Frail Older Adults with Presymptomatic SARS-CoV-2 Infection: Clinical Course and Prognosis
et al., Gerontology, doi:10.1159/000521412, Jan 2022
Retrospective 849 COVID-19+ patients in skilled nursing homes, showing lower risk of combined hospitalization/death with aspirin prophylaxis, not reaching statistical significance.
Study covers aspirin and vitamin D.
|
risk of death/hospitalization, 26.0% lower, HR 0.74, p = 0.13, treatment 29 of 159 (18.2%), control 178 of 690 (25.8%), NNT 13, adjusted per study, multivariable, Cox proportional hazards, day 40.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Levy et al., 31 Jan 2022, retrospective, Israel, peer-reviewed, 10 authors.
Frail Older Adults with Presymptomatic SARS-CoV-2 Infection: Clinical Course and Prognosis
Gerontology, doi:10.1159/000521412
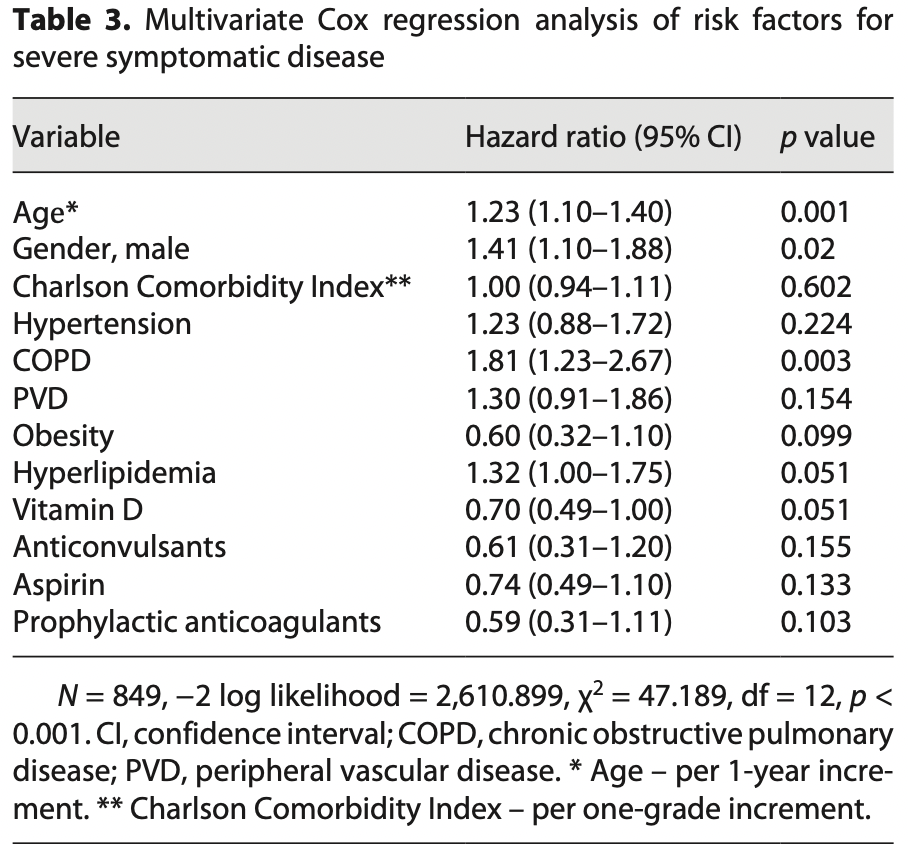
Background/Aims: The novel coronavirus SARS-CoV-2 has caused a pandemic threatening millions of people worldwide. This study aimed to describe clinical characteristics, outcomes, and risk factors of SARS-CoV-2-positive, asymptomatic, frail older adults. Methods: A retrospective cohort study was conducted in 6 designated COVID-19 units, in skilled nursing homes. Subjects were severely frail older adults, positive for SARS-CoV-2, and asymptomatic at the time of their admission in these units. Residents' characteristics and symptoms were obtained via electronic medical records. The primary outcome was a composite of death or hospitalization by day 40. We looked at time to the primary outcome and used Cox regression for a multivariate analysis. Results: During March-November 2020, 849 residents met inclusion criteria. Median age was 84 years. Most were completely dependent for basic activities of daily living and showed cognitive impairment. Six hundred forty-one (75.5%) residents were discharged after considered cured from CO-VID-19, 125 (14.7%) were hospitalized, and 82 (9.7%) died in the facilities. In survival analysis, 35% reached the primary outcome of death or hospitalization by day 40. Age (hazard ratio [HR] 1.23; 95% confidence interval [CI] 1.1-1.4), male gender (HR 1.41; 95% CI: 1.1-1.88), and COPD (HR 1.8; 95% CI: 1.23-2.67) were significant risk factors. Conclusions: In this large cohort, we report care and prognosis of asymptomatic older adults with major functional or cognitive impairments during the COVID-19 pandemic. Most presymptomatic patients do not develop severe infection, and age stays a predominant risk factor, even in the frailest older adults.
