Ursodeoxycholic acid does not affect the clinical outcome of SARS‐CoV‐2 infection: A retrospective study of propensity score‐matched cohorts
et al., Liver International, doi:10.1111/liv.15736, Sep 2023
PSM retrospective 629 hospitalized COVID-19 patients showing no significant difference in survival between 108 patients taking UDCA prior to infection compared to 521 matched controls not taking the drug. The lack of observed benefit in this retrospective inpatient cohort does not preclude potential protective effects of UDCA against infection or illness severe enough to require hospitalization.
|
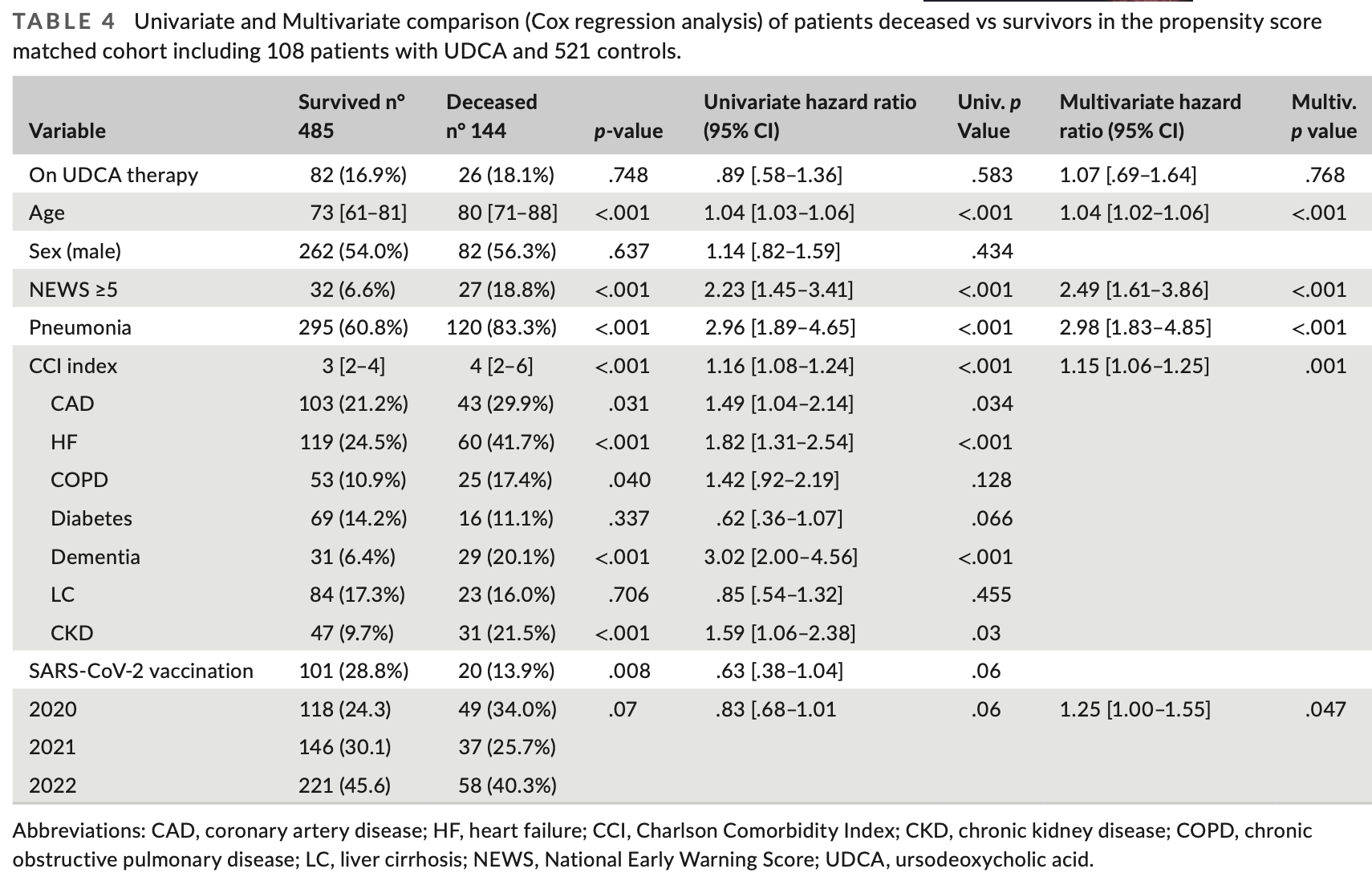
risk of death, 7.0% higher, HR 1.07, p = 0.77, treatment 26 of 108 (24.1%), control 118 of 521 (22.6%), adjusted per study, multivariable, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Marrone et al., 21 Sep 2023, retrospective, Italy, peer-reviewed, 10 authors, study period 1 March, 2020 - 31 December, 2022.
