Association of Endothelial Nitric Oxide Synthase Polymorphisms with Clinical Severity in Patients with COVID-19
et al., Journal of Clinical Medicine, doi:10.3390/jcm14061931, Mar 2025
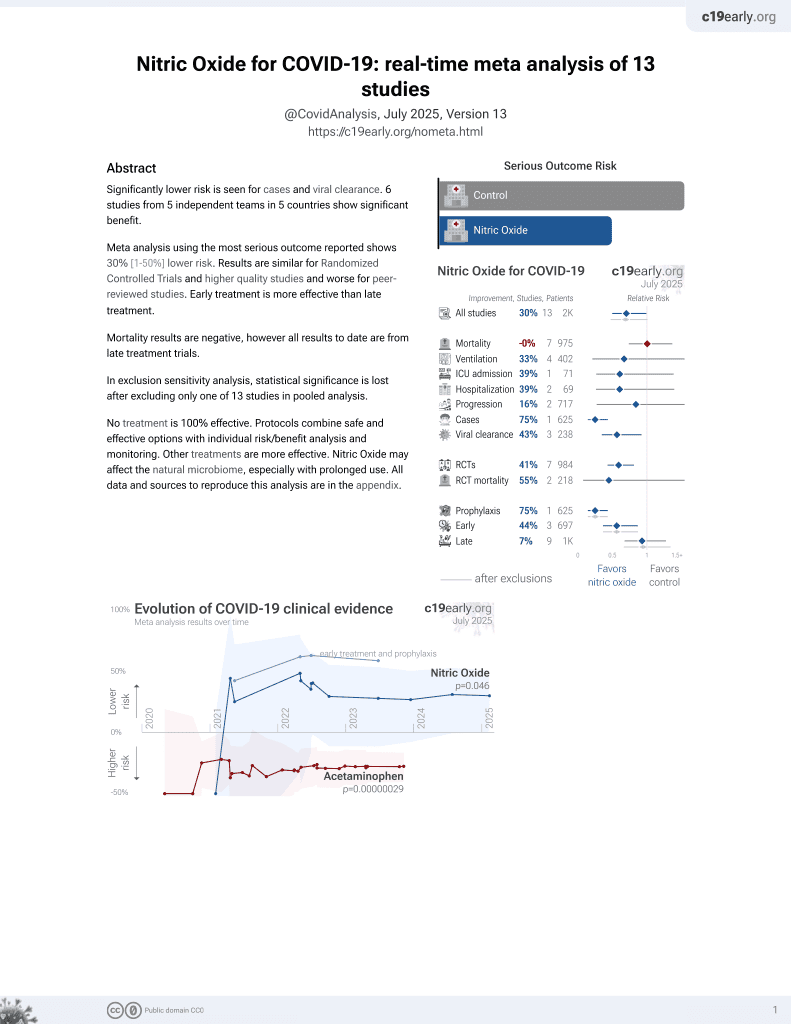
43rd treatment shown to reduce risk in
June 2022, now with p = 0.012 from 12 studies, recognized in 10 countries.
Lower risk for cases and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
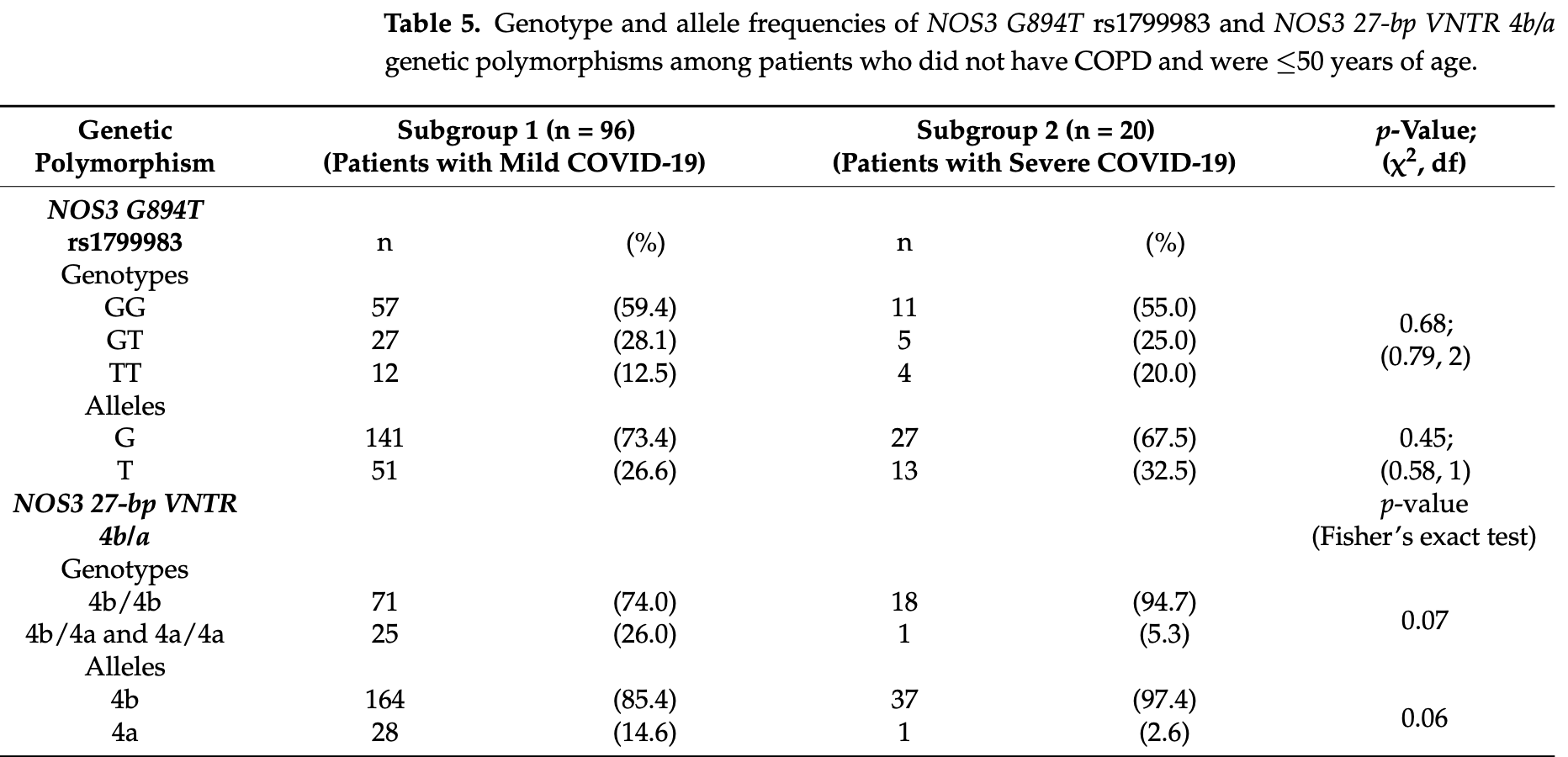
Retrospective 178 COVID-19 patients examining the association between NOS3 genetic polymorphisms (G894T and 27-bp VNTR 4b/a) and disease severity. Overall, no statistically significant associations were found between NOS3 genotypes and COVID-19 severity. However, subgroup analysis of younger patients (≤50 years) without COPD showed a trend toward higher frequency of the 4b allele (97.4% vs. 85.4%, p=0.06) and 4b/4b genotype (94.7% vs. 74.0%, p=0.05) in patients with severe disease. The 4b allele and 4b/4b genotype of the NOS3 27-bp VNTR polymorphism may relate to lower nitric oxide levels, via decreased NOS3 activity and reduced NO synthesis. Nitric oxide treatment for COVID-19 may be more benefiical in patients where polymorphisms reduce nitric oxide production.
İdikut et al., 13 Mar 2025, retrospective, USA, peer-reviewed, 8 authors, study period December 2021 - September 2022.
Contact: aytekinidikut@gmail.com (corresponding author), sevincsarinc@hacettepe.edu.tr, deniz.koksal@hacettepe.edu.tr, lter.deger@mku.edu.tr, babaoglu@hacettepe.edu.tr, skarahan@hacettepe.edu.tr.
Association of Endothelial Nitric Oxide Synthase Polymorphisms with Clinical Severity in Patients with COVID-19
Journal of Clinical Medicine, doi:10.3390/jcm14061931