Conflict of Interest Statement The authors have no conflicts, financial or others, to disclose.
Author Contributions Y.L. initiated the study, contributed to data collection, analysis, and interpretation, and drafted the manuscript. A.T. contributed to data analysis and interpretation. L.C. provided critical revisions. N.K. contributed to data acquisition. N.T. contributed to data acquisition. T.S. contributed to data acquisition. A.H. provided critical revisions. A.W. provided critical revisions. Y.B. provided critical revisions. Y.L.W. contributed to data analysis and interpretation and drafted the manuscript.
References
Adamo, Yoshikawa, Ouslander, Coronavirus disease 2019 in geriatrics and long-term care: the ABCDs of COVID-19, J Am Geriatr Soc
Anker, Landmesser, Haehling, Butler, Coats et al., Weight loss, malnutrition, and cachexia in COVID-19: facts and numbers, J Cachexia Sarcopenia Muscle
Annweiler, Corvaisier, Gautier, Dubée, Legrand et al., Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID Quasi-Experimental Study, Nutrients
Arons, Hatfield, Reddy, Kimball, James et al., Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility, N Engl J Med
Blazer, Social isolation and loneliness in older adults: a mental health/public health challenge, JAMA Psychiatry
Buitrago-Garcia, Egli-Gany, Counotte, Hossmann, Imeri et al., Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: a living systematic review and meta-analysis, PLoS Med
Cereda, Bogliolo, Lobascio, Barichella, Zecchinelli et al., Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy, Nutrition
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis
Dorjee, Kim, Bonomo, Dolma, Prevalence and predictors of death and severe disease in patients hospitalized due to CO-VID-19: a comprehensive systematic review and meta-analysis of 77 studies and 38,000 patients, PLoS One
Filippo, Lorenzo, 'amico, Sofia, Roveri et al., COVID-19 is associated with clinically significant weight loss and risk of malnutrition, independent of hospitalisation: a post-hoc analysis of a prospective cohort study, Clin Nutr
Grabowski, Mor, Nursing home care in crisis in the wake of COVID-19, JAMA
Graham, Junghans, Downes, Sendall, Lai et al., SARS-CoV-2 infection, clinical features and outcome of COVID-19 in United Kingdom nursing homes, J Infect
Hashan, Smoll, King, Ockenden-Muldoon, Walker et al., Epidemiology and clinical features of COVID-19 outbreaks in aged care facilities: a systematic review and meta-analysis, EClinicalMedicine
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Hewitt, Carter, Vilches-Moraga, Quinn, Braude et al., The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study, Lancet Public Health
Horby, Lim, Emberson, Mafham, Bell, Dexamethasone in hospitalized patients with Covid-19, N Engl J Med
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat Rev Microbiol
Katz, Ford, Moskowitz, Jackson, Jaffe, Studies of illness in the aged. the index of ADL: a standardized measure of biological and psychosocial function, JAMA
Kennelly, Dyer, Noonan, Martin, Kennelly et al., Asymptomatic carriage rates and case fatality of SARS-CoV-2 infection in residents and staff in Irish nursing homes, Age Ageing
Ma, Zhou, Heianza, Qi, Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank, Am J Clin Nutr
Manca, Marco, Venneri, The impact of COVID-19 infection and enforced prolonged social isolation on neuropsychiatric symptoms in older adults with and without dementia: a review, Front Psychiatry
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with CO-VID-19 test results, JAMA Netw Open
Oreopoulos, Kalantar-Zadeh, Sharma, Fonarow, The obesity paradox in the elderly: potential mechanisms and clinical implications, Clin Geriatr Med
Ouslander, Grabowski, COVID-19 in nursing homes: calming the perfect storm, J Am Geriatr Soc
Panagiotou, Kosar, White, Bantis, Yang et al., Risk factors associated with all-cause 30-day mortality in nursing home residents with COVID-19, JAMA Intern Med
Rockwood, Song, Macknight, Bergman, Hogan et al., A global clinical measure of fitness and frailty in elderly people, Can Med Assoc J
Rubin, Sorting out whether vitamin D deficiency raises COVID-19 risk, JAMA
Sah, Fitzpatrick, Zimmer, Abdollahi, Juden-Kelly et al., Asymptomatic SARS-CoV-2 infection: a systematic review and meta-analysis, Proc Natl Acad Sci
Sakurai, Sasaki, Kato, Hayashi, Tsuzuki et al., Natural history of asymptomatic SARS-CoV-2 infection, N Engl J Med
Shahid, Kalayanamitra, Mcclafferty, Kepko, Ramgobin et al., CO-VID-19 and older adults: what we know, J Am Geriatr Soc
Shi, Bakaev, Chen, Travison, Berry, Risk factors, presentation, and course of coronavirus disease 2019 in a large, academic long-term care facility, J Am Med Dir Assoc
Tehrani, Killander, Åstrand, Jakobsson, Gille-Johnson, Risk factors for death in adult COVID-19 patients: frailty predicts fatal outcome in older patients, Int J Infect Dis
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for disease control and prevention, JAMA
Zheng, Peng, Xu, Zhao, Liu et al., Risk factors of critical & mortal CO-VID-19 cases: a systematic literature review and meta-analysis, J Infect
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.1159/000521412",
"ISSN": [
"0304-324X",
"1423-0003"
],
"URL": "http://dx.doi.org/10.1159/000521412",