Ursodeoxycholic acid does not affect the clinical outcome of SARS‐CoV‐2 infection: A retrospective study of propensity score‐matched cohorts
Liver International, doi:10.1111/liv.15736
Background: Ursodeoxycholic acid (UDCA) has been recently proposed as a modulator of angiotensin-converting enzyme 2 (ACE2) receptor expression, with potential effects on COVID-19.
Aim and Study Design: We retrospectively evaluated the clinical course and outcome of subjects taking UDCA admitted to the hospital for COVID-19 compared with matched infected subjects. Differences regarding the severity and outcome of the disease between treated and non-treated subjects were assessed. The Kaplan-Meier survival analysis and log-rank test were used to evaluate the effect of UDCA on allcause intra-hospital mortality. Results: Among 6444 subjects with confirmed COVID-19 admitted to the emergency department (ED) from 1 March 2020 to 31 December 2022, 109 subjects were taking UDCA. After matching 629 subjects were included in the study: 521 in the no UDCA group and 108 in the UDCA group. In our matched cohort, 144 subjects (22.9%) died, 118 (22.6%) in the no-UDCA group and 26 (24.1%) in the UDCA group. The Kaplan-Meier analysis showed no significant difference in survival between groups. In univariate regression analysis, the presence of pneumonia, National Early Warning Score (NEWS) score, and Charlson Comorbidity Index (CCI) were significant independent predictors of death. At multivariate Cox regression analysis, age, NEWS, pneumonia and CCI index were confirmed significant independent predictors of death. UDCA treatment was not a predictor of survival both in univariate and multivariate regressions. Conclusions: UDCA treatment does not appear to have significant effects on the outcome of COVID-19. Specially designed prospective studies are needed to evaluate efficacy in preventing infection and severe disease.
K E Y W O R D S COVID-19, SARS-CoV-2, UDCA
Key points Treatment with ursodeoxycholic acid has no effect on the outcome of SARS-CoV-2 infection in hospitalized subjects. Age, presence of pneumonia, comorbidities and severity at onset are confirmed as predictors of unfavourable outcomes.
AUTH O R CO NTR I B UTI O N S Marcello Covino and Giuseppe Marrone were responsible for the conception and writing of the paper; Marcello Covino, Annamaria Amodeo and Giuseppe Marrone performed data collection, Marcello Covino and Giuseppe Marrone performed data analysis, Maurizio Pompili, Rita Murri, Angela Novelli, Andrea Piccioni and Giuseppe Merra reviewed the manuscript; Francesco Franceschi, Antonio Gasbarrini, Marcello Covino, Giuseppe Marrone performed final editing of the manuscript. All the authors approved the final version of the manuscript.
CO N FLI C T O F I NTER E S T S TATEM ENT The authors do not have any disclosures to report.
S U PP O RTI N G I N FO R M ATI O N Additional supporting information can be found online in the Supporting Information section at the end of this article.