Background/Objectives: To elucidate the factors that contribute to individual variability in the progression of COVID-19, experiments on endothelial nitric oxide synthase polymorphisms have been reported. Nitric oxide synthase (NOS3) is located in the endothelium and is involved in the regulation of inflammation and vascular homeostasis. In this study, we investigated the association between COVID-19 severity and NOS3 G894T and NOS3 27-bp VNTR 4b/a genetic polymorphisms. Methods: Patients with COVID-19 (n = 178) were divided into Group 1 (mild disease) and Group 2 (severe disease) based on oxygen saturation levels in room air (Group 1, SpO 2 ≥ 93%, n = 107; and Group 2, SpO 2 < 93%, n = 73) and hospitalization requirements. Genotyping was performed using polymerase chain reaction-restriction fragment length polymorphism analysis. Results: Overall, genotype and allele frequencies of the NOS3 genetic polymorphisms were similar across the two study groups (p > 0.05). However, the subgroup analysis showed a notable trend for the 4b/4a allele distribution between Groups 1 and 2. In the younger subgroup of patients (≤50 years old) without chronic obstructive pulmonary disease, Group 2 tended to have a higher frequency of the 4b allele than Group 1 (97.4% vs. 85.4% p = 0.06) and a higher occurrence of 4b/4b genotype (94.7% vs. 74.0%, p = 0.05). Additionally, a rarely observed 4c allele was detected only in two subjects within Group 2 but not in Group 1. Conclusions: These findings suggest a trend of association between COVID-19 severity and NOS3 27-bp VNTR 4b/a genetic polymorphism. Genetic analysis may reveal patient susceptibility to disease, prognosis risk factors, and drug responsiveness.
Funding: This research received no external funding. Institutional Review Board Statement: All procedures performed in this study involving human participants were in accordance with the ethical standards of the Helsinki Declaration, and the study was approved by the Hacettepe University Ethics Committee (Protocol Number: KA-21132, approved on 9 November 2021). Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare no conflicts of interest.
