Factors associated with COVID-19 fatality among patients admitted in Mashonaland West Province, Zimbabwe 2020-2022: a secondary data analysis
et al., Pan African Medical Journal, doi:10.11604/pamj.2023.44.142.37858, Mar 2023
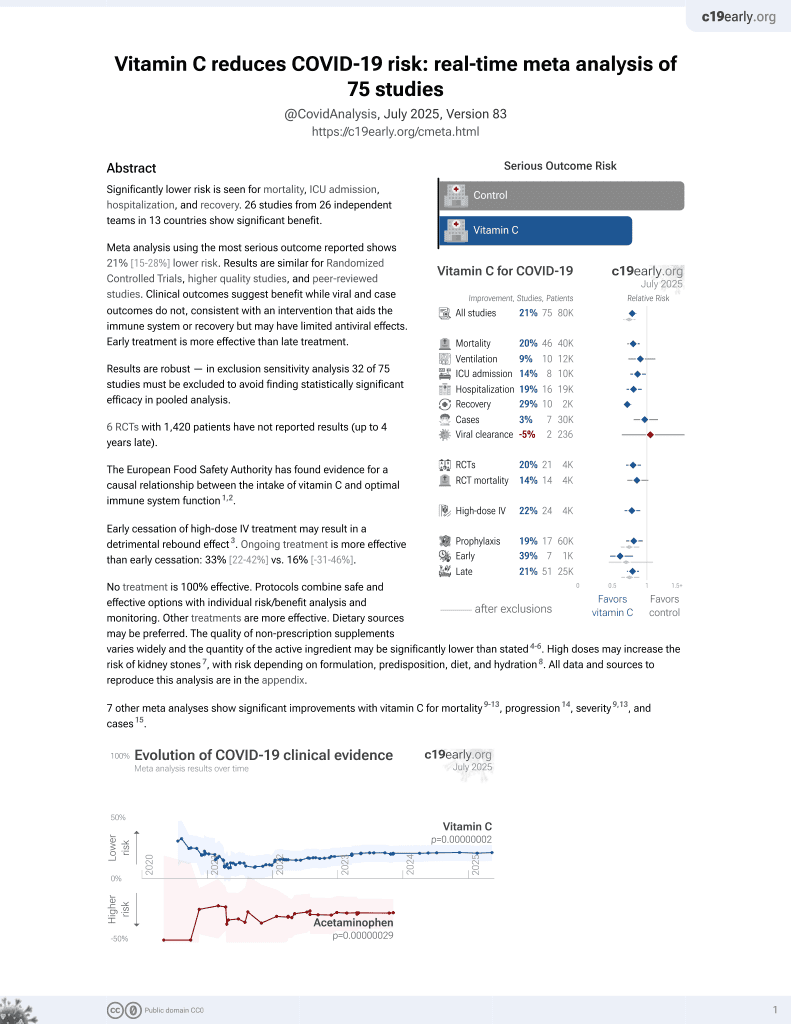
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000068 from 74 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 672 COVID-19 patients in Zimbabwe, showing lower mortality with vitamin C and azithromycin treatment, and higher mortality with dexamethasone treatment.
