Clinical, behavioural and social factors associated with racial disparities in COVID-19 patients from an integrated healthcare system in Georgia: a retrospective cohort study
et al., BMJ Open, doi:10.1136/bmjopen-2020-044052, May 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
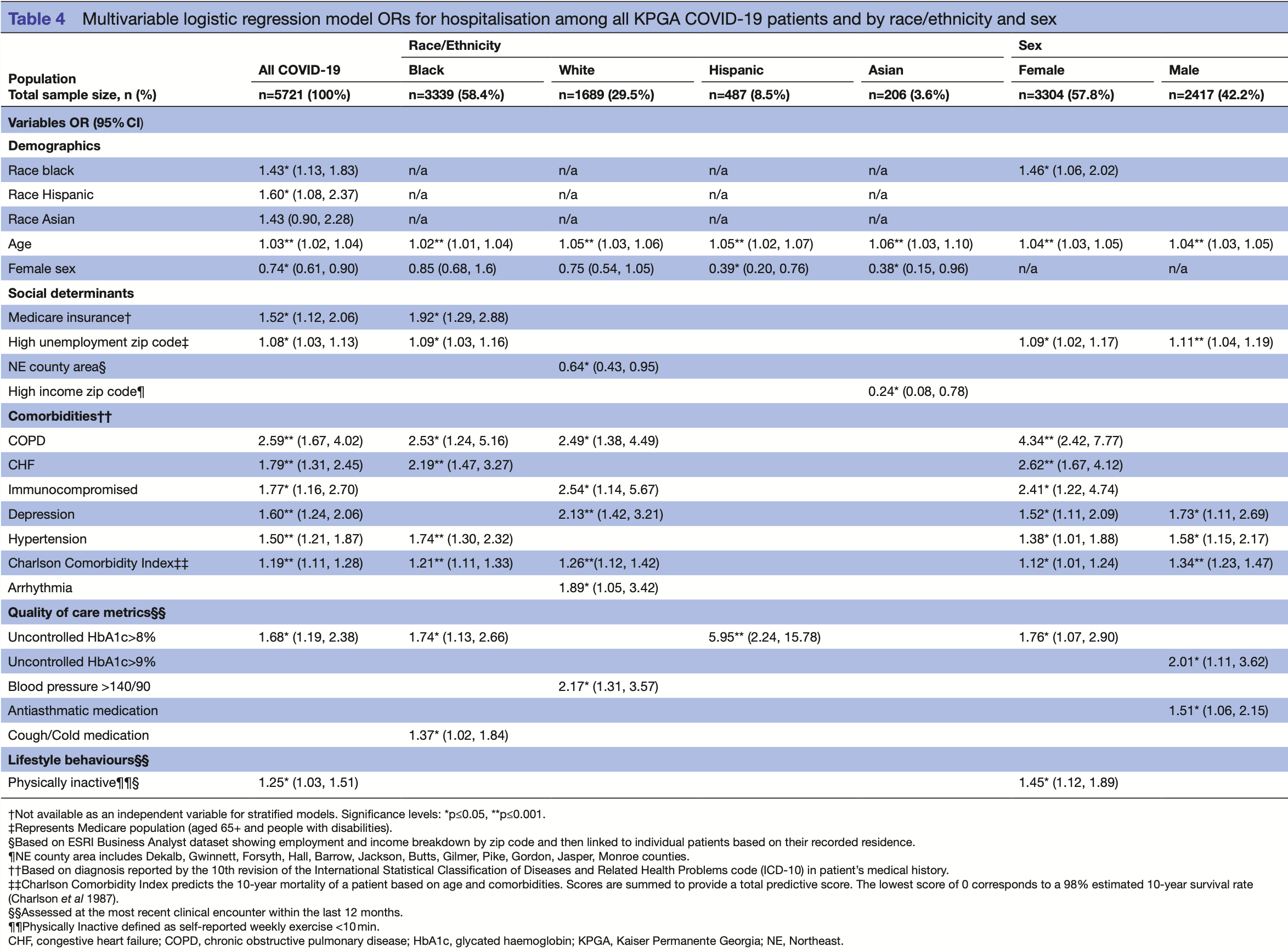
Retrospective 5,712 COVID-19 patients in the USA, showing higher risk of COVID-19 hospitalization with a history of physical inactivity.