Abbreviations The
References
Akerström, Mousavi-Jazi, Klingström, Leijon, Lundkvist et al., Nitric oxide inhibits the replication cycle of severe acute respiratory syndrome coronavirus, J. Virol, doi:10.1128/JVI.79.3.1966-1969.2005
Alshaikh, Godman, Sindi, Seaton, Kurdi, Prevalence of bacterial coinfection and patterns of antibiotics prescribing in patients with COVID-19: A systematic review and meta-analysis, PLoS ONE
Anastassopoulou, Gkizarioti, Patrinos, Tsakris, Human genetic factors associated with susceptibility to SARS-CoV-2 infection and COVID-19 disease severity, Hum. Genom, doi:10.1186/s40246-020-00290-4
Babaoglu, Dikmenoglu, Ileri-Gurel, Seringec, Zoto et al., Functional effects of endothelial nitric oxide synthase genetic polymorphisms on haemorheological parameters in healthy human individuals, Basic Clin. Pharmacol. Toxicol, doi:10.1111/j.1742-7843.2010.00637.x
Berlin, Gulick, Martinez, Severe COVID-19, N. Engl. J. Med, doi:10.1056/NEJMcp2009575
Blanco-Melo, Nilsson-Payant, Liu, Uhl, Hoagland et al., Imbalanced host response to SARS-CoV-2 drives development of COVID-19, Cell, doi:10.1016/j.cell.2020.04.026
Cotta Filho, Oliveira-Paula, ; Rondon, Pereira, Lacchini, Clinically relevant endothelial nitric oxide synthase polymorphisms and their impact on drug response, Expert Opin. Drug Metab. Toxicol, doi:10.1080/17425255.2020.1804857
Delgado-Wicke, Fernández De Córdoba-Oñate, Roy-Vallejo, Alegría-Carrasco, Rodríguez-Serrano et al., Genetic Variants Regulating the Immune Response Improve the Prediction of COVID-19 Severity Provided by Clinical Variables, Sci. Rep, doi:10.1038/s41598-024-71476-2
Demirci, Ünlü, Yi Gin, Zeyrek, Pathogenesis of SARS-CoV-2 and immune response in COVID-19, Turk. Mikrobiyol. Cem. Derg, doi:10.5222/TMCD.2020.183
Dieter, Brondani, Leitão, Gerchman, Lemos et al., Genetic Polymorphisms Associated with Susceptibility to COVID-19 Disease and Severity: A Systematic Review and Meta-Analysis, PLoS ONE, doi:10.1371/journal.pone.0270627
Eid, Aleksandrova, Shkurat, Shkurat, The Association of PON1 and NOS3 Genetic Variants with the Severity of COVID-19, Gene Rep, doi:10.1016/j.genrep.2023.101814
Ejaz, Alsrhani, Zafar, Javed, Junaid et al., COVID-19 and comorbidities: Deleterious impact on infected patients, J. Infect. Public Health, doi:10.1016/j.jiph.2020.07.014
Förstermann, Li, Therapeutic effect of enhancing endothelial nitric oxide synthase (NOS3) expression and preventing NOS3 uncoupling, Br. J. Pharmacol, doi:10.1111/j.1476-5381.2010.01196.x
Galanakis, Kofteridis, Stratigi, Petraki, Vazgiourakis et al., Intron 4 a/b polymorphism of the endothelial nitric oxide synthase gene is associated with both type 1 and type 2 diabetes in a genetically homogeneous population, Hum. Immunol, doi:10.1016/j.humimm.2008.03.001
Ghaznavi-Rad, Khosravi, Sayyadi, The importance of using routine laboratory tests in the diagnosis and prognosis of patients with coronavirus disease 2019: Shedding light on clinical laboratory data in COVID-19, J. Clin. Lab. Anal, doi:10.1002/jcla.24713
Godfrey, Chan, Cassidy, Butler, Choy et al., The functional consequence of the Glu298Asp polymorphism of the endothelial nitric oxide synthase gene in young healthy volunteers, Cardiovasc. Drug Rev, doi:10.1111/j.1527-3466.2007.00017.x
Guan, Seet, Kennedy, Does NOS3 derived nitric oxide protect the young from severe COVID-19 complications?, Ageing Res. Rev, doi:10.1016/j.arr.2020.101201
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Ji, Chen, Ze, Zhou, Human genetic basis of severe or critical illness in COVID-19, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2022.963239
Kaltoum, Mutations and polymorphisms in genes involved in the infections by COVID-19: A Review, Gene Rep, doi:10.1016/j.genrep.2021.101062
Khan, Shah, Mushtaq, Jehanzeb, Profiling laboratory biomarkers associated with COVID-19 disease progression: A single-center experience, Int. J. Microbiol, doi:10.1155/2021/6643333
Konar, Ramesh, Christopher, Prasanthi, Bhat et al., The correlation of endothelial nitric oxide synthase (NOS3) polymorphism and other risk factors with aneurysmal subarachnoid hemorrhage: A case-control study, Neurol. India, doi:10.4103/0028-3886.266231
Konradt, Hunter, Pathogen interactions with endothelial cells and the induction of innate and adaptive immunity, Eur. J. Immunol, doi:10.1002/eji.201646789
Li, Sun, Carmeliet, Hallmarks of endothelial cell metabolism in health and disease, Cell Metab, doi:10.1016/j.cmet.2019.08.011
Ma, Chen, Ren, Guo, Guo et al., Association between NOS3 4b/a polymorphism and the risk of diabetic retinopathy in type 2 diabetes mellitus: A meta-analysis, J. Diabetes Res, doi:10.1155/2014/549747
Marín, Rodríguez-Martínez, Role of vascular nitric oxide in physiological and pathological conditions, Pharmacol. Ther, doi:10.1016/S0163-7258(97)00051-X
Moncada, Nitric oxide, J. Hypertens. Suppl
Nägele, Haubner, Tanner, Ruschitzka, Flammer, Endothelial dysfunction in COVID-19: Current findings and therapeutic implications, Atherosclerosis, doi:10.1016/j.atherosclerosis.2020.10.014
