Sex Differences in Association Between Anti-Hypertensive Medications and Risk of COVID-19 in Middle-Aged and Older Adults
et al., Drugs & Aging, doi:10.1007/s40266-021-00886-y, Aug 2021
UK Biobank retrospective 77,271 patients aged 50-86, showing no significant differences with aspirin use. Matching lead to different results for the gender vs. overall analysis, for example the overall result for cases was OR 1.07, however both gender results are lower OR 0.97 and 1.02.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 9.0% lower, OR 0.91, p = 0.12, treatment 12,471, control 64,750, RR approximated with OR.
|
|
risk of hospitalization, 2.0% lower, OR 0.98, p = 0.47, treatment 12,471, control 64,750, RR approximated with OR.
|
|
risk of symptomatic case, 9.0% higher, OR 1.09, p = 0.18, treatment 12,471, control 64,750, RR approximated with OR.
|
|
risk of case, 7.0% higher, OR 1.07, p = 0.09, treatment 12,471, control 64,750, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ma et al., 18 Aug 2021, retrospective, propensity score matching, United Kingdom, peer-reviewed, 9 authors.
Sex Differences in Association Between Anti-Hypertensive Medications and Risk of COVID-19 in Middle-Aged and Older Adults
Drugs & Aging, doi:10.1007/s40266-021-00886-y
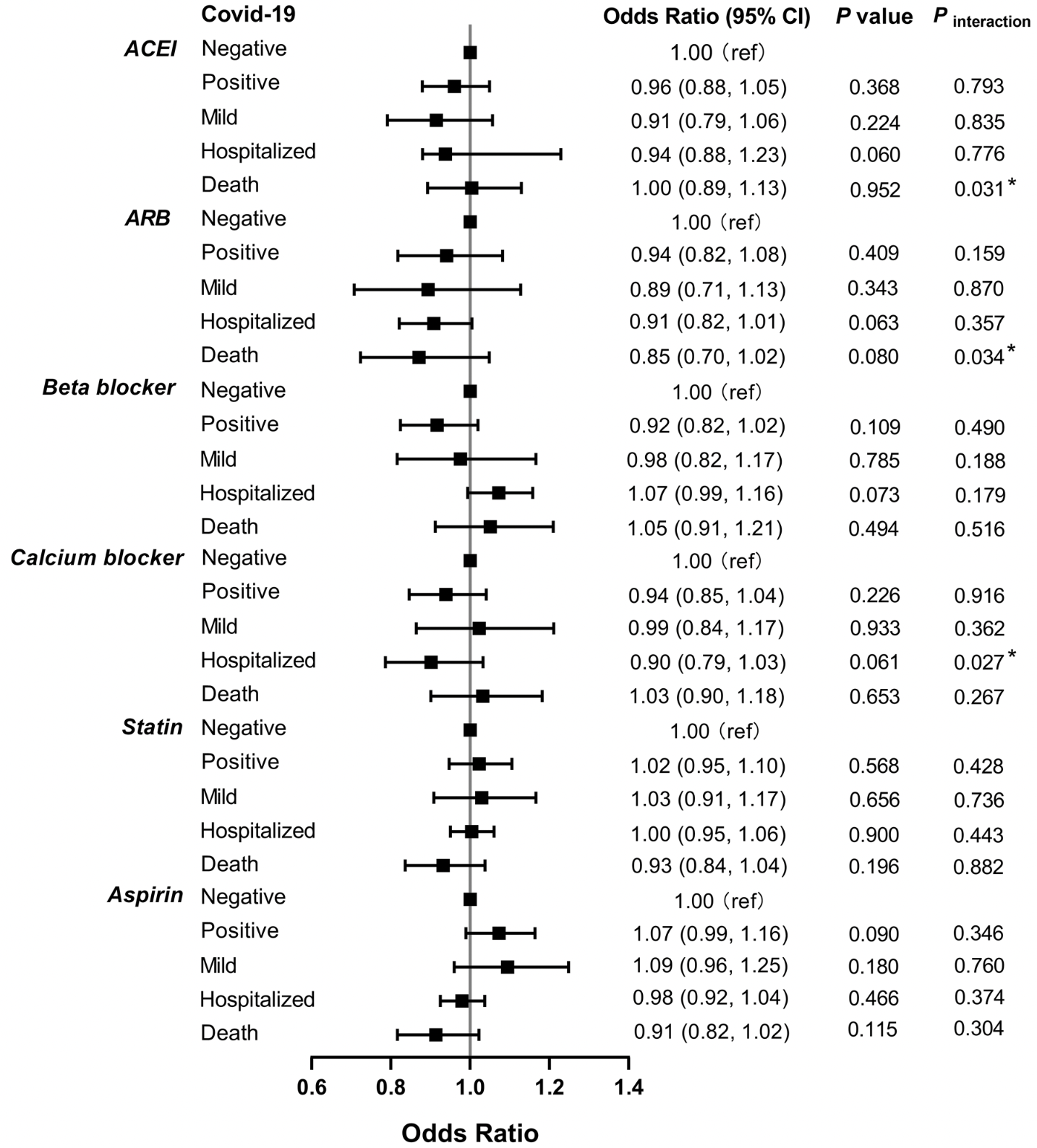
Background There is ongoing debate about the associations between drug therapies targeting the renin-angiotensin-aldosterone system (RAAS) and adverse outcomes in coronavirus disease 2019 . Objective This study aims to examine the associations between using medications for the cardiovascular system and the risks associated with COVID-19 in middle-aged and older adults. Methods A total of 77,221 participants (aged 50-86 years) from UK Biobank were tested for SARS-CoV-2 RNA. The medications included angiotensin-converting enzyme inhibitors (ACEI), angiotensin-receptor blockers (ARB), β-blockers, calcium channel blockers (CCB), statins, and aspirin. COVID-19 outcomes comprised a positive test result and severity of COVID-19 (defined as mild, hospitalization or death). We evaluated the risk among total participants and for sub-groups based on sex. Propensity score matching was performed 1:1 and logistic regression models were used. Results Among the middle-and older aged participants, no significant associations between any class of medications and the likelihood of COVID-19 infection were observed. ACEI were associated with a higher mortality risk from COVID-19 (odds ratio [OR] 1.15, 95% confidence interval [CI] 1.01-1.32) and CCB were associated with a lower hospitalization risk for COVID-19 (OR 0.87, 95% CI 0.79-0.96) among the male patients with COVID-19, while a lower mortality risk from COVID-19 (OR 0.67, 95% CI 0.47-0.96) was observed with ARB among the female patients with COVID-19. Conclusions The study suggested sex differences in the risk of death from COVID-19 with the use of ACEI and ARB among middle-aged and older adults. Sex differences in the risk of hospitalization for COVID-19 with the use of CCB was observed as well. It is of clinical importance that clinicians adopt different CVD treatment approaches for female and male patients with COVID-19.
Supplementary Information The online version contains supplementary material available at https:// doi. org/ 10. 1007/ s40266-021-00886-y.