|
risk of hospitalization, 20.0% lower, OR 0.80, p = 0.02, high activity levels 2,121, low activity levels 1,648, adjusted per study, inverted to make OR<1 favor high activity levels, active vs. inactive, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Lobelo et al., 19 May 2021, retrospective, Georgia, peer-reviewed, 7 authors, study period 3 March, 2020 - 29 October, 2020.
Contact: felipe.lobelo@kp.org.
Clinical, behavioural and social factors associated with racial disparities in COVID-19 patients from an integrated healthcare system in Georgia: a retrospective cohort study
BMJ Open, doi:10.1136/bmjopen-2020-044052
Objectives To identify sociodemographic, clinical and behavioural drivers of racial disparities and their association with clinical outcomes among Kaiser Permanente Georgia (KPGA) members with COVID-19. Design Retrospective cohort of patients with COVID-19 seen from 3 March to 29 October 2020. We described the distribution of underlying comorbidities, quality of care metrics, demographic and social determinants of health (SDOH) indicators across race groups. We also described clinical outcomes in hospitalised patients including length of stay, intensive care unit (ICU) admission, readmission and mortality. We performed multivariable analyses for hospitalisation risk among all patients with COVID-19 and stratifyied by race and sex. Setting KPGA, an integrated healthcare system. Participants 5712 patients who all had laboratoryconfirmed COVID-19. Of them, 57.8% were female, 58.4% black, 29.5% white, 8.5% Hispanic and 3.6% Asian. Results Black patients had the highest proportions of living in neighborhoods under the federal poverty line (12.4%) and in more deprived locations (neighbourhood deprivation index=0.4). Overall, 14.4% (n=827) of this cohort was hospitalised. Asian patients had the highest rates of ICU admission (53.1%) and mechanical ventilation (21.9%). Among all patients, Hispanics (adjusted 1.60, 95% CI (1.08, 2.37)), blacks (1.43 (1.13, 1.83)), age in years (1.03 (1.02, 1.04)) and living in a zip code with high unemployment (1.08 (1.03, 1.13)) were associated with higher odds of hospitalisation. COVID-19 patients with chronic obstructive pulmonary disease ( 2 .59 (1.67, 4.02)), chronic heart failure (1.79 (1.31, 2.45)), immunocompromised (1.77 (1.16, 2.70)), with glycated haemoglobin >8% (1.68 (1.19, 2.38)), depression (1.60 (1.24, 2.06)), hypertension (1.5 (1.21, 1.87)) and physical inactivity (1.25 (1.03, 1.51)) had higher odds of hospitalisation. Conclusions Black and Hispanic KPGA patients were at higher odds of hospitalisation, but not mortality, compared with other race groups. Beyond previously reported sociodemographics and comorbidities, factors such as quality of care, lifestyle behaviours and SDOH indicators should be considered when designing and implementing interventions to reduce COVID-19 racial disparities. ► To our knowledge, this is the first COVID-19 retrospective cohort study to incorporate multiple individual and community-level social determinants of health indicators, pre-pandemic lifestyle behaviours and comorbidity management metrics as drivers of COVID-19 racial disparities.
Competing interests None declared. Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research. Patient consent for publication Not required.
Ethics approval The KPGA institutional review board approved this study with a waiver of informed consent. Provenance and peer review Not commissioned; externally peer reviewed.