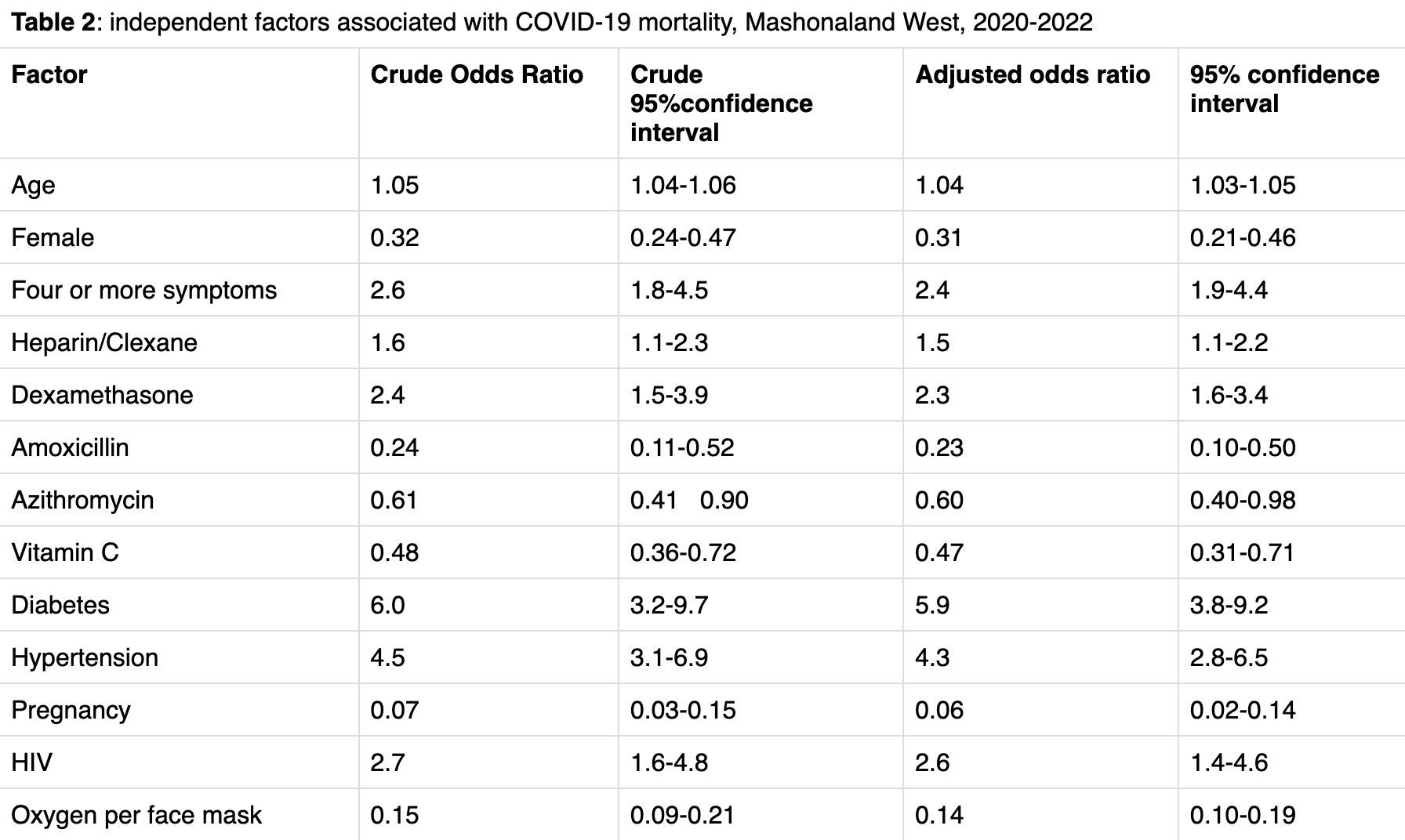
Results are pending author clarification/correction due to internal inconsistencies. The paper contains sample size discrepancies (672 vs. 673 vs. 605 patients), conflicting death counts (157 vs. 141), and case fatality rates that vary between 19%, 23%, and 26% across different sections without explanation. The adjusted odds ratios reported in the abstract differ from those in Table 2 for multiple variables (e.g., hypertension aOR 4.5 vs. 4.3; dexamethasone aOR 2.4 vs. 2.3; heparin aOR 1.6 vs. 1.5), suggesting either multiple unreported model specifications or transcription errors. Pregnancy appears strongly protective (aOR 0.06) in contradiction with expectations and other research. Authors also acknowledge high missing data rates.
This study is excluded in meta-analysis:
multiple potential data reliability issues.
Study covers vitamin C and dexamethasone.
|
risk of death, 53.0% lower, OR 0.47, p < 0.001, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Madamombe et al., 21 Mar 2023, retrospective, Zimbabwe, peer-reviewed, 9 authors, study period April 2020 - April 2022, dosage not specified.