Ohno, Dzúrová, Body mass index and risk for COVID-19-related hospitalization in adults aged 50 and older in Europe, Nutrients, doi:10.3390/nu14194001
Oliveira-Paula, Lacchini, Tanus-Santos, Endothelial nitric oxide synthase: From biochemistry and gene structure to clinical implications of NOS3 polymorphisms, Gene, doi:10.1016/j.gene.2015.09.061
Ombrello, Schulert, COVID-19 and cytokine storm syndrome: Are there lessons from macrophage activation syndrome?, Transl. Res, doi:10.1016/j.trsl.2021.03.002
Ozturk, Balat, Pehlivan, Ugur, Ozcan et al., Endothelial nitric oxide synthase gene polymorphisms in preeclampsia with or without eclampsia in a Turkish population, J. Obstet. Gynaecol. Res, doi:10.1111/j.1447-0756.2011.01606.x
Papadopoulos, Sutheesophon, Aw, The influence of renin angiotensin aldosterone system (RAAS), endothelial nitric oxide synthase (NOS3) and erythropoietin (EPO) on COVID-19 complications, Chem. Biol. Interact, doi:10.1016/j.cbi.2022.109834
Ponti, Maccaferri, Ruini, Tomasi, Ozben, Biomarkers associated with COVID-19 disease progression, Crit. Rev. Clin. Lab. Sci, doi:10.1080/10408363.2020.1770685
Purkayastha, Sen, Garcia, Jr, Langerman et al., Direct exposure to SARS-CoV-2 and cigarette smoke increases infection severity and alters the stem cell-derived airway repair response, Cell Stem Cell, doi:10.1016/j.stem.2020.11.010
Rossaint, Gerlach, Schmidt-Ruhnke, Pappert, Lewandowski et al., Efficacy of inhaled nitric oxide in patients with severe ARDS, Chest, doi:10.1378/chest.107.4.1107
Saini, Bhatnagar, Bhattacharjee, Association of endothelial dysfunction with endothelin, nitric oxide and NOS3 Glu298Asp gene polymorphism in coronary artery disease, Dis. Markers, doi:10.1155/2011/419708
Severe, Group; Ellinghaus, Degenhardt, Bujanda, Buti et al., Genomewide association study of severe COVID-19 with respiratory failure, N. Engl. J. Med, doi:10.1056/NEJMoa2020283
Shi, Liu, Guo, Liu, Xu et al., Association between NOS3 rs1799983 polymorphism and hypertension: A meta-analysis involving 14,185 cases and 13,407 controls, BMC Cardiovasc. Disord, doi:10.1186/s12872-021-02192-2
Silva, Neves, Rocha, Sales, Medeiros et al., Endothelial nitric oxide gene haplotype reduces the effect of a single bout of exercise on the vascular reactivity in healthy subjects, Transl. Res, doi:10.1016/j.trsl.2012.05.004
Sljivancanin Jakovljevic, Kontic-Vucinic, Nikolic, Nikolic, Carkic et al., Association between endothelial nitric oxide synthase (NOS3) -786 T/C and 27-bp VNTR 4b/a polymorphisms and preeclampsia development, Reprod. Sci, doi:10.1007/s43032-021-00632-0
Smith, Cuthbertson, Harvie, Webster, Robins et al., Increased bone resorption in the critically ill: Association with sepsis and increased nitric oxide production, Crit. Care Med, doi:10.1097/00003246-200204000-00020
Souza-Costa, Belo, Silva, Sertorio, Metzger et al., NOS3 haplotype associated with hypertension in obese children and adolescents, Int. J. Obes, doi:10.1038/ijo.2010.146
Staalsø, Edsen, Kotinis, Romner, Springborg et al., Association of the NOS3 intron-4 VNTR polymorphism with aneurysmal subarachnoid hemorrhage, J. Neurosurg, doi:10.3171/2014.5.JNS131572
Tanus-Santos, Desai, Deak, Pezzullo, Abernethy et al., Effects of endothelial nitric oxide synthase gene polymorphisms on platelet function, nitric oxide release, and interactions with estradiol, Pharmacogenetics, doi:10.1097/00008571-200207000-00008
Wang, Wang, Endothelial nitric oxide synthase gene sequence variations and vascular disease, Mol. Genet. Metab, doi:10.1006/mgme.2000.3033
Xu, Ilyas, Weng, Endothelial dysfunction in COVID-19: An overview of evidence, biomarkers, mechanisms and potential therapies, Acta Pharmacol. Sin, doi:10.1038/s41401-022-00998-0
Yanamandra, Boggs, Thurmon, Lewis, Bocchini et al., Novel allele of the endothelial nitric oxide synthase gene polymorphism in Caucasian asthmatics, Biochem. Biophys. Res. Commun, doi:10.1016/j.bbrc.2005.07.108
Özkan, Günay, Sener, Karcıoglu, Tahtasakal et al., Variants in TNF and NOS3 (NOS3) genes associated with sepsis in adult patients, J. Gene Med, doi:10.1002/jgm.3323
˙ilhan, Ateş, ˙ilhan, Kaman, Çeliker, NOS3 Glu298Asp polymorphism and endothelial dysfunction in patients with and without end-stage renal disease, Balkan Med. J, doi:10.5152/balkanmedj.2016.16566
DOI record:
{
"DOI": "10.3390/jcm14061931",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm14061931",