References
Andrews, Tamura, Claudel, Geospatial analysis of neighborhood deprivation index (NDI) for the United States by County, J Maps, doi:10.1080/17445647.2020.1750066
Arcgis, Esri Demographics -Tapestry Segmentation: ArcGIS
Azar, Shen, Romanelli, Disparities in outcomes among COVID-19 patients in a large health care system in California, Health Aff, doi:10.1377/hlthaff.2020.00598
Bryan, Davis, Chokshi, Moving from the five whys to five Hows: addressing racial inequities in COVID-19 infection and death, Health Aff, doi:10.1377/hblog20200625.389260
Ceriello, Schnell, COVID-19: considerations of diabetes and cardiovascular disease management, J Diabetes Sci Technol, doi:10.1177/1932296820930025
Clark, Jit, Gash, Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study, Lancet Glob Health, doi:10.1016/S2214-109X(20)30264-3
Coleman, Ngor, Reynolds, Initial validation of an exercise "vital sign" in electronic medical records, Med Sci Sports Exerc, doi:10.1249/MSS.0b013e3182630ec1
Deyo, Cherkin, Ciol, Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases, J Clin Epidemiol, doi:10.1016/0895-4356(92)90133-8
Eg, Burton, Fort, Hospitalization and mortality among black patients and white patients with Covid-19, N Engl J Med, doi:10.1056/NEJMsa2011686
Ga, Jones, Benkeser, Assessing differential impacts of COVID-19 on black communities, Ann Epidemiol, doi:10.1016/j.annepidem.2020.05.003
Gold, Wong, Szablewski, Characteristics and Clinical Outcomes of Adult Patients Hospitalized with COVID-19 -Georgia, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6918e1
Gu, Mack, Salvatore, Characteristics associated with racial/ethnic disparities in COVID-19 outcomes in an academic health care system, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.25197
Hales, Carroll, Fryar, Prevalence of obesity and severe obesity among adults: United States, 2017-2018, NCHS data brief
Henson, Yates, Edwardson, Sedentary time and markers of chronic low-grade inflammation in a high risk population, PLoS One, doi:10.1371/journal.pone.0078350
Hyattsville, None
Killerby, Link-Gelles, Haight, Characteristics Associated with Hospitalization Among Patients with COVID-19, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6925e1
Lobelo, Young, Sallis, Routine assessment and promotion of physical activity in healthcare settings: a scientific statement from the American heart association, Circulation, doi:10.1161/CIR.0000000000000559
Messer, Laraia, Kaufman, The development of a standardized neighborhood deprivation index, J Urban Health, doi:10.1007/s11524-006-9094-x
Metro, Chamber, Profile of Metro Atlanta
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J Sport Health Sci, doi:10.1016/j.jshs.2018.09.009
Parodi, Young, Bellows, Kaiser, Permanente's system capabilities to suppress Covid-19
Poulson, Neufeld, Geary, Intersectional disparities among Hispanic groups in COVID-19 outcomes, J Immigr Minor Health, doi:10.1007/s10903-020-01111-5
Powell, King, Buchner, The scientific foundation for the physical activity guidelines for Americans, 2nd edition, J Phys Act Health, doi:10.1123/jpah.2018-0618
Renelus, Khoury, Chandrasekaran, Racial disparities in COVID-19 hospitalization and in-hospital mortality at the height of the new York City pandemic, J Racial Ethn Health Disparities, doi:10.1007/s40615-020-00872-x
Rentsch, Kidwai-Khan, Tate, Covid-19 by race and ethnicity: a national cohort study of 6 million United States veterans, doi:10.1101/2020.05.12.20099135
Rodriguez, Solomon, De Lemos, Racial and Ethnic Differences in Presentation and Outcomes for Patients Hospitalized with COVID-19: Findings from the American Heart Association's COVID-19 Cardiovascular Disease Registry, Circulation, doi:10.1161/CIRCULATIONAHA.120.052278
Sallis, Pratt, A call to action: physical activity and COVID-19 exercise is medicine