How to cite this article:
References
Alabsi, Dhole, Hozayen, Chapman, Angiotensin-converting enzyme 2 expression and severity of SARS-CoV-2 infection, Microorganisms, doi:/10.3390/MICROORGANISMS11030612
Alenezi, Almeshari, Mahida, Bangash, Thickett et al., Incidence and risk factors of acute kidney injury in COVID-19 patients with and without acute respiratory distress syndrome (ARDS) during the first wave of COVID-19: a systematic review and meta-analysis, Ren Fail, doi:/10.1080/0886022X.2021.2011747
Beigel, Tomashek, Dodd, Remdesivir for the treatment of Covid-19 -final report, N Engl J Med, doi:/10.1056/NEJMOA2007764
Biswas, Rahaman, Biswas, Haque, Association of sex, age, and comorbidities with mortality in COVID-19 patients: a systematic review and meta-analysis, Intervirology, doi:/10.1159/000512592
Brevini, Maes, Webb, FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2, Nature, doi:/10.1038/S41586-022-05594-0
Cai, Yang, Liu, Experimental treatment with favipiravir for COVID-19: an open-label control study, Engineering, doi:/10.1016/J.ENG.2020.03.007
Canales, Mayoral, Hernández-Huerta, Interaction of spike protein and lipid membrane of SARS-CoV-2 with Ursodeoxycholic acid, an in-silico analysis, Sci Rep, doi:/10.1038/S41598-021-01705-5
Carino, Moraca, Fiorillo, Hijacking SARS-CoV-2/ACE2 receptor interaction by natural and semi-synthetic steroidal agents acting on functional pockets on the receptor binding domain, Front Chem, doi:/10.3389/FCHEM.2020.572885/BIBTEX
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis, doi:/10.1016/0021-9681(87)90171-8
Charlton, Levitsky, Aqel, International liver transplant society consensus statement on immunosuppression in liver transplant recipients, Transplantation, doi:/10.1097/TP.0000000000002147
Chatterjee, Nalla, Sharma, Association of COVID-19 with comorbidities: an update, ACS Pharmacol Transl Sci, doi:/10.1021/ACSPTSCI.2C00181
Cheung, Mok, Mao, COVID-19 vaccine immunogenicity among chronic liver disease patients and liver transplant recipients: a meta-analysis, Clin Mol Hepatol, doi:/10.3350/CMH.2022.0087
Colapietro, Angelotti, Masetti, Ursodeoxycholic acid does not improve COVID-19 outcome in hospitalized patients, Viruses, doi:/10.3390/v15081738
Covino, Petruzziello, Onder, A 12-year retrospective analysis of differences between elderly and oldest old patients referred to the emergency department of a large tertiary hospital, Maturitas, doi:/10.1016/J.MATURITAS.2018.11.011
Covino, Russo, Salini, Frailty assessment in the emergency department for risk stratification of COVID-19 patients aged ≥80 years, J Am Med Dir Assoc, doi:/10.1016/J.JAMDA.2021.07.005
Cromer, Steain, Reynaldi, Predicting vaccine effectiveness against severe COVID-19 over time and against variants: a meta-analysis, Nat Commun, doi:/10.1038/S41467-023-37176-7
De Almeida, Borges Freire, De Andrade, The landscape of neutralizing monoclonal antibodies (nAbs) for treatment and prevention of COVID-19, J Pharm Innov, doi:/10.1007/S12247-023-09713-W
De Vries, Beuers, Management of cholestatic disease in 2017, Liver Int, doi:/10.1111/LIV.13306
Giovinazzo, Vaccaro, Pascale, SARS-CoV-2 infection in adult liver transplantation recipients: a systematic review of risk factors for mortality and immunosuppression role, Eur Rev Med Pharmacol Sci, doi:/10.26355/eurrev_202302_31413
Gottlieb, Vaca, Paredes, Early Remdesivir to prevent progression to severe Covid-19 in outpatients, N Engl J Med, doi:/10.1056/NEJMOA2116846
Grieco, Menga, Cesarano, Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial, JAMA, doi:/10.1001/JAMA.2021.4682
Grupper, Rabinowich, Schwartz, Reduced humoral response to mRNA SARS-CoV-2 BNT162b2 vaccine in kidney transplant recipients without prior exposure to the virus, Am J Transplant, doi:/10.1111/AJT.16615
Hirschfield, Beuers, Corpechot, EASL clinical practice guidelines: the diagnosis and management of patients with primary biliary cholangitis, J Hepatol, doi:/10.1016/J.JHEP.2017.03.022
Hoffmann, Kleine-Weber, Schroeder, SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell, doi:/10.1016/J.CELL.2020.02.052
Horby, Mafham, Bell, Lopinavir-ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial, Lancet, doi:/10.1016/S0140-6736(20)32013-4