Declarations Ethics approval This article does not contain any studies with human participants or animals performed by the authors. Authors' contributions YW directed the study. YW and YM designed the study and analyzed data. YM developed the first manuscript draft. YW, SL, HY and YZ edited the manuscript. All authors critically revised the manuscript, and all authors contributed to the final version.
References
Austin, Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies, Pharm Stat
Bessa, Jesus, Nunes, Pontes, Lacerda et al., Stimulation of the ACE2/Ang-(1-7)/Mas axis in hypertensive pregnant rats attenuates cardiovascular dysfunction in adult male offspring, Hypertens Res
Bianconi, Violi, Fallarino, Pignatelli, Sahebkar et al., Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19?, Drugs
Cariou, Goronflot, Rimbert, Boullu, May et al., Routine use of statins and increased COVID-19 related mortality in inpatients with type 2 diabetes: results from the CORONADO study, Diabetes Metab
Chen, Cao, Zhong, Host calcium channels and pumps in viral infections, Cells
Clerkin, Fried, Raikhelkar, Sayer, Griffin et al., COVID-19 and cardiovascular disease, Circulation
Deng, Yin, Chen, Zeng, Clinical determinants for fatality of 44,672 patients with COVID-19, Crit Care
Domińska, Involvement of ACE2/Ang-(1-7)/MAS1 axis in the regulation of ovarian function in mammals, Int J Mol Sci
Driggin, Madhavan, Bikdeli, Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic, J Am Coll Cardiol
Du, Tu, Zhu, Mu, Wang et al., Clinical features of 85 fatal cases of COVID-19 from Wuhan. A retrospective observational study, Am J Respir Crit Care Med
Dumanski, Ahmed, Sex, drugs, and adverse drug reactions: sex differences in laboratory monitoring outcomes after initiation of renin-angiotensin-aldosterone-system inhibition therapy, Circ Cardiovasc Qual Outcomes
Fujioka, Nishide, Ose, Suzuki, Kato et al., A sialylated voltage-dependent Ca 2+ channel binds hemagglutinin and mediates influenza A virus entry into mammalian cells, Cell Host Microbe
Guo, Fan, Chen, Wu, Zhang et al., Cardiovascular implications of fatal outcomes of patients with Coronavirus disease 2019 (COVID-19), JAMA Cardiol
Guo, Huang, Lin, Lv, Ma, of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers on onset and severity of severe acute respiratory syndrome coronavirus 2 infection, J Am Heart Assoc
Iaccarino, Grassi, Borghi, Ferri, Salvetti et al., Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian Society of hypertension, Hypertension
Kim, Kim, Kim, Kim, Kim et al., Compliance of antihypertensive medication and risk of Coronavirus Disease 2019: a cohort study using big data from the Korean National Health Insurance Service, J Korean Med Sci
Li, Zhou, Yang, You, Physiological and pathological regulation of ACE2, the SARS-CoV-2 receptor, Pharmacol Res
Lin, Lin, Lin, Hsu, Lin et al., Association between Angiotensin-converting enzyme inhibitors and lung cancer-a Nationwide, population-based, propensity score-matched cohort study, Cancers
Little, Non-steroidal anti-inflammatory drugs and COVID-19, BMJ
Lukassen, Chua, Trefzer, Kahn, Schneider et al., SARS-CoV-2 receptor ACE2 and TMPRSS2 are primarily expressed in bronchial transient secretory cells, EMBO J
Machuki, Zhang, Geng, Fu, Adzika et al., Estrogen regulation of cardiac cAMP-L-type Ca 2+ channel pathway modulates sex differences in basal contraction and responses to β 2 AR-mediated stress in left ventricular apical myocytes, Cell Commun Signal