Shabto, Loerinc, Keefe, Characteristics and outcomes of COVID-19 positive patients with diabetes managed as outpatients, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108229
Song, Ren, Sun, Benefits of exercise on influenza or pneumonia in older adults: a systematic review, Int J Environ Res Public Health, doi:10.3390/ijerph17082655
Suleyman, Fadel, Malette, Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.12270
Young, Coleman, Ngor, Associations between physical activity and cardiometabolic risk factors assessed in a southern California health care system, Prev Chronic Dis, doi:10.5888/pcd11.140196
DOI record:
{
"DOI": "10.1136/bmjopen-2020-044052",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2020-044052",
"abstract": "<jats:sec><jats:title>Objectives</jats:title><jats:p>To identify sociodemographic, clinical and behavioural drivers of racial disparities and their association with clinical outcomes among Kaiser Permanente Georgia (KPGA) members with COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>Retrospective cohort of patients with COVID-19 seen from 3 March to 29 October 2020. We described the distribution of underlying comorbidities, quality of care metrics, demographic and social determinants of health (SDOH) indicators across race groups. We also described clinical outcomes in hospitalised patients including length of stay, intensive care unit (ICU) admission, readmission and mortality. We performed multivariable analyses for hospitalisation risk among all patients with COVID-19 and stratifyied by race and sex.</jats:p></jats:sec><jats:sec><jats:title>Setting</jats:title><jats:p>KPGA, an integrated healthcare system.</jats:p></jats:sec><jats:sec><jats:title>Participants</jats:title><jats:p>5712 patients who all had laboratory-confirmed COVID-19. Of them, 57.8% were female, 58.4% black, 29.5% white, 8.5% Hispanic and 3.6% Asian.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Black patients had the highest proportions of living in neighborhoods under the federal poverty line (12.4%) and in more deprived locations (neighbourhood deprivation index=0.4). Overall, 14.4% (n=827) of this cohort was hospitalised. Asian patients had the highest rates of ICU admission (53.1%) and mechanical ventilation (21.9%). Among all patients, Hispanics (adjusted 1.60, 95% CI (1.08, 2.37)), blacks (1.43 (1.13, 1.83)), age in years (1.03 (1.02, 1.04)) and living in a zip code with high unemployment (1.08 (1.03, 1.13)) were associated with higher odds of hospitalisation. COVID-19 patients with chronic obstructive pulmonary disease (2.59 (1.67, 4.02)), chronic heart failure (1.79 (1.31, 2.45)), immunocompromised (1.77 (1.16, 2.70)), with glycated haemoglobin >8% (1.68 (1.19, 2.38)), depression (1.60 (1.24, 2.06)), hypertension (1.5 (1.21, 1.87)) and physical inactivity (1.25 (1.03, 1.51)) had higher odds of hospitalisation.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Black and Hispanic KPGA patients were at higher odds of hospitalisation, but not mortality, compared with other race groups. Beyond previously reported sociodemographics and comorbidities, factors such as quality of care, lifestyle behaviours and SDOH indicators should be considered when designing and implementing interventions to reduce COVID-19 racial disparities.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjopen-2020-044052"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-4185-7193",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lobelo",
"given": "Felipe",
"sequence": "first"
},
{
"affiliation": [],
"family": "Bienvenida",
"given": "Alan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leung",
"given": "Serena",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mbanya",
"given": "Armand",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leslie",
"given": "Elizabeth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koplan",
"given": "Kate",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shin",
"given": "Sangmin Ryan",
