Association Between Inhaled Corticosteroid Use and the Severe Acute Respiratory Syndrome Coronavirus 2 Infection: A Nationwide Population-based Study in South Korea
et al., Research Square, doi:10.21203/rs.3.rs-72221/v1, Sep 2021
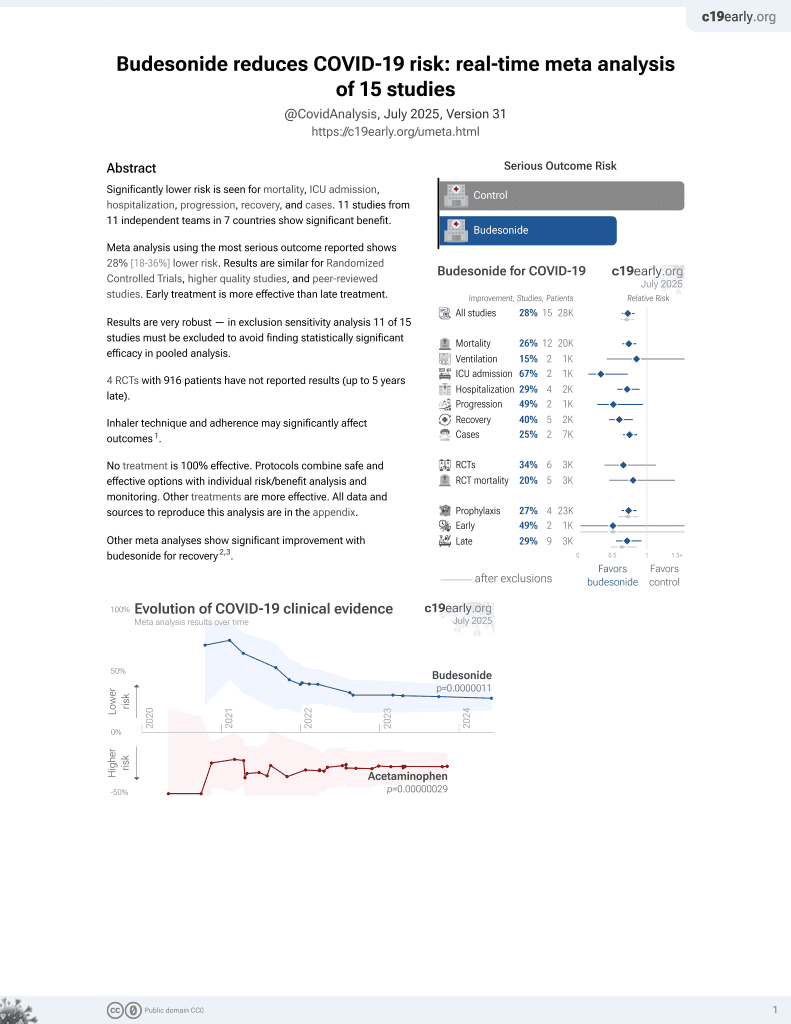
Budesonide for COVID-19
27th treatment shown to reduce risk in
September 2021, now with p = 0.0000042 from 14 studies, recognized in 10 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 44,968 patients in South Korea, 7,019 on inhaled corticosteroids, showing no statistically significant differences in COVID-19 cases.
Targeted administration to the respiratory tract provides treatment directly
to the typical source of initial SARS-CoV-2 infection and replication, and
allows for rapid onset of action, higher local drug concentration, and reduced systemic side effects.