Mancia, Rea, Ludergnani, Apolone, Corrao, Renin-Angiotensin-Aldosterone system blockers and the risk of Covid-19, N Engl J Med
Mechanick, Rosenson, Pinney, Mancini, Narula et al., Coronavirus and cardiometabolic syndrome: JACC focus seminar, J Am Coll Cardiol
Medzikovic, Cunningham, Li, Amjedi, Hong et al., Sex differences underlying preexisting cardiovascular disease and cardiovascular injury in COVID-19, J Mol Cell Cardiol
Nicin, Abplanalp, Mellentin, Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts, Eur Heart J
Regitz-Zagrosek, Kararigas, Mechanistic pathways of sex differences in cardiovascular disease, Physiol Rev
Reynolds, Adhikari, Pulgarin, Troxel, Iturrate et al., Renin-Angiotensin-Aldosterone system inhibitors and risk of Covid-19, N Engl J Med
Rosa, Spaccarotella, Basso, Calabrò, Curcio et al., Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era, Eur Heart J
Sama, Ravera, Santema, Van Goor, Maaten et al., Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors, Eur Heart J
Santos, Sampaio, Alzamora, Motta-Santos, Alenina et al., The ACE2/Angiotensin-(1-7)/MAS axis of the Renin-Angiotensin system: focus on Angiotensin-(1-7), Physiol Rev
Serfozo, Wysocki, Gulua, Schulze, Ye et al., Ang II (Angiotensin II) conversion to angiotensin-(1-7) in the circulation Is POP (Prolyloligopeptidase)-dependent and ACE2 (Angiotensin-Converting Enzyme 2)-independent, Hypertension
South, Tomlinson, Edmonston, Hiremath, Sparks, Controversies of renin-angiotensin system inhibition during the COVID-19 pandemic, Nat Rev Nephrol
Tukiainen, Villani, Rivas, Marshall, Satija, Landscape of X chromosome inactivation across human tissues, Nature
Vaduganathan, Vardeny, Michel, Mcmurray, Pfeffer et al., Renin-Angiotensin-Aldosterone system inhibitors in patients with Covid-19, N Engl J Med
Vignera, Cannarella, Condorelli, Torre, Aversa et al., Sex-specific SARS-CoV-2 mortality: among hormonemodulated ACE2 expression, risk of venous thromboembolism and hypovitaminosis D, Int J Mol Sci
Viveiros, Rasmuson, Vu, Mulvagh, Yip et al., Sex differences in COVID-19: candidate pathways, genetics of ACE2, and sex hormones, Am J Physiol Heart Circ Physiol
Wasserstrom, Kapur, Jones, Faruque, Sharma et al., Characteristics of intracellular Ca 2+ cycling in intact rat heart: a comparison of sex differences, Am J Physiol Heart Circ Physiol
Yan, Valdes, Vijay, Wang, Liang et al., Role of drugs used for chronic disease management on susceptibility and severity of COVID-19: a large case-control study, Clin Pharmacol Ther
Zhang, Zhu, Cai, Lei, Qin et al., Association of inpatient use of Angiotensin-converting enzyme inhibitors and Angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19, Circ Res
Ziegler, Allon, Nyquist, Mbano, Miao et al., SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues, Cell
DOI record:
{
"DOI": "10.1007/s40266-021-00886-y",
"ISSN": [
"1170-229X",
"1179-1969"
],
"URL": "http://dx.doi.org/10.1007/s40266-021-00886-y",
"alternative-id": [
"886"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "8 July 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 2,
"value": "18 August 2021"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Funding",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "This study was supported by The National Natural Science Foundation of China (71910107004)."