"sequence": "additional"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
5,
19
]
],
"date-time": "2021-05-19T19:00:25Z",
"timestamp": 1621450825000
},
"deposited": {
"date-parts": [
[
2021,
5,
19
]
],
"date-time": "2021-05-19T19:00:57Z",
"timestamp": 1621450857000
},
"indexed": {
"date-parts": [
[
2023,
3,
21
]
],
"date-time": "2023-03-21T19:15:04Z",
"timestamp": 1679426104471
},
"is-referenced-by-count": 6,
"issue": "5",
"issued": {
"date-parts": [
[
2021,
5
]
]
},
"journal-issue": {
"issue": "5",
"published-online": {
"date-parts": [
[
2021,
5,
19
]
]
},
"published-print": {
"date-parts": [
[
2021,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 18,
"start": {
"date-parts": [
[
2021,
5,
19
]
],
"date-time": "2021-05-19T00:00:00Z",
"timestamp": 1621382400000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2020-044052",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e044052",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
5
]
]
},
"published-online": {
"date-parts": [
[
2021,
5,
19
]
]
},
"published-print": {
"date-parts": [
[
2021,
5
]
]
},
"publisher": "BMJ",
"reference": [
{
"key": "2021051910404232000_11.5.e044052.1",
"unstructured": "World Health Organization . Coronavirus disease (COVID-19) situation report November 17, 2020. Available: https://www.who.int/publications/m/item/weekly-epidemiological-update-17-november-2020"
},
{
"DOI": "10.1056/NEJMsa2011686",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.2"
},
{
"DOI": "10.1377/hlthaff.2020.00598",
"article-title": "Disparities in outcomes among COVID-19 patients in a large health care system in California",
"author": "Azar",
"doi-asserted-by": "crossref",
"first-page": "1253",
"journal-title": "Health Aff",
"key": "2021051910404232000_11.5.e044052.3",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.12270",
"article-title": "Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit",
"author": "Suleyman",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "2021051910404232000_11.5.e044052.4",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/j.annepidem.2020.05.003",
"article-title": "Assessing differential impacts of COVID-19 on black communities",
"author": "Millett",
"doi-asserted-by": "crossref",
"first-page": "37",
"journal-title": "Ann Epidemiol",
"key": "2021051910404232000_11.5.e044052.5",
"volume": "47",
"year": "2020"
},
{
"key": "2021051910404232000_11.5.e044052.6",
"unstructured": "Centers for Disease Control and Prevention . National center for immunization and respiratory diseases (NCIRD) DoVD. COVID-19 in racial and ethnic minority groups Atlanta, GA, 2020. Available: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html [Accessed 2 Jul 2020]."
},
{
"DOI": "10.15585/mmwr.mm6918e1",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.7"
},
{
"DOI": "10.15585/mmwr.mm6925e1",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.8"
},
{
"DOI": "10.1101/2020.05.12.20099135",
"doi-asserted-by": "crossref",
"key": "2021051910404232000_11.5.e044052.9",
"unstructured": "Rentsch CT , Kidwai-Khan F , Tate JP . Covid-19 by race and ethnicity: a national cohort study of 6 million United States veterans. medRxiv.doi:10.1101/2020.05.12.20099135"
},
{
"key": "2021051910404232000_11.5.e044052.10",
"unstructured": "United States Census Bureau . Georgia, 2020. Available: https://data.census.gov/cedsci/profile?q=Georgia&g=0400000US13&tid=ACSDP1Y2018.DP05 [Accessed 17 Jun 2020]."
},
{
"key": "2021051910404232000_11.5.e044052.11",
"unstructured": "Georgia Department of Public Health . Georgia department of public health daily status report, 2020. Available: https://dph.georgia.gov/covid-19-daily-status-report [Accessed 20 Nov 2020]."
},
{
"key": "2021051910404232000_11.5.e044052.12",
"unstructured": "Georgia Department of Public Health . Georgia department of public health daily status report, 2020. Available: https://dph.georgia.gov/covid-19-daily-status-report [Accessed 12 May 2020]."