"abstract": "<jats:p>Background/Aims: The novel coronavirus SARS-CoV-2 has caused a pandemic threatening millions of people worldwide. This study aimed to describe clinical characteristics, outcomes, and risk factors of SARS-CoV-2-positive, asymptomatic, frail older adults. Methods: A retrospective cohort study was conducted in 6 designated COVID-19 units, in skilled nursing homes. Subjects were severely frail older adults, positive for SARS-CoV-2, and asymptomatic at the time of their admission in these units. Residents’ characteristics and symptoms were obtained via electronic medical records. The primary outcome was a composite of death or hospitalization by day 40. We looked at time to the primary outcome and used Cox regression for a multivariate analysis. Results: During March–November 2020, 849 residents met inclusion criteria. Median age was 84 years. Most were completely dependent for basic activities of daily living and showed cognitive impairment. Six hundred forty-one (75.5%) residents were discharged after considered cured from COVID-19, 125 (14.7%) were hospitalized, and 82 (9.7%) died in the facilities. In survival analysis, 35% reached the primary outcome of death or hospitalization by day 40. Age (hazard ratio [HR] 1.23; 95% confidence interval [CI] 1.1–1.4), male gender (HR 1.41; 95% CI: 1.1–1.88), and COPD (HR 1.8; 95% CI: 1.23–2.67) were significant risk factors. Conclusions: In this large cohort, we report care and prognosis of asymptomatic older adults with major functional or cognitive impairments during the COVID-19 pandemic. Most presymptomatic patients do not develop severe infection, and age stays a predominant risk factor, even in the frailest older adults. </jats:p>",
"archive": [
"Portico"
],
"author": [
{
"affiliation": [],
"family": "Levy",
"given": "Yochai",
"sequence": "first"
},
{
"affiliation": [],
"family": "Turjeman",
"given": "Adi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cooper",
"given": "Lisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kagansky",
"given": "Nadya",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0247-6737",
"affiliation": [],
"authenticated-orcid": false,
"family": "Nagulevich",
"given": "Tatiana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Snir",
"given": "Tamari",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hershkovitz",
"given": "Avital",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Weiss",
"given": "Avraham",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Beloosesky",
"given": "Yichayaou",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1898-6173",
"affiliation": [],
"authenticated-orcid": false,
"family": "Leibovici Weissman",
"given": "Yaara",
"sequence": "additional"
}
],
"container-title": [
"Gerontology"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
1,
31
]
],
"date-time": "2022-01-31T22:00:36Z",
"timestamp": 1643666436000
},
"deposited": {
"date-parts": [
[
2022,
2,
8
]
],
"date-time": "2022-02-08T10:01:11Z",
"timestamp": 1644314471000
},
"indexed": {
"date-parts": [
[
2022,
2,
8
]
],
"date-time": "2022-02-08T10:43:17Z",
"timestamp": 1644316997392
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0304-324X"
},
{
"type": "electronic",
"value": "1423-0003"
}
],
"issued": {
"date-parts": [
[
2022,
1,
31
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.karger.com/Services/SiteLicenses",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
31
]
],
"date-time": "2022-01-31T00:00:00Z",
"timestamp": 1643587200000
}
},
{
"URL": "https://www.karger.com/Services/SiteLicenses",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
31
]
],
"date-time": "2022-01-31T00:00:00Z",
"timestamp": 1643587200000
}
}
],
"link": [
{
"URL": "https://www.karger.com/Article/Pdf/521412",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.karger.com/Article/Pdf/521412",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "127",
"original-title": [],
"page": "1-9",
"prefix": "10.1159",
"published": {
"date-parts": [
[
2022,
1,
31
]
]
},
"published-online": {
"date-parts": [
[
2022,
1,
31
]
]
},
"publisher": "S. Karger AG",
"reference": [
{
"DOI": "10.1038/s41579-020-00459-7",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1016/j.ijid.2020.10.071",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1001/jama.2020.8524",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1111/jgs.16784",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1001/jama.2020.2648",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1001/jama.1963.03060120024016",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1371/journal.pone.0243191",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1001/jama.2020.24127",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1002/jcsm.12674",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1016/j.cger.2009.07.005",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1001/jamapsychiatry.2020.1054",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.3389/fpsyt.2020.585540",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1016/j.jamda.2020.08.027",
"doi-asserted-by": "publisher",
"key": "ref15"
}
],
"reference-count": 15,
"references-count": 15,
"relation": {},
"score": 1,
"short-container-title": [
"Gerontology"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Geriatrics and Gerontology",
"Aging"
],
"subtitle": [],
"title": [
"Frail Older Adults with Presymptomatic SARS-CoV-2 Infection: Clinical Course and Prognosis"
],
"type": "journal-article"
}
levy