},
{
"group": {
"label": "Conflicts of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "The authors declare no conflict of interest."
},
{
"group": {
"label": "Ethics approval",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "This article does not contain any studies with human participants or animals performed by the authors."
},
{
"group": {
"label": "Data availability",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 5,
"value": "The authors can confirm that all relevant data are included in the article and/or its supplementary information files."
},
{
"group": {
"label": "Authors' contributions",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 6,
"value": "YW directed the study. YW and YM designed the study and analyzed data. YM developed the first manuscript draft. YW, SL, HY and YZ edited the manuscript. All authors critically revised the manuscript, and all authors contributed to the final version."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"affiliation": [],
"family": "Ma",
"given": "Yue",
"sequence": "first"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Yuan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Shu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yang",
"given": "Hongxi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Huiping",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cao",
"given": "Zhi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xu",
"given": "Fusheng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sun",
"given": "Li",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2493-6471",
"affiliation": [],
"authenticated-orcid": false,
"family": "Wang",
"given": "Yaogang",
"sequence": "additional"
}
],
"container-title": [
"Drugs & Aging"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
8,
18
]
],
"date-time": "2021-08-18T02:02:17Z",
"timestamp": 1629252137000
},
"deposited": {
"date-parts": [
[
2021,
9,
30
]
],
"date-time": "2021-09-30T17:41:44Z",
"timestamp": 1633023704000
},
"funder": [
{
"DOI": "10.13039/501100001809",
"award": [
"71910107004"
],
"doi-asserted-by": "publisher",
"name": "National Natural Science Foundation of China"
}
],
"indexed": {
"date-parts": [
[
2021,
12,
16
]
],
"date-time": "2021-12-16T17:52:20Z",
"timestamp": 1639677140581
},
"is-referenced-by-count": 1,
"issn-type": [
{
"type": "print",
"value": "1170-229X"
},
{
"type": "electronic",
"value": "1179-1969"
}
],
"issue": "10",
"issued": {
"date-parts": [
[
2021,
8,
18
]
]
},
"journal-issue": {
"issue": "10",
"published-print": {
"date-parts": [
[
2021,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
18
]
],
"date-time": "2021-08-18T00:00:00Z",
"timestamp": 1629244800000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
18
]
],
"date-time": "2021-08-18T00:00:00Z",
"timestamp": 1629244800000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s40266-021-00886-y.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s40266-021-00886-y/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s40266-021-00886-y.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "921-930",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2021,
8,
18
]
]
},
"published-online": {
"date-parts": [
[
2021,
8,
18
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "886_CR1",
"unstructured": "WHO Coronavirus Disease (COVID-19) Dashboard. 2021. https://covid19.who.int/. Accessed 9 Jun 2021."