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.052278",
"doi-asserted-by": "crossref",
"key": "2021051910404232000_11.5.e044052.13",
"unstructured": "Rodriguez F , Solomon N , de Lemos JA , et al . Racial and Ethnic Differences in Presentation and Outcomes for Patients Hospitalized with COVID-19: Findings from the American Heart Association’s COVID-19 Cardiovascular Disease Registry. Circulation 2020;382.doi:10.1161/CIRCULATIONAHA.120.052278"
},
{
"article-title": "Racial disparities in COVID-19 hospitalization and in-hospital mortality at the height of the new York City pandemic",
"author": "Renelus",
"first-page": "1",
"journal-title": "J Racial Ethn Health Disparities",
"key": "2021051910404232000_11.5.e044052.14",
"year": "2020"
},
{
"key": "2021051910404232000_11.5.e044052.15",
"unstructured": "Centers for Disease Control and Prevention . National center for immunization and respiratory diseases (NCIRD) DoVD. COVID-19 hospitalization and death by Race/Ethnicity, 2020."
},
{
"key": "2021051910404232000_11.5.e044052.16",
"unstructured": "Metro Atlanta Chamber . Profile of Metro Atlanta, 2020. Available: https://www.metroatlantachamber.com/resources/reports-and-information/executive-profile [Accessed 25 Jun 2020]."
},
{
"key": "2021051910404232000_11.5.e044052.17",
"unstructured": "National Center for Immunization and Respiratory Diseases (NCIRD) Division of Viral Diseases . Standard operating procedure (SOP) for triage of suspected COVID-19 patients in non-US healthcare settings: early identification and prevention of transmission during triage. Centers for Disease Control and Prevention, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/sop-triage-prevent-transmission.html"
},
{
"key": "2021051910404232000_11.5.e044052.18",
"unstructured": "Georgia Department of Public Health . COVID-19: guidance for healthcare professionals 2020. Available: https://dph.georgia.gov/covid-19-guidance-healthcare-professionals [Accessed 18 Jun 2020]."
},
{
"DOI": "10.1080/17445647.2020.1750066",
"article-title": "Geospatial analysis of neighborhood deprivation index (NDI) for the United States by County",
"author": "Andrews",
"doi-asserted-by": "crossref",
"first-page": "101",
"journal-title": "J Maps",
"key": "2021051910404232000_11.5.e044052.19",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1007/s11524-006-9094-x",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.20"
},
{
"key": "2021051910404232000_11.5.e044052.21",
"unstructured": "ArcGIS . Esri Demographics - Tapestry Segmentation: ArcGIS, 2019. Available: https://doc.arcgis.com/en/esri-demographics/data/tapestry-segmentation.htm [Accessed 20 Jun 2022]."
},
{
"key": "2021051910404232000_11.5.e044052.22",
"unstructured": "Office of the Assistant Secretary for Planning and Evaluation . U.S. Federal Poverty Guidelines Used to Determine Financial Eligibility for Certain Federal Programs: U.S Department of Health & Human Services, 2020. Available: https://aspe.hhs.gov/poverty-guidelines2020"
},
{
"key": "2021051910404232000_11.5.e044052.23",
"unstructured": "World Health Organization . The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research, 1993."
},
{
"DOI": "10.1016/0895-4356(92)90133-8",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.24"
},
{
"key": "2021051910404232000_11.5.e044052.25",
"unstructured": "National Committee for Quality Assurance (NCQA) . HEDIS measures and technical resources, 2020. Available: https://www.ncqa.org/hedis/measures/2020"
},
{
"DOI": "10.1249/MSS.0b013e3182630ec1",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.26"
},
{
"DOI": "10.5888/pcd11.140196",
"article-title": "Associations between physical activity and cardiometabolic risk factors assessed in a southern California health care system, 2010-2012",
"author": "Young",
"doi-asserted-by": "crossref",
"journal-title": "Prev Chronic Dis",
"key": "2021051910404232000_11.5.e044052.27",
"volume": "11",
"year": "2014"
},
{
"DOI": "10.1161/CIR.0000000000000559",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.28"
},
{
"DOI": "10.1001/jamanetworkopen.2020.25197",
"article-title": "Characteristics associated with racial/ethnic disparities in COVID-19 outcomes in an academic health care system",
"author": "Gu",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "2021051910404232000_11.5.e044052.29",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1007/s10903-020-01111-5",
"article-title": "Intersectional disparities among Hispanic groups in COVID-19 outcomes",
"author": "Poulson",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "J Immigr Minor Health",
"key": "2021051910404232000_11.5.e044052.30",
"volume": "23",
"year": "2021"
},
{
"key": "2021051910404232000_11.5.e044052.31",
"unstructured": "Hales CM , Carroll MD , Fryar CD . Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS data brief. 360. Hyattsville, MD: National Center for Health Statistics, 2020."