Işık, Karaman, Micili, Beneficial effects of ursodeoxycholic acid via inhibition of airway remodelling, apoptosis of airway epithelial cells, and Th2 immune response in murine model of chronic asthma, Allergol Immunopathol, doi:/10.1016/J.ALLER.2016.12.003
Jackson, Anderson, Rouphael, An mRNA vaccine against SARS-CoV-2 -preliminary report, N Engl J Med, doi:/10.1056/NEJMOA2022483
John, Bastaich, Webb, Ursodeoxycholic acid is associated with a reduction in SARS-CoV-2 infection and reduced severity of COVID-19 in patients with cirrhosis, J Intern Med, doi:/10.1111/JOIM.13630
Li, Li, Chang, Liu, High-flow nasal cannula reduces intubation rate in patients with COVID-19 with acute respiratory failure: a meta-analysis and systematic review, BMJ Open, doi:/10.1136/BMJOPEN-2022-067879
Li, Noreen, Zhang, A critical analysis of SARS-CoV-2 (COVID-19) complexities, emerging variants, and therapeutic interventions and vaccination strategies, Biomed Pharmacother, doi:/10.1016/J.BIOPHA.2021.112550
Marjot, Moon, Cook, Outcomes following SARS-CoV-2 infection in patients with chronic liver disease: an international registry study, J Hepatol, doi:/10.1016/J.JHEP.2020.09.024
Mcconnell, Harte, Walsh, Comparative effectiveness of neutralising monoclonal antibodies in high risk COVID-19 patients: a Bayesian network meta-analysis, Sci Rep, doi:/10.1038/S41598-022-22431-6
Mroz, Harvey, Ursodeoxycholic acid inhibits ENaC and Na/K pump activity to restore airway surface liquid height in cystic fibrosis bronchial epithelial cells, Steroids, doi:/10.1016/J.STEROIDS.2019.108461
Niu, Li, Xu, Sun, Gan et al., Ursodeoxycholic acid protects against lung injury induced by fat embolism syndrome, J Cell Mol Med, doi:/10.1111/JCMM.15985
Ojetti, Saviano, Covino, COVID-19 and intestinal inflammation: role of fecal calprotectin, Dig Liver Dis, doi:/10.1016/J.DLD.2020.09.015
Polack, Thomas, Kitchin, Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine, N Engl J Med, doi:/10.1056/NEJMOA2034577
Prayitno, Bhat, Repurposing UDCA, an FXR inhibitor, to prevent SARS-Cov-2 infection, Gastroenterology, doi:/10.1053/J.GASTRO.2023.01.014
Ridjab, Ivan, Budiman, Juzar, Outcome in early vs late intubation among COVID-19 patients with acute respiratory distress syndrome: an updated systematic review and meta-analysis, Sci Rep, doi:/10.1038/S41598-022-26234-7
Rubin, Chan-Tack, Farley, Sherwat, FDA approval of remdesivir -a step in the right direction, N Engl J Med, doi:/10.1056/NEJMP2032369
Smith, Prytherch, Meredith, Schmidt, Featherstone, The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death, Resuscitation, doi:/10.1016/J.RESUSCITATION.2012.12.016
Sánchez-Zapardiel, Alós, Nozal, Humoral and cellular immune responses to Pfizer-BioNTech BNT162b2 SARS-CoV-2 vaccine in adolescents with liver transplantation: single center experience, Front Immunol, doi:/10.3389/FIMMU.2022.1049188
The, Group, Dexamethasone in hospitalized patients with Covid-19, N Engl J Med, doi:/10.1056/NEJMOA2021436/SUPPL_FILE/NEJMOA2021436_DATA-SHARING.PDF
Thuy, Bao, Moon, Ursodeoxycholic acid ameliorates cell migration retarded by the SARS-CoV-2 spike protein in BEAS-2B human bronchial epithelial cells, Biomed Pharmacother, doi:/10.1016/J.BIOPHA.2022.113021
Vardavas, Mathioudakis, Nikitara, Prognostic factors for mortality, intensive care unit and hospital admission due to SARS-CoV-2: a systematic review and meta-analysis of cohort studies in Europe, Eur Respir Rev, doi:/10.1183/16000617.0098-2022
Wang, Qiu, Liu, Wang, Zhao, The liver injury and gastrointestinal symptoms in patients with coronavirus disease 19: a systematic review and meta-analysis, Clin Res Hepatol Gastroenterol, doi:/10.1016/J.CLINRE.2020.04.012
Webb, Marjot, Cook, Outcomes following SARS-CoV-2 infection in liver transplant recipients: an international registry study, Lancet Gastroenterol Hepatol, doi:/10.1016/S2468-1253(20)30271-5
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:/10.1038/S41586-020-2521-4
Xie, Wang, Liao, Marley, Wu et al., Epidemiologic, clinical, and laboratory findings of the COVID-19 in the current pandemic: systematic review and meta-analysis, BMC Infect Dis, doi:/10.1186/S12879-020-05371-2