},
{
"DOI": "10.1001/jamacardio.2020.1017",
"author": "T Guo",
"doi-asserted-by": "publisher",
"first-page": "811",
"issue": "7",
"journal-title": "JAMA Cardiol.",
"key": "886_CR2",
"unstructured": "Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with Coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811–8.",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.03.031",
"author": "E Driggin",
"doi-asserted-by": "publisher",
"first-page": "2352",
"issue": "18",
"journal-title": "J Am Coll Cardiol",
"key": "886_CR3",
"unstructured": "Driggin E, Madhavan MV, Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–71.",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.04.035",
"author": "CGK Ziegler",
"doi-asserted-by": "publisher",
"first-page": "1016",
"issue": "5",
"journal-title": "Cell",
"key": "886_CR4",
"unstructured": "Ziegler CGK, Allon SJ, Nyquist SK, Mbano IM, Miao VN, Tzouanas CN, et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181(5):1016–35.",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1056/NEJMsr2005760",
"author": "M Vaduganathan",
"doi-asserted-by": "publisher",
"first-page": "1653",
"issue": "17",
"journal-title": "N Engl J Med",
"key": "886_CR5",
"unstructured": "Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin-Angiotensin-Aldosterone system inhibitors in patients with Covid-19. N Engl J Med. 2020;382(17):1653–9.",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1038/s41581-020-0279-4",
"author": "AM South",
"doi-asserted-by": "publisher",
"first-page": "305",
"issue": "6",
"journal-title": "Nat Rev Nephrol",
"key": "886_CR6",
"unstructured": "South AM, Tomlinson L, Edmonston D, Hiremath S, Sparks MA. Controversies of renin-angiotensin system inhibition during the COVID-19 pandemic. Nat Rev Nephrol. 2020;16(6):305–7.",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1161/HYPERTENSIONAHA.119.14071",
"author": "P Serfozo",
"doi-asserted-by": "publisher",
"first-page": "173",
"issue": "1",
"journal-title": "Hypertension",
"key": "886_CR7",
"unstructured": "Serfozo P, Wysocki J, Gulua G, Schulze A, Ye M, Liu P, et al. Ang II (Angiotensin II) conversion to angiotensin-(1–7) in the circulation Is POP (Prolyloligopeptidase)-dependent and ACE2 (Angiotensin-Converting Enzyme 2)-independent. Hypertension. 2020;75(1):173–82.",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2008975",
"author": "HR Reynolds",
"doi-asserted-by": "publisher",
"first-page": "2441",
"issue": "25",
"journal-title": "N Engl J Med",
"key": "886_CR8",
"unstructured": "Reynolds HR, Adhikari S, Pulgarin C, Troxel AB, Iturrate E, Johnson SB, et al. Renin-Angiotensin-Aldosterone system inhibitors and risk of Covid-19. N Engl J Med. 2020;382(25):2441–8.",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317134",
"author": "P Zhang",
"doi-asserted-by": "publisher",
"first-page": "1671",
"issue": "12",
"journal-title": "Circ Res",
"key": "886_CR9",
"unstructured": "Zhang P, Zhu L, Cai J, Lei F, Qin JJ, Xie J, et al. Association of inpatient use of Angiotensin-converting enzyme inhibitors and Angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020;126(12):1671–81.",
"volume": "126",
"year": "2020"
},
{
"DOI": "10.1161/JAHA.120.016219",
"author": "J Guo",
"doi-asserted-by": "publisher",
"first-page": "e016219",
"issue": "7",
"journal-title": "J Am Heart Assoc",
"key": "886_CR10",
"unstructured": "Guo J, Huang Z, Lin L, Lv J. Coronavirus disease 2019 (COVID-19) and cardiovascular disease: a viewpoint on the potential influence of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers on onset and severity of severe acute respiratory syndrome coronavirus 2 infection. J Am Heart Assoc. 2020;9(7):e016219.",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.10.001",
"author": "B Cariou",
"doi-asserted-by": "publisher",
"first-page": "101202",
"issue": "2",
"journal-title": "Diabetes Metab",
"key": "886_CR11",
"unstructured": "Cariou B, Goronflot T, Rimbert A, Boullu S, Le May C, Moulin P, et al. Routine use of statins and increased COVID-19 related mortality in inpatients with type 2 diabetes: results from the CORONADO study. Diabetes Metab. 2021;47(2):101202.",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1007/s40265-020-01365-1",