Factors associated with COVID-19 fatality among patients admitted in Mashonaland West Province, Zimbabwe 2020-2022: a secondary data analysis
Pan African Medical Journal, doi:10.11604/pamj.2023.44.142.37858
Introduction: approximately 15% of COVID-19 patients develop symptoms necessitating admission. From 2020 to 2022, Mashonaland West Province had an institutional case fatality rate of 23% against a national rate of 7%. Therefore, we evaluated the COVID-19 admissions in the province to determine the factors associated with COVID-19 mortality. Methods: we conducted an analytical cross-sectional study based on secondary data from isolation centers across the province using all 672 death audit forms and patient records. We obtained data on patient demographics, signs and symptoms, clinical management and oxygen therapy administered, among other things. Data were entered into an electronic form and imported into Epi-info 7 for analysis bivariate and multivariate conducted. Results: we found that being an older man, aOR 1.04 (1.03-1.05), who had diabetes aOR 6.0 (95% CI: 3.8-9.2) and hypertension aOR 4.5 (95% CI: 2.8-6.5) were independent risk factors. Patients put on dexamethasone aOR 2.4 (95% CI: 1.6-3.4) and heparin/clexane aOR 1.6 (95% CI: 1.1-2.2) had a higher mortality risk. However, vitamin C aOR 0.48 (95% CI: 0.31-0.71) and oxygen therapy aOR 0.14 (95% CI: 0.10-0.19) and being pregnant aOR 0.06 (95% CI: 0.02-0.14) were protective. Conclusion: mortality risk increased in older male patients with comorbidities and with those on dexamethasone and heparin therapy. Oxygen therapy and vitamin C were protective. There is a need to conduct further study of the source of these variations in risk across patients to establish the true impact of differences in individuals' mortality.
Competing interests The authors declare no competing interests.
Authors' contributions Kudzai Madamombe, Gerald Shambira, Tapiwa Dhliwayo, Gift Masoja, Notion Tafara Gombe, Addmore Chadambuka, Tsitsi Patience Juru and Mufuta Tshimanga: conception, design, acquisition, data collection, analysis and interpretation of data. Kudzai Madamombe and Gerald Shambira wrote the first draft of the manuscript. Addmore Chadambuka, Notion Tafara Gombe, Tsitsi Patience Juru and Mufuta Tshimanga critically revised the draft for important intellectual content. All authors have read and approved the final version of this manuscript.
References
Abate, Ali, Mantfardo, Basu, Rate of Intensive Care Unit admission and outcomes among patients with coronavirus: A systematic review and Meta-analysis, PLoS One
Adams, Mackenzie, Amegah, Ezeh, Gadanya et al., The Conundrum of Low COVID-19 Mortality Burden in sub-Saharan Africa: Myth or Reality? GHSP
Ashish, Gurung, Kinney, Sunny, Moinuddin et al., Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study, Lancet Glob Health
Bamgboye, Omiye, Afolaranmi, Davids, Tannor et al., COVID-19 Pandemic: Is Africa Different, J Natl Med Assoc
Barda, Riesel, Akriv, Levy, Finkel et al., Developing a COVID-19 mortality risk prediction model when individual-level data are not available, Nat Commun
Bertsimas, Lukin, Mingardi, Nohadani, Orfanoudaki et al., COVID-19 mortality risk assessment: An international multi-center study, PLoS One
Bi, Wu, Mei, Ye, Zou et al., Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study, Lancet Infect Dis
Books, Chapter 9 Rubin's Rules
Ciceri, Ruggeri, Lembo, Puglisi, Landoni et al., Decreased in-hospital mortality in patients with COVID-19 pneumonia, Pathog Glob Health
Dalal, Triulzi, James, Nguimbis, Dri et al., COVID-19 mortality in women and men in sub-Saharan Africa: a cross-sectional study, BMJ Glob Health
Fahme, Walsh, Rouzier, Chebrolu, Jaka et al., Practical recommendations for the prevention and management of COVID-19 in low-income and middle-income settings: adapting clinical experience from the field, Fam Med Community Health
Fauci, Lane, Redfield, COVID-19 -Navigating the Uncharted, N Engl J Med