|
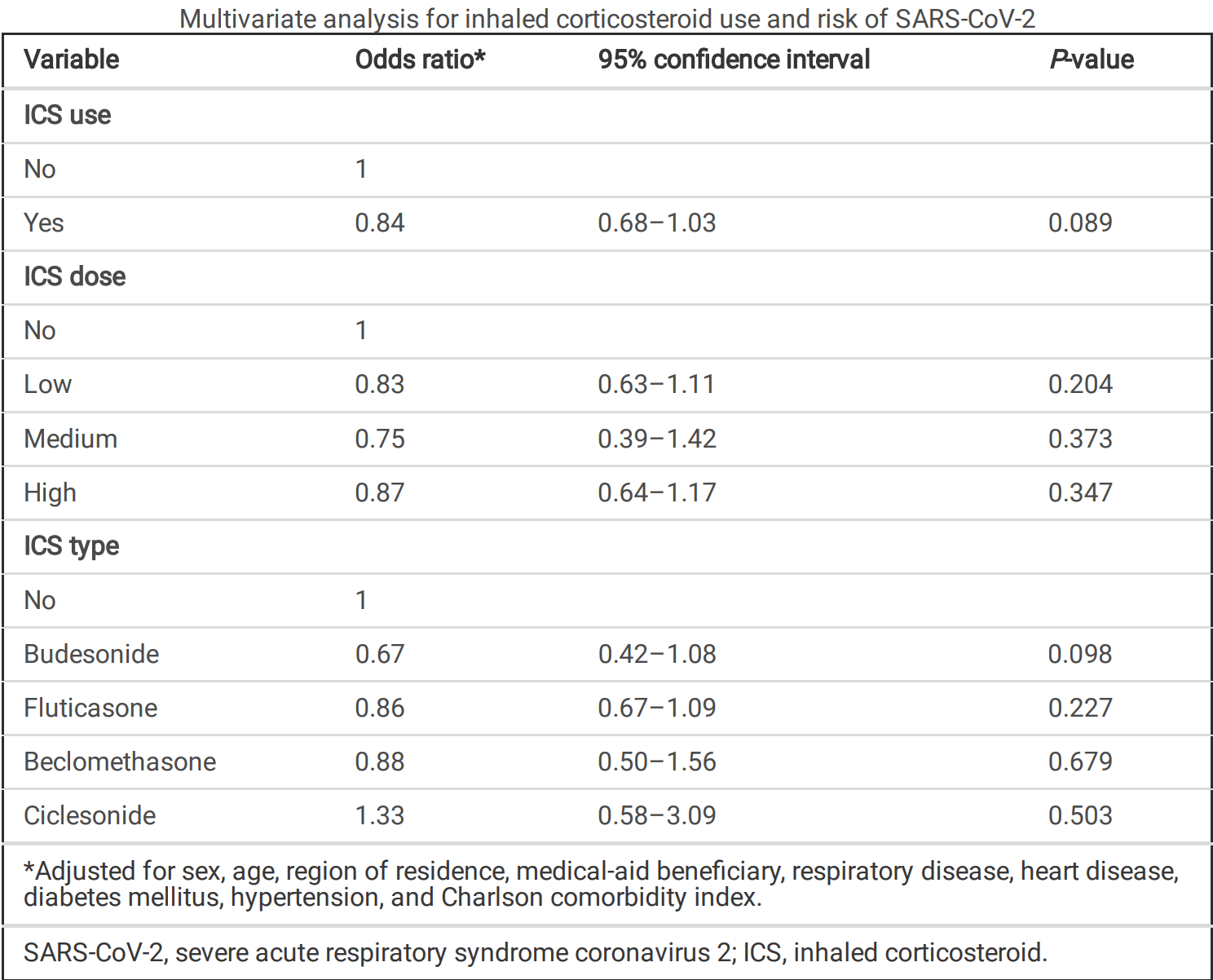
risk of case, 32.6% lower, RR 0.67, p = 0.10, treatment 19 of 1,674 (1.1%), control 95 of 5,345 (1.8%), NNT 156, adjusted per study, odds ratio converted to relative risk, multivariate.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Lee et al., 9 Sep 2021, retrospective, South Korea, preprint, 5 authors.
Association Between Inhaled Corticosteroid Use and the Severe Acute Respiratory Syndrome Coronavirus 2 Infection: A Nationwide Population-based Study in South Korea
doi:10.21203/rs.3.rs-72221/v1
Background Inhaled corticosteroid (ICS) use may increase the risk of respiratory infection, but its in uence on the risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is not known. This study aimed to investigate the association between ICS use and the risk of SARS-CoV-2 infection among the patients with chronic respiratory diseases.
Methods The Ministry of Health and Welfare and Health Insurance Review and Assessment Service in Korea provided nationwide data of 44,968 individuals with chronic respiratory diseases tested for SARS-CoV-2 until May 15. The risks of SARS-CoV-2 infection were retrospectively analysed according to the prescription, type, and dose of ICS taken one year before SARS-CoV-2 test.
Results Among 44,968 individuals tested, 931 (2.1%) were positive for SARS-CoV-2. A total of 7,019 patients (15.6%) were prescribed ICS one year prior to being tested for SARS-CoV-2. Low, medium, and high doses of ICS were prescribed in 7.5%, 1.6%, and 6.5% of total cases, respectively. Among the types of ICS, budesonide, uticasone, beclomethasone, and ciclesonide were prescribed in 3.7%, 8.9%, 2.3%, and 0.6% of total cases, respectively. The multivariate analysis showed no signi cant increase in infection with ICS use (OR, 0.84; 95% CI, 0.66-1.03). Moreover, there were no associations between the risk of infection, and doses or types of ICS prescribed.