Zhou, Yang, Wang, A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature, doi:/10.1038/s41586-020-2012-7
DOI record:
{
"DOI": "10.1111/liv.15736",
"ISSN": [
"1478-3223",
"1478-3231"
],
"URL": "http://dx.doi.org/10.1111/liv.15736",
"abstract": "<jats:title>Abstract</jats:title><jats:sec><jats:title>Background</jats:title><jats:p>Ursodeoxycholic acid (UDCA) has been recently proposed as a modulator of angiotensin‐converting enzyme 2 (ACE2) receptor expression, with potential effects on COVID‐19.</jats:p></jats:sec><jats:sec><jats:title>Aim and Study Design</jats:title><jats:p>We retrospectively evaluated the clinical course and outcome of subjects taking UDCA admitted to the hospital for COVID‐19 compared with matched infected subjects. Differences regarding the severity and outcome of the disease between treated and non‐treated subjects were assessed. The Kaplan–Meier survival analysis and log‐rank test were used to evaluate the effect of UDCA on all‐cause intra‐hospital mortality.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Among 6444 subjects with confirmed COVID‐19 admitted to the emergency department (ED) from 1 March 2020 to 31 December 2022, 109 subjects were taking UDCA. After matching 629 subjects were included in the study: 521 in the no UDCA group and 108 in the UDCA group. In our matched cohort, 144 subjects (22.9%) died, 118 (22.6%) in the no‐UDCA group and 26 (24.1%) in the UDCA group. The Kaplan–Meier analysis showed no significant difference in survival between groups. In univariate regression analysis, the presence of pneumonia, National Early Warning Score (NEWS) score, and Charlson Comorbidity Index (CCI) were significant independent predictors of death. At multivariate Cox regression analysis, age, NEWS, pneumonia and CCI index were confirmed significant independent predictors of death. UDCA treatment was not a predictor of survival both in univariate and multivariate regressions.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>UDCA treatment does not appear to have significant effects on the outcome of COVID‐19. Specially designed prospective studies are needed to evaluate efficacy in preventing infection and severe disease.</jats:p></jats:sec>",
"alternative-id": [
"10.1111/liv.15736"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2023-05-07"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2023-09-04"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2023-09-21"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-9475-3948",
"affiliation": [
{
"name": "Medical and Surgical Abdominal and Endocrine Metabolic Sciences AND Emergency, Anesthesiology and Resuscitation Departements Fondazione Policlinico Universitario A. Gemelli‐IRCCS Rome Italy"
},
{
"name": "Università Cattolica del Sacro Cuore Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Marrone",
"given": "Giuseppe",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-9916-9372",
"affiliation": [
{
"name": "Medical and Surgical Abdominal and Endocrine Metabolic Sciences AND Emergency, Anesthesiology and Resuscitation Departements Fondazione Policlinico Universitario A. Gemelli‐IRCCS Rome Italy"
},
{
"name": "Università Cattolica del Sacro Cuore Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Covino",
"given": "Marcello",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4753-3528",
"affiliation": [
{
"name": "Department of Biomedicine and Prevention Università degli Studi di Roma Tor Vergata Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Merra",
"given": "Giuseppe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5703-8737",
"affiliation": [
{
"name": "Medical and Surgical Abdominal and Endocrine Metabolic Sciences AND Emergency, Anesthesiology and Resuscitation Departements Fondazione Policlinico Universitario A. Gemelli‐IRCCS Rome Italy"
},
{
"name": "Università Cattolica del Sacro Cuore Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Piccioni",
"given": "Andrea",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0009-0007-5539-0789",
"affiliation": [
{
"name": "Medical and Surgical Abdominal and Endocrine Metabolic Sciences AND Emergency, Anesthesiology and Resuscitation Departements Fondazione Policlinico Universitario A. Gemelli‐IRCCS Rome Italy"