"author": "V Bianconi",
"doi-asserted-by": "publisher",
"first-page": "1383",
"issue": "14",
"journal-title": "Drugs",
"key": "886_CR12",
"unstructured": "Bianconi V, Violi F, Fallarino F, Pignatelli P, Sahebkar A, Pirro M.Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19? Drugs. 2020;80(14):1383–96.",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1161/CIRCOUTCOMES.120.007045",
"author": "SM Dumanski",
"doi-asserted-by": "publisher",
"first-page": "e007045",
"issue": "9",
"journal-title": "Circ Cardiovasc Qual Outcomes.",
"key": "886_CR13",
"unstructured": "Dumanski SM, Ahmed SB. Sex, drugs, and adverse drug reactions: sex differences in laboratory monitoring outcomes after initiation of renin-angiotensin-aldosterone-system inhibition therapy. Circ Cardiovasc Qual Outcomes. 2020;13(9):e007045.",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.15252/embj.2020105114",
"author": "S Lukassen",
"doi-asserted-by": "publisher",
"first-page": "e105114",
"issue": "10",
"journal-title": "EMBO J",
"key": "886_CR14",
"unstructured": "Lukassen S, Chua RL, Trefzer T, Kahn NC, Schneider MA, Muley T, et al. SARS-CoV-2 receptor ACE2 and TMPRSS2 are primarily expressed in bronchial transient secretory cells. EMBO J. 2020;39(10):e105114.",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.3390/ijms21134572",
"author": "K Domińska",
"doi-asserted-by": "publisher",
"first-page": "4572",
"issue": "13",
"journal-title": "Int J Mol Sci",
"key": "886_CR15",
"unstructured": "Domińska K. Involvement of ACE2/Ang-(1–7)/MAS1 axis in the regulation of ovarian function in mammals. Int J Mol Sci. 2020;21(13):4572.",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.yjmcc.2020.08.007",
"author": "L Medzikovic",
"doi-asserted-by": "publisher",
"first-page": "25",
"journal-title": "J Mol Cell Cardiol",
"key": "886_CR16",
"unstructured": "Medzikovic L, Cunningham CM, Li M, Amjedi M, Hong J, Ruffenach G, et al. Sex differences underlying preexisting cardiovascular disease and cardiovascular injury in COVID-19. J Mol Cell Cardiol. 2020;148:25–33.",
"volume": "148",
"year": "2020"
},
{
"DOI": "10.3390/ijms21082948",
"author": "S La Vignera",
"doi-asserted-by": "publisher",
"first-page": "2948",
"issue": "8",
"journal-title": "Int J Mol Sci",
"key": "886_CR17",
"unstructured": "La Vignera S, Cannarella R, Condorelli RA, Torre F, Aversa A, Calogero AE. Sex-specific SARS-CoV-2 mortality: among hormone-modulated ACE2 expression, risk of venous thromboembolism and hypovitaminosis D. Int J Mol Sci. 2020;21(8):2948.",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1002/pst.433",
"author": "PC Austin",
"doi-asserted-by": "publisher",
"first-page": "150",
"issue": "2",
"journal-title": "Pharm Stat",
"key": "886_CR18",
"unstructured": "Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10(2):150–61.",
"volume": "10",
"year": "2011"
},
{
"DOI": "10.1016/j.phrs.2020.104833",
"author": "Y Li",
"doi-asserted-by": "publisher",
"first-page": "104833",
"journal-title": "Pharmacol Res",
"key": "886_CR19",
"unstructured": "Li Y, Zhou W, Yang L, You R. Physiological and pathological regulation of ACE2, the SARS-CoV-2 receptor. Pharmacol Res. 2020;157:104833.",
"volume": "157",
"year": "2020"
},
{
"DOI": "10.1038/nature24265",
"author": "T Tukiainen",
"doi-asserted-by": "publisher",
"first-page": "244",
"issue": "7675",
"journal-title": "Nature",
"key": "886_CR20",
"unstructured": "Tukiainen T, Villani AC, Yen A, Rivas MA, Marshall JL, Satija R, et al. Landscape of X chromosome inactivation across human tissues. Nature. 2017;550(7675):244–8.",
"volume": "550",
"year": "2017"
},
{
"DOI": "10.1038/s41440-019-0321-8",
"author": "ASM Bessa",
"doi-asserted-by": "publisher",
"first-page": "1883",
"issue": "12",
"journal-title": "Hypertens Res",
"key": "886_CR21",
"unstructured": "Bessa ASM, Jesus ÉF, Nunes ADC, Pontes CNR, Lacerda IS, Costa JM, et al. Stimulation of the ACE2/Ang-(1–7)/Mas axis in hypertensive pregnant rats attenuates cardiovascular dysfunction in adult male offspring. Hypertens Res. 2019;42(12):1883–93.",
"volume": "42",
"year": "2019"
},
{
"DOI": "10.1152/physrev.00023.2016",
"author": "RAS Santos",
"doi-asserted-by": "publisher",
"first-page": "505",