Kraef, Juma, Kallestrup, Mucumbitsi, Ramaiya et al., The COVID-19 Pandemic and Non-communicable Diseases-A Wake-up Call for Primary Health Care System Strengthening in sub-Saharan Africa, J Prim Care Community Health
Mehta, Goel, Kabarriti, Cole, Goldfinger et al., Case Fatality Rate of Cancer Patients with COVID-19 in a New York Hospital System, Cancer Discov
Meizlish, Goshua, Liu, Fine, Amin, Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: A propensity scorematched analysis, Am J Hematol
Mikami, Miyashita, Yamada, Harrington, Steinberg et al., Risk Factors for Mortality in Patients with COVID-19 in New York City, J Gen Intern Med
Mohammed, Muhammad, Mohammed, Mustapha, Sha'aban et al., Risk Factors Associated with Mortality Among Patients with Novel Coronavirus Disease (COVID-19) in Africa, J Racial Ethn Health Disparities
Najera, Ortega-Avila, Health and Institutional Risk Factors of COVID-19 Mortality in Mexico, 2020, Am J Prev Med
Nakkazi, Oxygen supplies and COVID-19 mortality in Africa, Lancet Respir Med
Okeahalam, Williams, Otwombe, Factors associated with COVID-19 infections and mortality in Africa: a cross-sectional study using publicly available data, BMJ Open
Oksanen, Kaakinen, Latikka, Savolainen, Savela et al., Regulation and Trust: 3-Month Follow-up Study on COVID-19 Mortality in 25 European Countries, JMIR Public Health Surveill
Rath, Petersen-Uribe, Avdiu, Witzel, Jaeger et al., Impaired cardiac function is associated with mortality in patients with acute COVID-19 infection, Clin Res Cardiol
Rothan, Byrareddy, The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak, J Autoimmun
Sussman, Time for Bed(s): Hospital Capacity and Mortality from COVID-19
Westgren, Pettersson, Hagberg, Acharya, Severe maternal morbidity and mortality associated with COVID-19: The risk should not be downplayed, Acta Obstet Gynecol Scand
DOI record:
{
"DOI": "10.11604/pamj.2023.44.142.37858",
"ISSN": [
"1937-8688"
],
"URL": "http://dx.doi.org/10.11604/pamj.2023.44.142.37858",
"alternative-id": [
"37858"
],
"author": [
{
"affiliation": [],
"family": "Madamombe",
"given": "Kudzai",
"sequence": "first"
},
{
"affiliation": [],
"family": "Shambira",
"given": "Gerald",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Masoja",
"given": "Gift",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dhliwayo",
"given": "Tapiwa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Juru",
"given": "Tsitsi Patience",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gombe",
"given": "Notion Tafara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chadambuka",
"given": "Addmore",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Karakadzai",
"given": "Mujinga",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tshimanga",
"given": "Mufuta",
"sequence": "additional"
}
],
"container-title": "Pan African Medical Journal",
"container-title-short": "Pan Afr Med J",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"panafrican-med-journal.com"
]
},
"created": {
"date-parts": [
[
2023,
3,
21
]
],
"date-time": "2023-03-21T07:50:20Z",
"timestamp": 1679385020000
},
"deposited": {
"date-parts": [
[
2023,
3,
21
]
],
"date-time": "2023-03-21T07:50:21Z",
"timestamp": 1679385021000
},
"indexed": {
"date-parts": [
[
2023,
3,
22
]
],
"date-time": "2023-03-22T05:18:53Z",
"timestamp": 1679462333339
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023
]
]
},
"language": "en",
"link": [
{
"URL": "https://www.panafrican-med-journal.com/content/article/44/142/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "4870",
"original-title": [],
"prefix": "10.11604",
"published": {
"date-parts": [
[
2023
]
]
},
"published-online": {
"date-parts": [
[
2023
]
]
},
"publisher": "Pan African Medical Journal",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.panafrican-med-journal.com/content/article/44/142/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Factors associated with COVID-19 fatality among patients admitted in Mashonaland West Province, Zimbabwe 2020-2022: a secondary data analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.11604/pamj.2016.07.30.0001",
"volume": "44"
}