},
{
"name": "Università Cattolica del Sacro Cuore Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Amodeo",
"given": "Annamaria",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0009-0000-9202-6512",
"affiliation": [
{
"name": "Medical and Surgical Abdominal and Endocrine Metabolic Sciences AND Emergency, Anesthesiology and Resuscitation Departements Fondazione Policlinico Universitario A. Gemelli‐IRCCS Rome Italy"
},
{
"name": "Università Cattolica del Sacro Cuore Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Novelli",
"given": "Angela",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9468-5458",
"affiliation": [
{
"name": "Medical and Surgical Abdominal and Endocrine Metabolic Sciences AND Emergency, Anesthesiology and Resuscitation Departements Fondazione Policlinico Universitario A. Gemelli‐IRCCS Rome Italy"
},
{
"name": "Università Cattolica del Sacro Cuore Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Murri",
"given": "Rita",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6699-7980",
"affiliation": [
{
"name": "Medical and Surgical Abdominal and Endocrine Metabolic Sciences AND Emergency, Anesthesiology and Resuscitation Departements Fondazione Policlinico Universitario A. Gemelli‐IRCCS Rome Italy"
},
{
"name": "Università Cattolica del Sacro Cuore Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Pompili",
"given": "Maurizio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4863-6924",
"affiliation": [
{
"name": "Medical and Surgical Abdominal and Endocrine Metabolic Sciences AND Emergency, Anesthesiology and Resuscitation Departements Fondazione Policlinico Universitario A. Gemelli‐IRCCS Rome Italy"
},
{
"name": "Università Cattolica del Sacro Cuore Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Gasbarrini",
"given": "Antonio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6266-445X",
"affiliation": [
{
"name": "Medical and Surgical Abdominal and Endocrine Metabolic Sciences AND Emergency, Anesthesiology and Resuscitation Departements Fondazione Policlinico Universitario A. Gemelli‐IRCCS Rome Italy"
},
{
"name": "Università Cattolica del Sacro Cuore Rome Italy"
}
],
"authenticated-orcid": false,
"family": "Franceschi",
"given": "Francesco",
"sequence": "additional"
}
],
"container-title": "Liver International",
"container-title-short": "Liver International",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2023,
9,
22
]
],
"date-time": "2023-09-22T06:55:20Z",
"timestamp": 1695365720000
},
"deposited": {
"date-parts": [
[
2023,
9,
22
]
],
"date-time": "2023-09-22T06:55:26Z",
"timestamp": 1695365726000
},
"indexed": {
"date-parts": [
[
2023,
9,
23
]
],
"date-time": "2023-09-23T16:18:00Z",
"timestamp": 1695485880166
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
9,
21
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
9,
21
]
],
"date-time": "2023-09-21T00:00:00Z",
"timestamp": 1695254400000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1111/liv.15736",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"prefix": "10.1111",
"published": {
"date-parts": [
[
2023,
9,
21
]
]
},
"published-online": {
"date-parts": [
[
2023,
9,
21
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1016/J.BIOPHA.2021.112550",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_2_1"
},
{
"DOI": "10.1186/S12879-020-05371-2",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_3_1"
},
{
"DOI": "10.1016/J.CLINRE.2020.04.012",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_4_1"
},
{
"DOI": "10.1080/0886022X.2021.2011747",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_5_1"
},
{
"DOI": "10.1016/J.DLD.2020.09.015",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_6_1"
},
{
"DOI": "10.1038/S41467-023-37176-7",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_7_1"
},
{
"DOI": "10.1159/000512592",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_8_1"
},
{
"DOI": "10.1038/S41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_9_1"
},
{
"DOI": "10.1016/J.JAMDA.2021.07.005",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_10_1"
},
{
"DOI": "10.1183/16000617.0098-2022",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_11_1"
},
{