"issue": "1",
"journal-title": "Physiol Rev",
"key": "886_CR22",
"unstructured": "Santos RAS, Sampaio WO, Alzamora AC, Motta-Santos D, Alenina N, Bader M, et al. The ACE2/Angiotensin-(1–7)/MAS axis of the Renin-Angiotensin system: focus on Angiotensin-(1–7). Physiol Rev. 2018;98(1):505–53.",
"volume": "98",
"year": "2018"
},
{
"DOI": "10.1093/eurheartj/ehaa373",
"author": "IE Sama",
"doi-asserted-by": "publisher",
"first-page": "1810",
"journal-title": "Eur Heart J",
"key": "886_CR23",
"unstructured": "Sama IE, Ravera A, Santema BT, van Goor H, Ter Maaten JM, Cleland JGF, et al. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Heart J. 2020;41:1810–7.",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.3390/cells9010094",
"author": "X Chen",
"doi-asserted-by": "publisher",
"first-page": "94",
"issue": "1",
"journal-title": "Cells",
"key": "886_CR24",
"unstructured": "Chen X, Cao R, Zhong W. Host calcium channels and pumps in viral infections. Cells. 2019;9(1):94.",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1016/j.chom.2018.04.015",
"author": "Y Fujioka",
"doi-asserted-by": "publisher",
"first-page": "809",
"issue": "6",
"journal-title": "Cell Host Microbe",
"key": "886_CR25",
"unstructured": "Fujioka Y, Nishide S, Ose T, Suzuki T, Kato I, Fukuhara H, et al. A sialylated voltage-dependent Ca2+ channel binds hemagglutinin and mediates influenza A virus entry into mammalian cells. Cell Host Microbe. 2018;23(6):809–18.",
"volume": "23",
"year": "2018"
},
{
"DOI": "10.1152/ajpheart.00469.2008",
"author": "JA Wasserstrom",
"doi-asserted-by": "publisher",
"first-page": "H1895",
"issue": "5",
"journal-title": "Am J Physiol Heart Circ Physiol",
"key": "886_CR26",
"unstructured": "Wasserstrom JA, Kapur S, Jones S, Faruque T, Sharma R, Kelly JE, et al. Characteristics of intracellular Ca2+ cycling in intact rat heart: a comparison of sex differences. Am J Physiol Heart Circ Physiol. 2008;295(5):H1895–904.",
"volume": "295",
"year": "2008"
},
{
"DOI": "10.1186/s12964-019-0346-2",
"author": "JO Machuki",
"doi-asserted-by": "publisher",
"first-page": "34",
"issue": "1",
"journal-title": "Cell Commun Signal",
"key": "886_CR27",
"unstructured": "Machuki JO, Zhang HY, Geng J, Fu L, Adzika GK, Wu L, et al. Estrogen regulation of cardiac cAMP-L-type Ca2+ channel pathway modulates sex differences in basal contraction and responses to β2AR-mediated stress in left ventricular apical myocytes. Cell Commun Signal. 2019;17(1):34.",
"volume": "17",
"year": "2019"
},
{
"DOI": "10.1152/ajpheart.00755.2020",
"author": "A Viveiros",
"doi-asserted-by": "publisher",
"first-page": "H296",
"issue": "1",
"journal-title": "Am J Physiol Heart Circ Physiol",
"key": "886_CR28",
"unstructured": "Viveiros A, Rasmuson J, Vu J, Mulvagh SL, Yip CYY, Norris CM, Oudit GY. Sex differences in COVID-19: candidate pathways, genetics of ACE2, and sex hormones. Am J Physiol Heart Circ Physiol. 2021;320(1):H296–304.",
"volume": "320",
"year": "2021"
},
{
"DOI": "10.1152/physrev.00021.2015",
"author": "V Regitz-Zagrosek",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Physiol Rev",
"key": "886_CR29",
"unstructured": "Regitz-Zagrosek V, Kararigas G. Mechanistic pathways of sex differences in cardiovascular disease. Physiol Rev. 2017;97(1):1–37.",
"volume": "97",
"year": "2017"
},
{
"DOI": "10.1186/s13054-020-02902-w",
"author": "G Deng",
"doi-asserted-by": "publisher",
"first-page": "179",
"issue": "1",
"journal-title": "Crit Care",
"key": "886_CR30",
"unstructured": "Deng G, Yin M, Chen X, Zeng F. Clinical determinants for fatality of 44,672 patients with COVID-19. Crit Care. 2020;24(1):179.",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1093/eurheartj/ehaa409",
"author": "S De Rosa",
"doi-asserted-by": "publisher",
"first-page": "2083",
"issue": "22",
"journal-title": "Eur Heart J",
"key": "886_CR31",
"unstructured": "De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41(22):2083–8.",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1164/rccm.202003-0543OC",
"author": "Y Du",
"doi-asserted-by": "publisher",
"first-page": "1372",
"issue": "11",
"journal-title": "Am J Respir Crit Care Med",
"key": "886_CR32",