"abstract": "<jats:p>Background/Objectives: To elucidate the factors that contribute to individual variability in the progression of COVID-19, experiments on endothelial nitric oxide synthase polymorphisms have been reported. Nitric oxide synthase (NOS3) is located in the endothelium and is involved in the regulation of inflammation and vascular homeostasis. In this study, we investigated the association between COVID-19 severity and NOS3 G894T and NOS3 27-bp VNTR 4b/a genetic polymorphisms. Methods: Patients with COVID-19 (n = 178) were divided into Group 1 (mild disease) and Group 2 (severe disease) based on oxygen saturation levels in room air (Group 1, SpO2 ≥ 93%, n = 107; and Group 2, SpO2 < 93%, n = 73) and hospitalization requirements. Genotyping was performed using polymerase chain reaction-restriction fragment length polymorphism analysis. Results: Overall, genotype and allele frequencies of the NOS3 genetic polymorphisms were similar across the two study groups (p > 0.05). However, the subgroup analysis showed a notable trend for the 4b/4a allele distribution between Groups 1 and 2. In the younger subgroup of patients (≤50 years old) without chronic obstructive pulmonary disease, Group 2 tended to have a higher frequency of the 4b allele than Group 1 (97.4% vs. 85.4% p = 0.06) and a higher occurrence of 4b/4b genotype (94.7% vs. 74.0%, p = 0.05). Additionally, a rarely observed 4c allele was detected only in two subjects within Group 2 but not in Group 1. Conclusions: These findings suggest a trend of association between COVID-19 severity and NOS3 27-bp VNTR 4b/a genetic polymorphism. Genetic analysis may reveal patient susceptibility to disease, prognosis risk factors, and drug responsiveness.</jats:p>",
"alternative-id": [
"jcm14061931"
],
"author": [
{
"ORCID": "https://orcid.org/0000-0002-5750-1223",
"affiliation": [
{
"name": "Department of Chest Diseases, Faculty of Medicine, Hacettepe University, Ankara 06230, Türkiye"
}
],
"authenticated-orcid": false,
"family": "İdikut",
"given": "Aytekin",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Pharmacology, Faculty of Medicine, Hacettepe University, Ankara 06230, Türkiye"
}
],
"family": "Değer",
"given": "İlter",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Chest Diseases, Faculty of Medicine, Hacettepe University, Ankara 06230, Türkiye"
}
],
"family": "Göktaş",
"given": "Gamze",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Bioistatistics, Faculty of Medicine, Hacettepe University, Ankara 06230, Türkiye"
}
],
"family": "Karahan",
"given": "Sevilay",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Chest Diseases, Faculty of Medicine, Hacettepe University, Ankara 06230, Türkiye"
}
],
"family": "Sarınç",
"given": "Sevinç",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-8374-3691",
"affiliation": [
{
"name": "Department of Chest Diseases, Faculty of Medicine, Hacettepe University, Ankara 06230, Türkiye"
}
],
"authenticated-orcid": false,
"family": "Köksal",
"given": "Deniz",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacology, Faculty of Medicine, Hacettepe University, Ankara 06230, Türkiye"
}
],
"family": "Babaoğlu",
"given": "Melih O.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Chest Diseases, Faculty of Medicine, Hacettepe University, Ankara 06230, Türkiye"
}
],
"family": "Babaoğlu",
"given": "Elif",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
3,
13
]
],
"date-time": "2025-03-13T10:53:00Z",
"timestamp": 1741863180000
},
"deposited": {
"date-parts": [
[
2025,
3,
13
]
],
"date-time": "2025-03-13T12:19:59Z",
"timestamp": 1741868399000
},
"indexed": {
"date-parts": [
[
2025,
3,
14
]
],
"date-time": "2025-03-14T04:19:09Z",
"timestamp": 1741925949976,
"version": "3.38.0"
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2025,
3,
13
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2025,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
3,
13
]
],
"date-time": "2025-03-13T00:00:00Z",
"timestamp": 1741824000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/14/6/1931/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1931",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2025,
3,
13
]
]
},
"published-online": {
"date-parts": [
[
2025,
3,
13
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1056/NEJMcp2009575",
"article-title": "Severe COVID-19",
"author": "Berlin",
"doi-asserted-by": "crossref",
"first-page": "2451",
"journal-title": "N. Engl. J. Med.",
"key": "ref_1",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1016/j.jiph.2020.07.014",
"article-title": "COVID-19 and comorbidities: Deleterious impact on infected patients",
"author": "Ejaz",
"doi-asserted-by": "crossref",
"first-page": "1833",
"journal-title": "J. Infect. Public Health",
"key": "ref_2",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1016/j.stem.2020.11.010",
"article-title": "Direct exposure to SARS-CoV-2 and cigarette smoke increases infection severity and alters the stem cell-derived airway repair response",
"author": "Purkayastha",
"doi-asserted-by": "crossref",
"first-page": "869",
"journal-title": "Cell Stem Cell",
"key": "ref_3",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1186/s40246-020-00290-4",
"article-title": "Human genetic factors associated with susceptibility to SARS-CoV-2 infection and COVID-19 disease severity",
"author": "Anastassopoulou",
"doi-asserted-by": "crossref",
"first-page": "40",
"journal-title": "Hum. Genom.",
"key": "ref_4",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2020283",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Severe COVID-19 GWAS Group, Ellinghaus, D., Degenhardt, F., Bujanda, L., Buti, M., Albillos, A., Invernizzi, P., Fernández, J., Prati, D., and Baselli, G. (2020). Genomewide association study of severe COVID-19 with respiratory failure. N. Engl. J. Med., 383, 1522–1534."