"DOI": "10.1053/J.GASTRO.2023.01.014",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_12_1"
},
{
"DOI": "10.3390/MICROORGANISMS11030612",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_13_1"
},
{
"DOI": "10.1038/S41586-022-05594-0",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_14_1"
},
{
"DOI": "10.1016/J.JHEP.2017.03.022",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_15_1"
},
{
"DOI": "10.1111/LIV.13306",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_16_1"
},
{
"DOI": "10.1016/J.STEROIDS.2019.108461",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_17_1"
},
{
"DOI": "10.1111/JCMM.15985",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_18_1"
},
{
"DOI": "10.1016/J.ALLER.2016.12.003",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_19_1"
},
{
"DOI": "10.1016/J.RESUSCITATION.2012.12.016",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_20_1"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_21_1"
},
{
"DOI": "10.1016/J.CELL.2020.02.052",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_22_1"
},
{
"DOI": "10.1038/s41586-020-2012-7",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_23_1"
},
{
"DOI": "10.1016/S0140-6736(20)32013-4",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_24_1"
},
{
"DOI": "10.1016/J.ENG.2020.03.007",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_25_1"
},
{
"DOI": "10.1056/NEJMP2032369",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_26_1"
},
{
"DOI": "10.1056/NEJMOA2022483",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_27_1"
},
{
"DOI": "10.1056/NEJMOA2034577",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_28_1"
},
{
"DOI": "10.1007/S12247-023-09713-W",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_29_1"
},
{
"DOI": "10.1016/J.JHEP.2020.09.024",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_30_1"
},
{
"DOI": "10.1016/S2468-1253(20)30271-5",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_31_1"
},
{
"DOI": "10.1038/S41598-021-01705-5",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_32_1"
},
{
"DOI": "10.3389/FCHEM.2020.572885/BIBTEX",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_33_1"
},
{
"DOI": "10.1016/J.BIOPHA.2022.113021",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_34_1"
},
{
"DOI": "10.3390/v15081738",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_35_1"
},
{
"DOI": "10.1021/ACSPTSCI.2C00181",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_36_1"
},
{
"DOI": "10.1016/J.MATURITAS.2018.11.011",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_37_1"
},
{
"DOI": "10.1056/NEJMOA2021436/SUPPL_FILE/NEJMOA2021436_DATA-SHARING.PDF",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_38_1"
},
{
"DOI": "10.1038/S41598-022-22431-6",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_39_1"
},
{
"DOI": "10.1056/NEJMOA2007764",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_40_1"
},
{
"DOI": "10.1056/NEJMOA2116846",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_41_1"
},
{
"DOI": "10.26355/eurrev_202302_31413",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_42_1"
},
{
"DOI": "10.1097/TP.0000000000002147",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_43_1"
},
{
"DOI": "10.3350/CMH.2022.0087",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_44_1"
},
{
"DOI": "10.1111/AJT.16615",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_45_1"
},
{
"DOI": "10.3389/FIMMU.2022.1049188",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_46_1"
},
{
"DOI": "10.1038/S41598-022-26234-7",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_47_1"
},
{
"DOI": "10.1136/BMJOPEN-2022-067879",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_48_1"
},
{
"DOI": "10.1001/JAMA.2021.4682",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_49_1"
},
{
"DOI": "10.1111/JOIM.13630",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_50_1"
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1111/liv.15736"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Hepatology"
],
"subtitle": [],
"title": "Ursodeoxycholic acid does not affect the clinical outcome of <scp>SARS‐CoV‐2</scp> infection: A retrospective study of propensity score‐matched cohorts",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy"
}