Conclusion Prior ICS use did not increase the risk of SARS-CoV-2 infection. Moreover, different doses or types of ICS did not affect the risk. This study supports the current guidelines to manage patients taking ICS during the SARS-CoV-2 pandemic.
Declarations Ethics approval and consent to participate: This study was approved by the Institutional Review Board of the National Health Insurance Service of the Ilsan Hospital and adhered to the tenets of the Declaration of Helsinki (NHIMC 2020-04-008). Written informed consent was waived as the data were de-identi ed in the database used.
Consent for publication:
Not
Con icts of interest: The authors declare that they have no relevant con icts of interest.
Author's contributions: Supplementary Files This is a list of supplementary les associated with this preprint. Click to download.
COVID19andICSRespiratoryResearchSuppl.docx
References
Andréjak, Nielsen, Thomsen, Duhaut, Sørensen et al., Chronic respiratory disease, inhaled corticosteroids and risk of non-tuberculous mycobacteriosis, Thorax
Brode, Campitelli, Kwong, Lu, Marchand-Austin et al., The risk of mycobacterial infections associated with inhaled corticosteroid use, Eur Respir J
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet
Gif, Global strategy for asthma management and prevention
Guan, Ni, Hu, Liang, Ou et al., Clinical Characteristics of Coronavirus Disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032
Halpin, Faner, Sibila, Badia, Agusti, Do chronic respiratory diseases or their treatment affect the risk of SARS-CoV-2 infection?, Lancet Respir Med
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell
Iwabuchi, Kurakami, Takahashi, Kato, Morishima, Therapeutic potential of ciclesonide inahalation for COVID-19 pneumonia: Report of three cases, J Infect Chemother
Janson, Stratelis, Miller-Larsson, Harrison, Larsson, Scienti c rationale for the possible inhaled corticosteroid intraclass difference in the risk of pneumonia in COPD, Int J Chron Obstruct Pulmon Dis
Kew, Seniukovich, Inhaled steroids and risk of pneumonia for chronic obstructive pulmonary disease, Cochrane Database Syst Rev, doi:10.1002/14651858.CD010115.pub2
Kim, Rhee, Shim, Park, Yoo et al., Inhaled Corticosteroids in Asthma and the Risk of Pneumonia, Allergy Asthma Immunol Res
Lee, Kim, Hyun, Jang, Lee et al., Use of inhaled corticosteroids and the risk of tuberculosis, Thorax
Matsuyama, Kawase, Nao, Shirato, Ujike et al., The inhaled corticosteroid ciclesonide blocks coronavirus RNA replication by targeting viral NSP15, bioRxiv, doi:10.1101/2020.03.11.987016.2020
Mckeever, Harrison, Hubbard, Shaw, Inhaled corticosteroids and the risk of pneumonia in people with asthma: a case-control study, Chest
O'byrne, Pedersen, Carlsson, Radner, Thorén et al., Risks of pneumonia in patients with asthma taking inhaled corticosteroids, Am J Respir Crit Care Med
Organization, Coronavirus disease (COVID-2019) situation reports
Peters, Sajuthi, Deford, Christenson, Rios et al., COVID-19 Related Genes in Sputum Cells in Asthma: Relationship to Demographic Features and Corticosteroids, Am J Respir Crit Care Med, doi:10.1164/rccm.202003-0821OC
Singanayagam, Glanville, Girkin, Ching, Marcellini et al., Corticosteroid suppression of antiviral immunity increases bacterial loads and mucus production in COPD exacerbations, Nat Commun
Suissa, Mcghan, Niewoehner, Make, Inhaled corticosteroids in chronic obstructive pulmonary disease, Proc Am Thorac Soc
Yamaya, Nishimura, Deng, Sugawara, Watanabe et al., Inhibitory effects of glycopyrronium, formoterol, and budesonide on coronavirus HCoV-229E replication and cytokine production by primary cultures of human nasal and tracheal epithelial cells, Respir Investig
Yan, Zhang, Li, Xia, Guo et al., Structural basis for the recognition of SARS-CoV-2 by fulllength human ACE2, Science
Yang, Chen, Zhang, Du, Xu et al., Long-term of inhaled corticosteroids and risk of upper respiratory tract infection in chronic obstructive pulmonary disease: a meta-analysis, Inhal Toxicol
Yang, Zhang, Chen, Lin, Zeng et al., Inhaled corticosteroids and risk of upper respiratory tract infection in patients with asthma: a meta-analysis, Infection
Yang, Zheng, Gou, Pu, Chen et al., Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: A systematic review and meta-analysis, Int J Infect Dis