},
{
"DOI": "10.3389/fcimb.2022.963239",
"doi-asserted-by": "crossref",
"key": "ref_6",
"unstructured": "Ji, X.S., Chen, B., Ze, B., and Zhou, W.H. (2022). Human genetic basis of severe or critical illness in COVID-19. Front. Cell. Infect. Microbiol., 12."
},
{
"key": "ref_7",
"unstructured": "Delgado-Wicke, P., Fernández de Córdoba-Oñate, S., Roy-Vallejo, E., Alegría-Carrasco, E., Rodríguez-Serrano, D.A., Lamana, A., Montes, N., Nicolao-Gómez, A., Carracedo-Rodríguez, R., and Marcos-Jiménez, A. (2024). Genetic Variants Regulating the Immune Response Improve the Prediction of COVID-19 Severity Provided by Clinical Variables. Sci. Rep., 14."
},
{
"article-title": "Pathogenesis of SARS-CoV-2 and immune response in COVID-19",
"author": "Demirci",
"first-page": "183",
"journal-title": "Turk. Mikrobiyol. Cem. Derg.",
"key": "ref_8",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1016/j.trsl.2021.03.002",
"article-title": "COVID-19 and cytokine storm syndrome: Are there lessons from macrophage activation syndrome?",
"author": "Ombrello",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Transl. Res.",
"key": "ref_9",
"volume": "232",
"year": "2021"
},
{
"DOI": "10.1155/2021/6643333",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Khan, M., Shah, N., Mushtaq, H., and Jehanzeb, V. (2021). Profiling laboratory biomarkers associated with COVID-19 disease progression: A single-center experience. Int. J. Microbiol., 2021."
},
{
"DOI": "10.1080/10408363.2020.1770685",
"article-title": "Biomarkers associated with COVID-19 disease progression",
"author": "Ponti",
"doi-asserted-by": "crossref",
"first-page": "389",
"journal-title": "Crit. Rev. Clin. Lab. Sci.",
"key": "ref_11",
"volume": "57",
"year": "2020"
},
{
"DOI": "10.1111/j.1742-7843.2010.00637.x",
"article-title": "Functional effects of endothelial nitric oxide synthase genetic polymorphisms on haemorheological parameters in healthy human individuals",
"author": "Babaoglu",
"doi-asserted-by": "crossref",
"first-page": "171",
"journal-title": "Basic Clin. Pharmacol. Toxicol.",
"key": "ref_12",
"volume": "108",
"year": "2011"
},
{
"article-title": "Nitric oxide",
"author": "Moncada",
"first-page": "S35",
"journal-title": "J. Hypertens. Suppl.",
"key": "ref_13",
"volume": "12",
"year": "1994"
},
{
"DOI": "10.1002/jgm.3323",
"article-title": "Variants in TNF and NOS3 (NOS3) genes associated with sepsis in adult patients",
"author": "Sener",
"doi-asserted-by": "crossref",
"first-page": "e3323",
"journal-title": "J. Gene Med.",
"key": "ref_14",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1111/j.1476-5381.2010.01196.x",
"article-title": "Therapeutic effect of enhancing endothelial nitric oxide synthase (NOS3) expression and preventing NOS3 uncoupling",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "213",
"journal-title": "Br. J. Pharmacol.",
"key": "ref_15",
"volume": "164",
"year": "2011"
},
{
"DOI": "10.1016/S0163-7258(97)00051-X",
"article-title": "Role of vascular nitric oxide in physiological and pathological conditions",
"doi-asserted-by": "crossref",
"first-page": "111",
"journal-title": "Pharmacol. Ther.",
"key": "ref_16",
"volume": "75",
"year": "1997"
},
{
"DOI": "10.1006/mgme.2000.3033",
"article-title": "Endothelial nitric oxide synthase gene sequence variations and vascular disease",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "241",
"journal-title": "Mol. Genet. Metab.",
"key": "ref_17",
"volume": "70",
"year": "2000"
},
{
"DOI": "10.1111/j.1527-3466.2007.00017.x",
"article-title": "The functional consequence of the Glu298Asp polymorphism of the endothelial nitric oxide synthase gene in young healthy volunteers",
"author": "Godfrey",
"doi-asserted-by": "crossref",
"first-page": "280",
"journal-title": "Cardiovasc. Drug Rev.",
"key": "ref_18",
"volume": "25",
"year": "2007"
},
{
"DOI": "10.5152/balkanmedj.2016.16566",
"article-title": "NOS3 Glu298Asp polymorphism and endothelial dysfunction in patients with and without end-stage renal disease",
"author": "Kaman",
"doi-asserted-by": "crossref",
"first-page": "128",
"journal-title": "Balkan Med. J.",
"key": "ref_19",
"volume": "33",
"year": "2016"
},
{
"DOI": "10.4103/0028-3886.266231",
"article-title": "The correlation of endothelial nitric oxide synthase (NOS3) polymorphism and other risk factors with aneurysmal subarachnoid hemorrhage: A case-control study",
"author": "Konar",
"doi-asserted-by": "crossref",
"first-page": "1006",
"journal-title": "Neurol. India",
"key": "ref_20",
"volume": "67",
"year": "2019"
},
{
"DOI": "10.1155/2014/549747",
"article-title": "Association between NOS3 4b/a polymorphism and the risk of diabetic retinopathy in type 2 diabetes mellitus: A meta-analysis",
"author": "Ma",
"doi-asserted-by": "crossref",
"first-page": "549747",
"journal-title": "J. Diabetes Res.",
"key": "ref_21",
"volume": "2014",
"year": "2014"
},
{
"DOI": "10.1155/2011/419708",
"article-title": "Association of endothelial dysfunction with endothelin, nitric oxide and NOS3 Glu298Asp gene polymorphism in coronary artery disease",
"author": "Saini",
"doi-asserted-by": "crossref",
"first-page": "215",
"journal-title": "Dis. Markers",
"key": "ref_22",
"volume": "31",
"year": "2011"
},
{
"DOI": "10.1186/s12872-021-02192-2",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Shi, J., Liu, S., Guo, Y., Liu, S., Xu, J., Pan, L., Hu, Y., Liu, Y., and Cheng, Y. (2021). Association between NOS3 rs1799983 polymorphism and hypertension: A meta-analysis involving 14,185 cases and 13,407 controls. BMC Cardiovasc. Disord., 21."