},
{
"key": "2021051910404232000_11.5.e044052.32",
"unstructured": "Centers for Disease Control and Prevention . National diabetes statistics report A. GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services, 2020."
},
{
"DOI": "10.1016/S2214-109X(20)30264-3",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.33"
},
{
"DOI": "10.1177/1932296820930025",
"article-title": "COVID-19: considerations of diabetes and cardiovascular disease management",
"author": "Ceriello",
"doi-asserted-by": "crossref",
"first-page": "723",
"journal-title": "J Diabetes Sci Technol",
"key": "2021051910404232000_11.5.e044052.34",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108229",
"article-title": "Characteristics and outcomes of COVID-19 positive patients with diabetes managed as outpatients",
"author": "Shabto",
"doi-asserted-by": "crossref",
"journal-title": "Diabetes Res Clin Pract",
"key": "2021051910404232000_11.5.e044052.35",
"volume": "164",
"year": "2020"
},
{
"key": "2021051910404232000_11.5.e044052.36",
"unstructured": "Emory University . COVID-19 health equity interactive Dashboard, 2020. Available: https://covid19.emory.edu/ [Accessed 23 Jun 2020]."
},
{
"key": "2021051910404232000_11.5.e044052.37",
"unstructured": "County Health Rankings & Roadmaps . 2020 Georgia report, 2020. Available: https://www.countyhealthrankings.org/reports/state-reports/2020-georgia-report [Accessed 23 Jun 2020]."
},
{
"article-title": "The scientific foundation for the physical activity guidelines for Americans, 2nd edition",
"author": "Powell",
"first-page": "1",
"journal-title": "J Phys Act Health",
"key": "2021051910404232000_11.5.e044052.38",
"year": "2018"
},
{
"DOI": "10.1371/journal.pone.0078350",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.39"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"doi-asserted-by": "publisher",
"key": "2021051910404232000_11.5.e044052.40"
},
{
"DOI": "10.3390/ijerph17082655",
"doi-asserted-by": "crossref",
"key": "2021051910404232000_11.5.e044052.41",
"unstructured": "Song Y , Ren F , Sun D , et al . Benefits of exercise on influenza or pneumonia in older adults: a systematic review. Int J Environ Res Public Health 2020;17:2655. doi:10.3390/ijerph17082655"
},
{
"key": "2021051910404232000_11.5.e044052.42",
"unstructured": "Sallis J , Pratt M . A call to action: physical activity and COVID-19 exercise is medicine, 2020. Available: https://www.exerciseismedicine.org/support_page.php/stories/?b=896 [Accessed 23 Jun 2020]."
},
{
"key": "2021051910404232000_11.5.e044052.43",
"unstructured": "Bryan A D-GJ , Davis NJ , Chokshi DA . Moving from the five whys to five Hows: addressing racial inequities in COVID-19 infection and death. Health Aff 2020.doi:10.1377/hblog20200625.389260"
},
{
"key": "2021051910404232000_11.5.e044052.44",
"unstructured": "Parodi SCB , Young S , Bellows J . Kaiser Permanente’s system capabilities to suppress Covid-19. NEJM Catal."
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2020-044052"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Clinical, behavioural and social factors associated with racial disparities in COVID-19 patients from an integrated healthcare system in Georgia: a retrospective cohort study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "11"
}