Zhu, Zhang, Li, Yang, Song, GINA-GLOBAL Initiative for Asthma HIRA-Health Insurance Review and Assessment Service ICS-Inhaled corticosteroid OR-Odds ratio SARS-CoV-2-Severe acute respiratory syndrome coronavirus 2 TMPRSS2-Transmembrane protease serine 2 URTI-Upper respiratory tract infection References, N Engl J Med
DOI record:
{
"DOI": "10.21203/rs.3.rs-72221/v1",
"URL": "http://dx.doi.org/10.21203/rs.3.rs-72221/v1",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>Background\n\nInhaled corticosteroid (ICS) use may increase the risk of respiratory infection, but its influence on the risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is not known. This study aimed to investigate the association between ICS use and the risk of SARS-CoV-2 infection among the patients with chronic respiratory diseases.\nMethods\n\nThe Ministry of Health and Welfare and Health Insurance Review and Assessment Service in Korea provided nationwide data of 44,968 individuals with chronic respiratory diseases tested for SARS-CoV-2 until May 15. The risks of SARS-CoV-2 infection were retrospectively analysed according to the prescription, type, and dose of ICS taken one year before SARS-CoV-2 test.\nResults\n\nAmong 44,968 individuals tested, 931 (2.1%) were positive for SARS-CoV-2. A total of 7,019 patients (15.6%) were prescribed ICS one year prior to being tested for SARS-CoV-2. Low, medium, and high doses of ICS were prescribed in 7.5%, 1.6%, and 6.5% of total cases, respectively. Among the types of ICS, budesonide, fluticasone, beclomethasone, and ciclesonide were prescribed in 3.7%, 8.9%, 2.3%, and 0.6% of total cases, respectively. The multivariate analysis showed no significant increase in infection with ICS use (OR, 0.84; 95% CI, 0.66–1.03). Moreover, there were no associations between the risk of infection, and doses or types of ICS prescribed.\nConclusion\n\nPrior ICS use did not increase the risk of SARS-CoV-2 infection. Moreover, different doses or types of ICS did not affect the risk. This study supports the current guidelines to manage patients taking ICS during the SARS-CoV-2 pandemic.</jats:p>",
"accepted": {
"date-parts": [
[
2020,
9,
4
]
]
},
"author": [
{
"affiliation": [
{
"name": "National Health Insurance Service Ilsan Hospital"
}
],
"family": "Lee",
"given": "Sang Chul",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Health Insurance Service Ilsan Hospital"
}
],
"family": "Son",
"given": "Kang Ju",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Health Insurance Service Ilsan Hospital"
}
],
"family": "Han",
"given": "Chang Hoon",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1589-4142",
"affiliation": [
{
"name": "Yonsei University College of Medicine"
}
],
"authenticated-orcid": false,
"family": "Jung",
"given": "Ji Ye",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Health Insurance Service Ilsan Hospital"
}
],
"family": "Park",
"given": "Seon Cheol",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
9,
9
]
],
"date-time": "2020-09-09T16:55:28Z",
"timestamp": 1599670528000
},
"deposited": {
"date-parts": [
[
2021,
3,
17
]
],
"date-time": "2021-03-17T18:45:48Z",
"timestamp": 1616006748000
},
"group-title": "In Review",
"indexed": {
"date-parts": [
[
2022,
4,
4
]
],
"date-time": "2022-04-04T12:53:35Z",
"timestamp": 1649076815932
},
"institution": [
{
"name": "Research Square"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2020,
9,
9
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
9,
9
]
],
"date-time": "2020-09-09T00:00:00Z",
"timestamp": 1599609600000
}
}
],
"link": [
{
"URL": "https://www.researchsquare.com/article/rs-72221/v1",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.researchsquare.com/article/rs-72221/v1.html",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "8761",
"original-title": [],
"posted": {
"date-parts": [
[
2020,
9,
9
]
]
},
"prefix": "10.21203",
"published": {
"date-parts": [
[
2020,
9,
9
]
]
},
"publisher": "Research Square Platform LLC",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.researchsquare.com/article/rs-72221/v1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Association Between Inhaled Corticosteroid Use and the Severe Acute Respiratory Syndrome Coronavirus 2 Infection: A Nationwide Population-based Study in South Korea",
"type": "posted-content"
}