},
{
"DOI": "10.1371/journal.pone.0270627",
"doi-asserted-by": "crossref",
"key": "ref_24",
"unstructured": "Dieter, C., Brondani, L.A., Leitão, C.B., Gerchman, F., Lemos, N.E., and Crispim, D. (2022). Genetic Polymorphisms Associated with Susceptibility to COVID-19 Disease and Severity: A Systematic Review and Meta-Analysis. PLoS ONE, 17."
},
{
"DOI": "10.1016/j.genrep.2021.101062",
"article-title": "Mutations and polymorphisms in genes involved in the infections by COVID-19: A Review",
"author": "Kaltoum",
"doi-asserted-by": "crossref",
"first-page": "101062",
"journal-title": "Gene Rep.",
"key": "ref_25",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1016/j.genrep.2023.101814",
"article-title": "The Association of PON1 and NOS3 Genetic Variants with the Severity of COVID-19",
"author": "Eid",
"doi-asserted-by": "crossref",
"first-page": "101814",
"journal-title": "Gene Rep.",
"key": "ref_26",
"volume": "33",
"year": "2023"
},
{
"DOI": "10.1097/00008571-200207000-00008",
"article-title": "Effects of endothelial nitric oxide synthase gene polymorphisms on platelet function, nitric oxide release, and interactions with estradiol",
"author": "Desai",
"doi-asserted-by": "crossref",
"first-page": "407",
"journal-title": "Pharmacogenetics",
"key": "ref_27",
"volume": "12",
"year": "2002"
},
{
"DOI": "10.1038/s41401-022-00998-0",
"article-title": "Endothelial dysfunction in COVID-19: An overview of evidence, biomarkers, mechanisms and potential therapies",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "695",
"journal-title": "Acta Pharmacol. Sin.",
"key": "ref_28",
"volume": "44",
"year": "2023"
},
{
"DOI": "10.1016/j.atherosclerosis.2020.10.014",
"article-title": "Endothelial dysfunction in COVID-19: Current findings and therapeutic implications",
"author": "Haubner",
"doi-asserted-by": "crossref",
"first-page": "58",
"journal-title": "Atherosclerosis",
"key": "ref_29",
"volume": "314",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.04.026",
"article-title": "Imbalanced host response to SARS-CoV-2 drives development of COVID-19",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "1036",
"journal-title": "Cell",
"key": "ref_30",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "ref_31",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.3390/nu14194001",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Ohno, M., and Dzúrová, D. (2022). Body mass index and risk for COVID-19-related hospitalization in adults aged 50 and older in Europe. Nutrients, 14."
},
{
"DOI": "10.1002/jcla.24713",
"article-title": "The importance of using routine laboratory tests in the diagnosis and prognosis of patients with coronavirus disease 2019: Shedding light on clinical laboratory data in COVID-19",
"author": "Khosravi",
"doi-asserted-by": "crossref",
"first-page": "e24713",
"journal-title": "J. Clin. Lab. Anal.",
"key": "ref_33",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.1128/JVI.79.3.1966-1969.2005",
"article-title": "Nitric oxide inhibits the replication cycle of severe acute respiratory syndrome coronavirus",
"author": "Leijon",
"doi-asserted-by": "crossref",
"first-page": "1966",
"journal-title": "J. Virol.",
"key": "ref_34",
"volume": "79",
"year": "2005"
},
{
"DOI": "10.1016/j.arr.2020.101201",
"article-title": "Does NOS3 derived nitric oxide protect the young from severe COVID-19 complications?",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "101201",
"journal-title": "Ageing Res. Rev.",
"key": "ref_35",
"volume": "64",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2019.08.011",
"article-title": "Hallmarks of endothelial cell metabolism in health and disease",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "414",
"journal-title": "Cell Metab.",
"key": "ref_36",
"volume": "30",
"year": "2019"
},
{
"DOI": "10.1378/chest.107.4.1107",
"article-title": "Efficacy of inhaled nitric oxide in patients with severe ARDS",
"author": "Rossaint",
"doi-asserted-by": "crossref",
"first-page": "1107",
"journal-title": "Chest",
"key": "ref_37",
"volume": "107",
"year": "1995"
},
{
"DOI": "10.1002/eji.201646789",
"article-title": "Pathogen interactions with endothelial cells and the induction of innate and adaptive immunity",
"author": "Konradt",
"doi-asserted-by": "crossref",
"first-page": "1607",
"journal-title": "Eur. J. Immunol.",
"key": "ref_38",
"volume": "48",
"year": "2018"
},
{
"DOI": "10.1016/j.cbi.2022.109834",
"doi-asserted-by": "crossref",
"key": "ref_39",
"unstructured": "Papadopoulos, K.I., Sutheesophon, W., and Aw, T.-C. (2022). The influence of renin angiotensin aldosterone system (RAAS), endothelial nitric oxide synthase (NOS3) and erythropoietin (EPO) on COVID-19 complications. Chem. Biol. Interact., 354."
