804"
],
"author": [
{
"affiliation": [],
"family": "Oh",
"given": "Tak-Kyu",
"sequence": "first"
},
{
"affiliation": [],
"family": "Song",
"given": "In-Ae",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Joon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Eom",
"given": "Woosik",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jeon",
"given": "Young-Tae",
"sequence": "additional"
}
],
"container-title": "International Journal of Environmental Research and Public Health",
"container-title-short": "IJERPH",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
6,
24
]
],
"date-time": "2021-06-24T15:01:38Z",
"timestamp": 1624546898000
},
"deposited": {
"date-parts": [
[
2021,
6,
25
]
],
"date-time": "2021-06-25T09:09:46Z",
"timestamp": 1624612186000
},
"indexed": {
"date-parts": [
[
2022,
6,
3
]
],
"date-time": "2022-06-03T18:29:13Z",
"timestamp": 1654280953928
},
"is-referenced-by-count": 5,
"issue": "13",
"issued": {
"date-parts": [
[
2021,
6,
24
]
]
},
"journal-issue": {
"issue": "13",
"published-online": {
"date-parts": [
[
2021,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
24
]
],
"date-time": "2021-06-24T00:00:00Z",
"timestamp": 1624492800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1660-4601/18/13/6804/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "6804",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
6,
24
]
]
},
"published-online": {
"date-parts": [
[
2021,
6,
24
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30673-5",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"key": "ref2",
"unstructured": "Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Global Map of Cases and Deaths by Country/Region/Sovereigntyhttps://coronavirus.jhu.edu/map.html"
},
{
"DOI": "10.1056/NEJMoa2101765",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1016/S0140-6736(20)32623-4",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1056/NEJMc2009567",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1038/s41418-020-0530-3",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1111/ctr.13511",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1182/blood-2016-01-634873",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1093/cid/ciaa863",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1016/j.pain.2014.05.007",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1002/art.21568",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1016/j.cmet.2016.10.010",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1002/ejp.1506",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1016/j.bja.2019.08.012",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1007/s12020-020-02382-6",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.5055/jom.2020.0597",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.7326/0003-4819-147-8-200710160-00010",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/S0885-3924(01)00294-9",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1093/oxfordjournals.aje.a009758",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1136/bmj.i1981",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1001/jama.2016.7789",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1001/jamanetworkopen.2018.0217",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1016/j.drugalcdep.2014.09.782",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1093/infdis/jiz133",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1371/journal.pmed.1003247",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1097/QAI.0000000000000591",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1080/10826084.2020.1791184",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1038/s41380-020-00880-7",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/j.jsat.2020.108153",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1111/jrh.12438",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1016/S2665-9913(20)30169-7",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1002/art.41456",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.2471/BLT.17.204891",
"doi-asserted-by": "publisher",
"key": "ref33"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1660-4601/18/13/6804"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Health, Toxicology and Mutagenesis",
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": "Musculoskeletal Disorders, Pain Medication, and in-Hospital Mortality among Patients with COVID-19 in South Korea: A Population-Based Cohort Study",
"type": "journal-article",
"volume": "18"
}