"unstructured": "Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan. A retrospective observational study. Am J Respir Crit Care Med. 2020;201(11):1372–9.",
"volume": "201",
"year": "2020"
},
{
"DOI": "10.3346/jkms.2020.35.e232",
"author": "J Kim",
"doi-asserted-by": "publisher",
"first-page": "e232",
"issue": "25",
"journal-title": "J Korean Med Sci",
"key": "886_CR33",
"unstructured": "Kim J, Kim DW, Kim KI, Kim HB, Kim JH, Lee YG, et al. Compliance of antihypertensive medication and risk of Coronavirus Disease 2019: a cohort study using big data from the Korean National Health Insurance Service. J Korean Med Sci. 2020;35(25):e232.",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1002/cpt.2047",
"author": "H Yan",
"doi-asserted-by": "publisher",
"first-page": "1185",
"journal-title": "Clin Pharmacol Ther",
"key": "886_CR34",
"unstructured": "Yan H, Valdes AM, Vijay A, Wang S, Liang L, Yang S, et al. Role of drugs used for chronic disease management on susceptibility and severity of COVID-19: a large case-control study. Clin Pharmacol Ther. 2020;108:1185–94.",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.046941",
"author": "KJ Clerkin",
"doi-asserted-by": "publisher",
"first-page": "1648",
"issue": "20",
"journal-title": "Circulation",
"key": "886_CR35",
"unstructured": "Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, et al. COVID-19 and cardiovascular disease. Circulation. 2020;141(20):1648–55.",
"volume": "141",
"year": "2020"
},
{
"DOI": "10.1093/eurheartj/ehaa311",
"author": "L Nicin",
"doi-asserted-by": "publisher",
"first-page": "1804",
"issue": "19",
"journal-title": "Eur Heart J",
"key": "886_CR36",
"unstructured": "Nicin L, Abplanalp WT, Mellentin H. Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts. Eur Heart J. 2020;41(19):1804–6.",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.3390/cancers12030747",
"author": "SY Lin",
"doi-asserted-by": "publisher",
"first-page": "747",
"issue": "3",
"journal-title": "Cancers (Basel).",
"key": "886_CR37",
"unstructured": "Lin SY, Lin CL, Lin CC, Hsu WH, Lin CD, Wang IK, et al. Association between Angiotensin-converting enzyme inhibitors and lung cancer—a Nationwide, population-based, propensity score-matched cohort study. Cancers (Basel). 2020;12(3):747.",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.07.069",
"author": "JI Mechanick",
"doi-asserted-by": "publisher",
"first-page": "2024",
"issue": "17",
"journal-title": "J Am Coll Cardiol",
"key": "886_CR38",
"unstructured": "Mechanick JI, Rosenson RS, Pinney SP, Mancini DM, Narula J, Fuster V. Coronavirus and cardiometabolic syndrome: JACC focus seminar. J Am Coll Cardiol. 2020;76(17):2024–35.",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1185",
"author": "P Little",
"doi-asserted-by": "publisher",
"first-page": "m1185",
"journal-title": "BMJ",
"key": "886_CR39",
"unstructured": "Little P. Non-steroidal anti-inflammatory drugs and COVID-19. BMJ. 2020;368:m1185.",
"volume": "368",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2006923",
"author": "G Mancia",
"doi-asserted-by": "publisher",
"first-page": "2431",
"issue": "25",
"journal-title": "N Engl J Med",
"key": "886_CR40",
"unstructured": "Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G. Renin-Angiotensin-Aldosterone system blockers and the risk of Covid-19. N Engl J Med. 2020;382(25):2431–40.",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1161/HYPERTENSIONAHA.120.15324",
"author": "G Iaccarino",
"doi-asserted-by": "publisher",
"first-page": "366",
"issue": "2",
"journal-title": "Hypertension.",
"key": "886_CR41",
"unstructured": "Iaccarino G, Grassi G, Borghi C, Ferri C, Salvetti M, Volpe M, et al. Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian Society of hypertension. Hypertension. 2020;76(2):366–72.",
"volume": "76",
"year": "2020"
}
],
"reference-count": 41,
"references-count": 41,
"relation": {},
"score": 1,
"short-container-title": [
"Drugs Aging"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology (medical)",
"Geriatrics and Gerontology"
],
"subtitle": [],
"title": [
"Sex Differences in Association Between Anti-Hypertensive Medications and Risk of COVID-19 in Middle-Aged and Older Adults"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "38"
}