},
{
"DOI": "10.1016/j.gene.2015.09.061",
"article-title": "Endothelial nitric oxide synthase: From biochemistry and gene structure to clinical implications of NOS3 polymorphisms",
"author": "Lacchini",
"doi-asserted-by": "crossref",
"first-page": "584",
"journal-title": "Gene",
"key": "ref_40",
"volume": "575",
"year": "2016"
},
{
"DOI": "10.1097/00003246-200204000-00020",
"article-title": "Increased bone resorption in the critically ill: Association with sepsis and increased nitric oxide production",
"author": "Smith",
"doi-asserted-by": "crossref",
"first-page": "837",
"journal-title": "Crit. Care Med.",
"key": "ref_41",
"volume": "30",
"year": "2002"
},
{
"DOI": "10.1080/17425255.2020.1804857",
"article-title": "Clinically relevant endothelial nitric oxide synthase polymorphisms and their impact on drug response",
"author": "Lacchini",
"doi-asserted-by": "crossref",
"first-page": "927",
"journal-title": "Expert Opin. Drug Metab. Toxicol.",
"key": "ref_42",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1016/j.humimm.2008.03.001",
"article-title": "Intron 4 a/b polymorphism of the endothelial nitric oxide synthase gene is associated with both type 1 and type 2 diabetes in a genetically homogeneous population",
"author": "Galanakis",
"doi-asserted-by": "crossref",
"first-page": "279",
"journal-title": "Hum. Immunol.",
"key": "ref_43",
"volume": "69",
"year": "2008"
},
{
"DOI": "10.1038/ijo.2010.146",
"article-title": "NOS3 haplotype associated with hypertension in obese children and adolescents",
"author": "Belo",
"doi-asserted-by": "crossref",
"first-page": "387",
"journal-title": "Int. J. Obes.",
"key": "ref_44",
"volume": "35",
"year": "2011"
},
{
"DOI": "10.3171/2014.5.JNS131572",
"article-title": "Association of the NOS3 intron-4 VNTR polymorphism with aneurysmal subarachnoid hemorrhage",
"author": "Edsen",
"doi-asserted-by": "crossref",
"first-page": "587",
"journal-title": "J. Neurosurg.",
"key": "ref_45",
"volume": "121",
"year": "2014"
},
{
"DOI": "10.1111/j.1447-0756.2011.01606.x",
"article-title": "Endothelial nitric oxide synthase gene polymorphisms in preeclampsia with or without eclampsia in a Turkish population",
"author": "Ozturk",
"doi-asserted-by": "crossref",
"first-page": "1778",
"journal-title": "J. Obstet. Gynaecol. Res.",
"key": "ref_46",
"volume": "37",
"year": "2011"
},
{
"DOI": "10.1007/s43032-021-00632-0",
"article-title": "Association between endothelial nitric oxide synthase (NOS3) −786 T/C and 27-bp VNTR 4b/a polymorphisms and preeclampsia development",
"author": "Nikolic",
"doi-asserted-by": "crossref",
"first-page": "3529",
"journal-title": "Reprod. Sci.",
"key": "ref_47",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1016/j.bbrc.2005.07.108",
"article-title": "Novel allele of the endothelial nitric oxide synthase gene polymorphism in Caucasian asthmatics",
"author": "Yanamandra",
"doi-asserted-by": "crossref",
"first-page": "545",
"journal-title": "Biochem. Biophys. Res. Commun.",
"key": "ref_48",
"volume": "335",
"year": "2005"
},
{
"DOI": "10.1016/j.trsl.2012.05.004",
"article-title": "Endothelial nitric oxide gene haplotype reduces the effect of a single bout of exercise on the vascular reactivity in healthy subjects",
"author": "Silva",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Transl. Res.",
"key": "ref_49",
"volume": "161",
"year": "2013"
},
{
"DOI": "10.1101/2022.03.02.22271779",
"doi-asserted-by": "crossref",
"key": "ref_50",
"unstructured": "Alshaikh, F.S., Godman, B., Sindi, O.N., Seaton, R.A., and Kurdi, A. (2022). Prevalence of bacterial coinfection and patterns of antibiotics prescribing in patients with COVID-19: A systematic review and meta-analysis. PLoS ONE, 17."
}
],
"reference-count": 50,
"references-count": 50,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/14/6/1931"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Association of Endothelial Nitric Oxide Synthase Polymorphisms with Clinical Severity in Patients with COVID-19",
"type": "journal-article",
"volume": "14"
}